|
| |
Issue no. 28 - March 1987
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 28 -
March 1987
|
DDOnline
Dialogue
on Diarrhoea Online Issue 28 March 1987  Page 1 2
Page 1 2
Time for action
|
Anyone with diarrhoea needs to drink more liquid than they are
losing in the stools.
It is dehydration (loss of water and essential body salts), caused by acute diarrhoea,
that kills. Just two loose, watery stools will begin to cause dehydration, especially in
young children. (This may be even more dangerous if the diarrhoea is accompanied with
vomiting.) That is the time for families to take action, before the dehydration takes hold
and becomes obvious.
|
 |
|
In this issue . . .
- DD questionnaire results
- Early action to prevent dehydration
- deciding on an appropriate home solution
|
DDOnline
Dialogue
on Diarrhoea Online Issue 28 March 1987
 1 Page 2 3 1 Page 2 3
ORT in practice: Egypt The Diarrhoeal Disease Research and Rehydration Centre (DDRRC) at Bab-el-Sha'reya
University Hospital in Cairo has been working 24 hours a day since May 1983. By the end of
1986 we estimated that over 15,000 children had been treated. Widespread promotion of ORT
through the successful national diarrhoeal disease control project (NCDDP) has meant that
mothers start giving ORT early on, at the onset of an episode of diarrhoea. While mothers
still bring packets of ORS with them to the Centre, we have noticed that they stay for
less time - an average of about two hours - than they did, and ORS consumption at the
Centre has decreased. This is because mothers are more confident about giving ORS so they
continue to give the treatment at home once the child has stabilised in the Centre. Even
more important, the degree of dehydration is becoming less severe in children presenting
at the Centre, and the ratio of severe to moderate cases has changed from 1:9.7 in 1983 to
1:16.8 in 1985. It is presumed that this trend will have a great impact on mortality and
long term morbidity. The credit is to the mothers. It is right and natural that the first
person to manage a diarrhoeal episode is the mother, she is concerned and now has the
proper knowledge and tools (ORS and food) to deal with most cases of diarrhoea. I am
afraid that little is left to us! Professor Mahmoud El-Mougi, Professor of Paediatrics, Principal Supervisor, DDRRC,
Cairo, Egypt.
|
Hospital 'Friends' Dr Anne Savage proposes to start a 'League of Friends' for overseas rural hospitals. It
is hoped that the scheme will be able to match up such hospitals with groups or
individuals in the U. K., U.S.A. and Europe, to provide the former with equipment and
medical supplies. Anyone interested, either as a 'Friend' or as a potential recipient
should write to Dr Anne Savage, 12 Turner Close, London NW11 6TU, U. K. It
would be helpful if hospitals or clinics could supply the following details: name,
address, type of hospital (i.e. government, mission), number of beds, type of work
undertaken, whether a charge is made to patients. The name of an organisation which could
provide a reference would be appreciated. Stop press UNICEF's 1987 edition of The State of the World's Children, published by Oxford
University Press is now available from UNICEF, price £4.25, US$ 8.95. Readers should
contact their regional or local UNICEF office. Erratum Apologies to Dr J P Ackers for omitting the 'Dr' from the credit for his article on
amoebiasis in="dd27.htm">DD 27 New ORT film Sonamoni (Golden Pearl) is a colour 16mm film, 34 minutes in length, in Bengali,
available with or without English subtitles. It was produced in Bangladesh in 1986 and is
the third in a series of 'melodrama with a message' films produced in the commercial
entertaining style enjoyed by Bengali audiences. Underlying the story is a message which
promotes the use of oral rehydration therapy for diarrhoea and ways to prevent the
disease. 16mm copies of the film are available from DSR Inc., Box 281, Columbia, MD
21045, USA at US$ 450. All formats of video are available (for purchase or hire). DD translations Translations of DD are available in French, Spanish, Portuguese and Arabic. If
readers would like to receive DD in any of these languages, please write to AHRTAG,
85 Marylebone High Street, London W1M 3DE, U.K. Disease diagnosis The Diagnostic Technology for Community Health (DiaTech) project, funded by USAID,
seeks to develop technologically appropriate assays for diagnosis of infectious diseases
in developing countries, particularly for diarrhoea, acute respiratory infections and
tuberculosis. All proposed studies should have an applied dimension and the potential for
beneficial impact on community or individual health care. Proposals will be considered in
two batches and should be received by DiaTech no later than June 1 or December 1 1987.
Forms and guidelines from: Program Administrator / DiaTech, PATH, 4 Nickerson Street,
Seattle, Washington 98109-1699, U. S. A. ICORT II Proceedings from the Second International Conference on Oral Rehydration Therapy, held
in Washington D.C. in December 1985, and reported in DD 24, are
now available free of charge to DD readers. For copies please write to Robert
Clay, Office of Health, Bureau of Science and Technology, Agency for International
Development, Room 702, SA 18, Washington D.C. 20523, U. S. A.
|
ORT in practice: China While most large hospitals in China have routinely used IV fluids to treat diarrhoea,
it seems that oral rehydration - using salt and sugar solution for diarrhoea - has been
widely used in China for more than 20 years. Recent surveys in five counties found that
over 90 per cent of 'barefoot doctors' use a simple sugar and salt solution. 34 per cent
of mothers also said that they used an oral rehydration solution. Rice water, porridge and
other liquids have also been used for diarrhoea in Chinese traditional medicine. In one
province carrot juice is a traditional treatment for diarrhoea. Although surveys have
revealed high morbidity from diarrhoea in China, mortality figures were found to be very
low. It is thought that early treatment using sugar-salt solution, rice water, porridge
and other traditional fluids is the reason for the low mortality rates. Oral rehydration in China. Carl E Taylor and Zu Zhao Yu, American Journal of Public
Health, 1986 76:187-9.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 28 March 1987
 2 Page 3 4 2 Page 3 4
DD readership survey
The editors would like to thank all readers who filled in and returned the DD questionnaire
sent out with issue 23. One thousand of your replies have been analysed and these have
provided us with many useful ideas for future issues and for improving DD, as well
as much valuable information about the composition of the readership, about how DD is
used, and the impact it has had. It was especially nice to receive so many replies from among the many readers who have
only recently joined our mailing list. Readership profile
The largest proportion of readers is still comprised of doctors, nurses and health
administrators (42, 14 and 10 per cent respectively), but there has been an encouraging
increase in the range of people represented among the readership since our last survey in
1983. Many more village and community health workers, nutritionists, medical auxiliaries,
teachers, now read the Dialogue. It was also interesting to note a significant increase in the percentage of readers who
work in clinics and dispensaries and in training schools. Many respondents share their copy of DD with up to six colleagues. On that basis
we estimate that DD may be reaching well over 250,000 people worldwide in English
alone. Impact of DD Over two thirds of the respondents manage cases of diarrhoea themselves, and a similar
proportion are involved on a day-to-day basis in training and teaching others about
diarrhoea management. It is very encouraging therefore to note from the responses to the
questionnaire that DD has had a significant impact on readers' attitudes and
practices regarding diarrhoea management. 81 per cent have changed their management of
diarrhoea with regard to feeding; 50 per cent their attitudes to medicine prescribing; and
80 per cent the advice they give to patients, as a result of reading DD. Of those
readers who teach others about diarrhoea management, 82 per cent said that DD had
influenced what they teach about rehydration; 46 per cent what they teach about medicine
prescribing; and 73 per cent what they teach about feeding. Content Features in DD which readers have found most useful included information on
management by rehydration; feeding and diarrhoea; news about research and scientific
developments; and the practical advice pages. Requests for features to be included in
future issues also covered a wide range of topics, including nutrition and diarrhoea,
aetiology, use of drugs, feeding and diarrhoea, prevention of diarrhoea, approaches to
treatment, diagnosis, hygiene and sanitation, and health education. Use of DD It was also very clear from the questionnaire results that many readers have reproduced
material from DD, for teaching and training purposes mainly, but also in the media,
for local use, and as reference material for diagnosis and treatment. We were also very
encouraged by the extent to which material from DD has been translated into local
languages. Well over 56 local languages were mentioned by respondents from all parts of
the world. We hope that readers will continue to freely reproduce and translate material
from the newsletter to ensure that the information reaches the widest possible audience
and representatives from other disciplines such as agriculture.
|
Practical evaluation A new manual, Partners in Evaluation: Evaluating Development and Community
Programmes with Participants, by Dr Marie-Therese Feuerstein has been published by
Macmillan.
|
Overlay showing community socio-economic and health
profile for one year
It is a practical handbook, based on extensive field research and the experience of
many people in many parts of the world, designed for those with little formal training in
evaluation methodology who want to monitor and evaluate their own work.
|
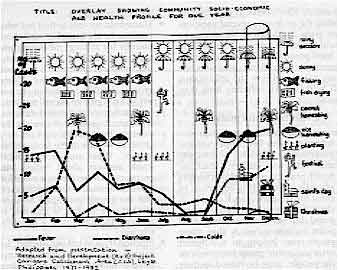 |
Partners in Evaluation is written in clear, straightforward language, contains
many illustrations, and the evaluation methods it describes are appropriate for use in a
wide range of development and community programmes. The manual is available from TALC,
P O Box 49. St Albans, Herts, U. K. Price £3.25 for single copies (including postage
and packing) decreasing on a sliding scale to £2.05 per copy if 20 copies are ordered.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 28 March 1987
 3 Page 4 5 3 Page 4 5
| Choosing an appropriate home fluid |
Oral rehydration in the home
Roger Goodall of UNICEF outlines simple guidelines for
formulating a national strategy for oral therapy. Any strategy or recommendations must be based on an understanding of current customary
approaches to treating diarrhoea - or failing to treat it - in the home. This ensures that
strategies advocated are acceptable to families and communities and avoids confusing or
conflicting messages. When is a solution appropriate? Recommended home available solutions for early oral rehydration therapy the onset of
diarrhoea must be:
- physiologically appropriate - that is contain a digestible starch or glucose and between
30 and 80 mmol/litre of sodium;
- cheap and readily available at all times;
- require the minimum modification of usual preparation methods. The more the solutions
require complicated measuring techniques, the more unlikely they are to be used or
prepared correctly. This is one reason why sugar-salt solutions have often proved
disappointing in uptake;
- culturally acceptable and relevant, for example, in keeping with beliefs about 'hot' and
'cold' illnesses.
Cereal or vegetable based soups, rice congees, lentil dhals, or preparations equivalent
to these examples are likely to be suitable for early home oral rehydration in many
countries. Unfortunately sugar-salt solutions have been promoted as appropriate for home use in
many settings where this is not appropriate - for example, where sugar is either
unavailable or expensive, where resources for training parents are inadequate, and where
no reinforcement of messages concerning continued feeding is undertaken. Continued feeding
Proper case management of diarrhoea consists not only of giving an appropriate home
available fluid (oral rehydration therapy) at the onset of the illness to prevent
dehydration, but also of promoting continued and increased feeding of children and
breastfeeding of infants, both during and after acute diarrhoea, to prevent weight loss
and development of malnutrition. If dehydration does occur
It is essential that parents can recognise when a child has become dehydrated. At this
point it needs oral rehydration salts (ORS) solution to treat the dehydration. Home
prepared solutions are not fully adequate for treatment of actual dehydration and should
only be used where formula ORS is not available. Those children whose condition
deteriorates still further and who are suffering from severe dehydration, or are in shock
and are unable to drink, need to be given rehydration fluids intravenously as a lifesaving
measure which can only be administered by a trained person in a health facility. Every
effort should be made to discourage the unnecessary use of anti-diarrhoeal drugs and
inappropriate antibiotics (except in certain cases of dysentery and in cholera). Roger Goodall, Essential Drugs Adviser, UNICEF, 866 UN Plaza, New York, NY 10017, U.
S. A.
What drinks to give: carrying out a survey
William Cutting describes the steps to take at community
level. To decide what drinks to give requires finding the answers to several questions (see="#page5">page 5). Most of these can be found by health workers with the help of
local people. Always explain to the community why these questions are being asked and how
the information will help children suffering from diarrhoea. Collecting information
Various methods can be used such as:
- Interviews with key people, such as government officials, community and religious
leaders, teachers, health practitioners, opinion leaders amongst women. It is important to
enlist the support of such people. A check list of questions should be prepared before the
interviews. One point to remember is that these people may belong to a different
socio-economic group from most of the people, may be biased in their responses, and may
not give representative answers.
- Household surveys to find out what ingredients are available, and about utensils for
mixing, measuring and storage of the drink. A representative sample of homes, rich and
poor, and covering all ethnic and cultural groups, should be visited or the survey will
not give an overall picture.
- Informal or spontaneous discussions with small groups of people, for example local
health workers, or a group of women at the local well or market. These may produce more
frank answers about beliefs and practices than answering a more formal questionnaire. One
limitation is that the groups may again be unrepresentative and it is difficult to measure
the answers in a quantitative way.
- Practical trials to test out whether, for example, a particular drink is acceptable to
infants and young children with diarrhoea, or if the method of mixing the fluid is easy
and easily remembered. Again it is important to make sure that there is no bias; for
example, getting only the most educated mothers to mix the drink will not indicate how
those who have not been to school will cope with mixing and measuring.
Drawing conclusions
Finally, the answers to all the questions asked will have to be assembled for the
authorities to use as the basis for deciding on the most suitable home rehydration drink
for that area. The method of mixing it must be clear and this message must then be widely
communicated by every possible means. Expert help may be needed to arrive at the decision
and with communication, but ordinary field workers can collect together the necessary
background information without which treating diarrhoea at home will not work effectively. Dr William A M Cutting, Department of Child Life and Health, University of
Edinburgh, 17 Hatton Place, Edinburgh EH9 1UW, U. K.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 28 March 1987
 4 Page 5 6 4 Page 5 6
| WHO decision-making guidelines |
While ORS solution may be used to prevent (as well as treat)
dehydration, it may be more convenient, less costly, and nearly as effective to use other
fluids. An ideal home fluid is safe, effective in preventing dehydration, available,
affordable, easy to prepare and likely to be used. Giving such fluids to children as soon
as diarrhoea starts should prevent most cases from becoming dehydrated. Identify fluids which may be suitable by considering what potentially suitable
food-based fluids are commonly prepared and what containers, measuring devices and
ingredients are widely available. Assess each fluid, to see which best meets the criteria
for an ideal home solution. In countries where differences in culture, availability of
ingredients, or other characteristics exist, separate recommendations may be needed for
different regions. A policy for home therapy can be based on food based fluids, sugar-salt
solution or ORS. Before establishing a policy it may be useful to ask the following
questions. Food based fluids
- Are there commonly prepared cereal gruels, soups or other food based fluids that may be
appropriate for preventing dehydration? What are they? Which are made most frequently in
the home? Which in most parts of the country?
- Which fluids, if any, are already used in times of illness? Are any unsuitable because
of customs that would prevent them being given to young children with diarrhoea? Which
fluids have ingredients that are available throughout the year? Which are the cheapest?
- Which involve boiling? Would the time and fuel needed for cooking make mothers less
likely to prepare the fluid? Which fluids will spoil least quickly?
- Which are most likely to be made with a safe sodium concentration? Which contain a
source of glucose in an appropriate amount?
- If none have a suitable composition made in the traditional manner, would some be
suitable if modified slightly? How difficult would it be to get people to change the
preparation method? Would confusion result from use of two preparation methods - one as a
food, and one as a fluid for treating diarrhoea?
Sugar salt solution
- How expensive is sugar? Is it affordable?
- What measuring utensils and containers of a standard size are commonly available in
homes? What are the difficulties of increasing availability of sugar and appropriate
measuring utensils if they are not already available?
- Can mothers be trained to make and use SSS properly? If so what are the costs? Do the
costs (including regular reinforcing training) exceed the costs of providing sufficient
ORS packets for use in preventing dehydration? Are mothers likely to use SSS as a therapy?
ORS
- How many packets of ORS are, or will be, available in the country? Are supplies
sufficient for use in preventing as well as treating dehydration? What percentage of cases
would be likely to use ORS for prevention if it is the recommended home fluid? Could more
ORS be obtained to allow for its use in preventing dehydration? What would this cost the
programme?
- Where would families be able to obtain ORS packets? What would it cost them? Are they
likely to buy and store it for convenient use?
- Have mothers learnt to correctly mix ORS solution for treating dehydration? What would
be the additional costs of teaching them to use OR solution for preventing as well as
treating dehydration? Are containers for measuring correct amounts of water available in
homes? Could they be made available?
- Would reliance on ORS for home therapy create an undesirable dependence on the health
care system?
|
ADVANTAGES AND DISADVANTAGES OF
POSSIBLE HOME FLUIDS FOR PREVENTING DEHYDRATION |
| TYPE OF FLUID |
ADVANTAGES |
DISADVANTAGES |
| Suitable food-based fluids
commonly prepared in homes |
Variable but safe composition Widely
available
Mothers already know how to prepare
May already be used during diarrhoea
Often involves boiled (sterile) water
Not dependent on a delivery system |
Effectiveness may vary Spoilage
(e.g.from fermentation of gruels) necessitates frequent preparation
May lack 'appeal' as a therapy
May be misunderstood to be a substitute for food
Boiling takes time and consumes fuel |
| Food-based fluids made suitable
with minor modification (such as adding salt or diluting) |
Those listed above. plus: Effectiveness
may be increased
Modification may enhance 'appeal' as a therapy |
Those listed above, plus: May
be difficult to change a current preparation
Composition may vary more. If too much salt is added to the solution it may be
dangerous (can cause hypernatraemia). |
| Salt-sugar solution
(SSS) |
Salt and sugar are often available in
homes Has some of the appeal of a special therapy
Not dependent on a delivery system
No cooking needed |
Requires three accurate measurements Widely
variable and potentially dangerous composition due to inaccurate measurements:
-Too much salt is dangerous (can cause hypernatraemia)
-Too much sugar can lead to osmotic diarrhoea (and consequent hypernatraemia)
Utensils may not be available for measuring correct amounts of salt, sugar, and
water
Sugar may be costly or unavailable
Recipes are difficult to teach, learn, and remember |
| ORS solution |
Easy to prepare, if there is an
appropriate container Requires measurement of only one ingredient,
water. Composition consistently safe unless water is incorrectly measured
No boiling needed
May be less expensive for families than currently used remedies
Will probably prevent dehydration more effectively
Has the appeal of a special therapy |
Container for measuring an appropriate
amount of water may not be available Requires instruction on how to mix
and administer
Must be obtained from a health worker or purchased, thus creating dependence
It will be expensive to provide ORS for every case of diarrhoea
There may not be enough ORS supplies nationally for use in prevention as well as
treatment
In most cases, is unnecessary for prevention of dehydration |
Taken from A decision process for establishing policy on fluids for
home therapy of diarrhoea WHO 1987, WHO/CDD/SER/87.10. Copies of this document are
available from CDD, WHO, 1211 Geneva 27, Switzerland.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 28 March 1987
 5 Page 6 7 5 Page 6 7
Lessons from Africa
Ron Waldman highlights some of the difficulties which
may hinder effective use and acceptance of sugar-salt solution. Since 1982, the African Child Survival Initiative Combatting Childhood Communicable
Diseases (ACSI-CCCD) programme has helped to implement disease control activities in
diarrhoeal diseases; vaccine-preventable diseases; and malaria, in Guinea, Liberia, Ivory
Coast, Togo, Nigeria, Congo, Central African Republic, Zaire, Rwanda, Burundi, Malawi,
Swaziland, and Lesotho. The main focus of the diarrhoeal disease component, in accordance
with WHO strategy, has been on establishing widespread use of oral rehydration salts (ORS)
by health providers in health facilities, together with promotion of continued feeding
during diarrhoea. Home fluids
The use of fluids easily prepared at home is an essential part of the strategy,
especially where death rates from diarrhoeal diseases are high and access to health
services or ORS packets is limited. Because no known home-available solutions in Africa
contain sufficient potassium, these are not as effective or as safe as packet ORS for
treatment of dehydration. However, home-available solutions are usually adequate both to prevent
dehydration from occurring, and to maintain hydration in a child who has been
rehydrated as long as sufficient quantities of fluid are consumed. They are certainly
better than nothing for treating dehydration. valuating sugar-salt solution
The home available solution so far most thoroughly investigated in Africa is sugar-salt
solution (SSS). Where SSS has been promoted, it has been assumed that:
- a culturally acceptable and easy to prepare recipe can be widely disseminated in a way
that ensures correct preparation at home;
- both sugar and salt (sodium-chloride) are readily available to most families:
- these ingredients are cheap enough to be used as a remedy for a frequently occurring
condition; and
- the necessary measuring devices (spoons, cups and containers) are available.
Several countries in the project have carried out surveys to evaluate the effectiveness
of SSS. These have shown that sugar is not always readily available and can be expensive.
Water is sometimes also expensive in terms of time and labour. The word 'spoon' may
sometimes mean only one of several instruments of widely varying size, or there may be no
container to which a single volume of water in the recipe for SSS can be tailored. Where a
standard container does exist. a recipe may have been promoted which calls for a different
sized container. The lessons to be learned are that:
- well-designed research is necessary before a national recipe for SSS can be formulated;
- continuous monitoring should be carried out; and
- promotional messages should be modified as new data becomes available.
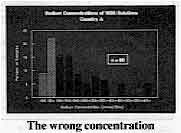
The wrong concentration
|
Table 1. Sodium
Concentrations of SSS Solutions - Country A In one country (A) (see table 1) nearly half the women surveyed prepared SSS containing
more than 150 mmol/litre of sodium (current WHO recommendations suggest a safe range of
between 30 and 80 mmol/litre). Here, promotion of several recipes had undoubtedly
contributed to the variability of SSS preparation.
|
|
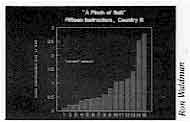 |
Table 2. "A Pinch of Salt" Fifteen Instructors, Country B
In another country (B), instructors being trained at an ORT training centre were asked
to prepare SSS according to the national recipe. The wide range of results shown in Table
2 speak for themselves.
|
In a third country (C), where a major health education effort using carefully prepared
and pre-tested mass media messages had been implemented, a post-campaign evaluation showed
that 54 per cent of women cited recipes with over 100 mmol/litre of sodium, and 12 per
cent with more than 142 mmol/litre. A further study (in country D), where women were trained to prepare SSS in a clinic to
which they had brought their children for treatment of diarrhoea, showed that a third of
solutions collected from their homes a few days later had sodium concentrations above the
recommended level. New strategies
Other studies have found similar results. It would seem sensible to investigate new
strategies for home-prepared solutions. What could these be? First, SSS should not be discarded, at least not until acceptable alternatives are
locally available. While SSS is still being used, improved training and health education
techniques need to be tested, including perhaps the development of a simple colour test
for sodium concentration to provide trainers with instant feedback. Second, if appropriate fluids traditionally used in childhood diarrhoea can be
identified, they should be promoted with particular attention paid to the amount of fluid
administered. Most traditional remedies are given in quantities too small to prevent
dehydration. Third, encourage families to give any available fluid in adequate quantities to prevent
dehydration, while simultaneously teaching them to recognise the signs of dehydration and
when to seek treatment at facilities offering proper case management with ORS packets. Finally, more work is necessary in social marketing and involving the private sector,
especially pharmacists and merchants, to improve access to packaged ORS and to information
about appropriate usage. Dr R Waldman, Centers for Disease Control, Atlanta, GA 30333, U. S. A.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 28 March 1987
 6 Page 7 8 6 Page 7 8
Seawater for OR solution?
I am working in Papua New Guinea in a district that consists of many islands and where
the people mainly live on the coast. In this district few people ever buy salt because
they use seawater to salt their food. Even families living a few kilometres from the sea
collect seawater in bottles to use as salt. Can seawater be used directly along with fresh
water to make up sugar-salt solution for the treatment of diarrhoea? Or is the
concentration of salt in seawater too variable, due to the influence of rain and run off
fresh water, for it to be used directly? If seawater can be used as it is, rather than
first evaporating it to obtain the salt, can you tell me how much seawater should be used
to make up 1 litre of sugar-salt solution? Mary Byfield, Nutritionist, Nisima District, Bwagaoia Health Centre, Division of
Health, P O Box 5, Bwagaoia, Milne Bay Province, Papua New Guinea.
Editors' note: A breakdown of the main constituents of seawater shows that
oceanic water has a concentration of sodium of approximately 458 mmol/litre. This means
that about 200 ml of seawater made up to a litre by adding tap/fresh water would give a
concentration of about 90 mmol/ litre of sodium. However, the concentration of sodium in
seawater can vary considerably depending on dilution by rain, or river water, or following
a tropical storm, or may be more concentrated in shallow pools. Depending on its
concentration it is also possible that seawater may be contaminated with pathogenic
vibrios. We have not seen any data on the use of seawater in making oral rehydration
solution, and would welcome comments from other DD readers.
Acceptance of ORS solution
I have the following comments to make in connection with the letter entitled 'taste and
temperature' from Pakistan, published in DD 26. We
are fully convinced about ORS, and, while an occasional child may show some problems in
accepting ORT, overall acceptance is very good. Flavoured ORS packets are available but
they are very expensive. I wonder whether the problem of excessive intake has been
considered in the case of flavoured ORS*. As regards the availability of ORS packets in remote areas, the government is making
efforts to popularise ORS in every part of the country. A health education campaign has
been started and all media: radio, newspapers, TV are being used to disseminate knowledge
about ORS. The Pakistan Paediatric Association gives due importance to diarrhoea, and
considers it to be one of the major causes of morbidity and mortality in children in
Pakistan. Dr S M Insikar Ali, Assistant Professor of Paediatrics, Secretary General Pakistan
Paediatric Association, Dow Medical College, Karachi, Pakistan.
*Research is required to determine whether flavoured ORS is over-consumed. The editors
would welcome comments from DD readers.
Ready-made solution?
I am presently working in Western Iran in the province of Ilam. The Ministry of Health,
which is providing copies of DD to all doctors concerned, is playing a strong role
in preparing doctors to fight diarrhoea and dehydration. ORS is being promoted in place of
intravenous rehydration and we always prepare the ORS solution in front of the child's
parents and give the solution to the child there and then. This serves not only to
rehydrate the child but also convinces the parents about the dramatic effects of ORT. However, diarrhoea is most prevalent in the rural areas where lack of proper sanitation
facilities and open sewers are major problems and illiteracy makes it extremely difficult
to convince people about the use of ORS in dehydration. Would it not be better to provide
ORS in the form of a prepared solution rather than in packet form, which in my opinion
would be more acceptable to the general public? This is especially important in rural
areas where even safe drinking water is not available. Dr Syed Javeed Zaheer, P 0 Box 69314- 349 Ilam, Islamic Republic of Iran.
Editors' note: Ready-prepared oral rehydration solution is available in some
countries but is usually much more expensive and needs careful storage.
Treating dysentery
Diarrhoea is one of the most common illnesses among children in India, and yet there
are still many misconceptions about its management. Many practitioners use antibiotics
indiscriminately and ORT is used only sparingly for treatment of diarrhoea. Our own
experience with ORT at one of the Oral Rehydration Centres in Bombay has been very
gratifying and we are managing almost all cases of diarrhoea with ORT only. Antibiotics
and other medications are used rarely. I found the article in DD25 about dysentery very
informative but have one query - whether antibiotics and/or metronidazole are necessary
for the treatment of dysentery? Seeing the encouraging results of using ORT in acute
diarrhoeas with watery stools, we decided not to use antibiotics and metronidazole in any
case of dysentery. Our results have been very encouraging and most of the children with
dysentery improved after five to seven days without any antibiotics. Even in the few cases
where drugs were prescribed the children took the same length of time to show an
improvement. But one question we have is, if drugs are not used in dysentery, will chronic
dysentery develop, even though the acute attack may subside within a few days. I would be
very grateful for your comments on this question. Perhaps criteria should be established
for using antibiotics for dysentery cases, especially where it is not possible to
differentiate between amoebic and bacillary dysentery by laboratory examination of stool
specimens. Dr M B Bhagat, 16 Jawahar Nagar, S. V. Road, Goregoan (West), Bombay 400062, India.
Editors' note: We suggest that cases of clinical dysentery (i.e. blood in stool)
be treated with drugs if there is high fever (more than or equal to 101° F) or if the
patient is malnourished. In children, dysentery is usually caused by shigellae, so an
appropriate antibiotic (based on the local antibiotic-sensitivity pattern) should be
chosen. Amoebic dysentery occurs primarily in adults. It requires microscopic examination
of stools for diagnosis before drug therapy is given.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 28 March 1987
 7 Page 8 7 Page 8
Vomiting and ORT
The importance of oral rehydration therapy cannot be overemphasised especially in a
country like Nigeria. I have, however, been coming across the problem of mothers
complaining that their children, especially those under one year of age, usually vomit the
OR solution whenever they are given it, including those suffering from diarrhoea only. The
OR solution is usually prepared by adding ten level teaspoons of sugar and one level
teaspoon of cooking salt to one litre of water. I have been tempted to give parenteral
largactil to stop the vomiting but I need further explanation as to the possible cause of
vomiting immediately after giving ORS. Dr A M Ahmed, Alfijir Clinic, P O Box 2428, Sokoto, Sokoto State, Nigeria
DD asked Dr Norbert Hirschhorn to respond to these questions:
From your description I can suggest several causes of the vomiting, any of which could
occur in any particular child. They are as follows:
- The majority of children brought to a clinic for treatment have already vomited (this is
what usually alarms the mother) and will vomit a few more times in the first hour or two
of treatment. I do not get concerned unless it is over four times an hour.
- Sometimes the solution is given too quickly. One teaspoon (5cc) a minute is actually
quite leisurely (time it for yourself) and usually works to prevent vomiting. One can
space giving the fluid out to 5cc every two minutes. Often the child is thirsty at the
start and demands more, and although vomiting can be alarming, the amount vomited is
usually less than the amount absorbed, so patience helps.
- A sugar-salt solution without bicarbonate will prolong the vomiting as acidosis is
corrected (by the kidneys) a bit more slowly.
- Table sugar, in the amount you use, tends to cause more vomiting (an osmotic effect in
the upper intestine). You could try using seven level teaspoons to one litre of solution.
Mostly I would avoid anti-emetics like largactil as they make children too drowsy to
drink. I find in difficult cases that a slow drip by naso-gastric tube is effective. Dr N Hirschhorn, John Snow Incorporated, 1100 Wilson Boulevard, 9th Floor,
Arlington, VA 22209, U. S. A.
Sorai storage
I have just noticed the report in DD 26 about the
reduction in transmission of cholera if water is stored in a sorai - the narrow-necked
earthenware vessel. I have also just read recently that one problem with storing water in
sorais is that they are very difficult to clean and hence often harbour amoebic dysentery
cysts. It would be useful if DD readers were made aware of this possible problem
with water storage in sorais and similar narrow-necked vessels. Carrie Osborn, 25 Hercules Street, London N7 6AT, U. K.
Diarrhoea in the U. K.
As a medical officer for Environmental Health in the United Kingdom, I have quite a
number of cases of food poisoning and dysentery reported to me. The city of Leeds has a
population of approximately three quarters of a million and in the average year I receive
600 notifications of an illness presenting as diarrhoea. For every case that is officially
notified there are many which are not brought to my attention. I have to express concern that the management of patients with diarrhoeal illness
appears to be better conducted in Bangladesh than it is in the U.K. Many patients are
advised to stop eating and quite a number go on to a very restricted amount of fluids.
Advice is frequently given to cut things out of the diet with no indication of when the
normal eating pattern should be resumed. Lack of understanding about the gastro-colic
reflex which produces bowel motions when food is taken, particularly after a period of
starvation, is common. Diarrhoeal illness accounts for quite a number of lost school days in children and lost
work days in adults in a city this size. We urgently need to find ways of communicating
good practices learnt in developing countries to the U.K. Dr Martin Schweiger, Specialist in Community Medicine, Leeds Eastern Health
Authority, Meanwood Park Hospital, Tongue Lane, Leeds LS6 4QD, U.K.
Editors' note: DD 29 will focus on the
important role and influence of doctors in diarrhoea case management in both developed and
developing countries. The editors would welcome comments from readers for publication in DD.
Using a nasogastric tube
I would like to comment on the article by Christine Candy on 'Using a nasogastric tube'
in="dd26.htm">issue 26. Is it really necessary to include mothers' saliva as a
lubricant when water can do the job well? Are there other advantages that are not stated?
Please clarify. Mrs Modupe Ojo, Paediatric Nurse Practitioner, Institute of Child Health and Primary
Care, College of Medicine, Idi-Araba, Lagos, Nigeria.
Christine Candy has made the following comments: I suggested using maternal
saliva for use under field (e.g. emergency famine relief) conditions as an alternative to
water. The glycoprotein content of saliva is similar to a water soluble lubricant such as
K-Y jelly; it is also possible that maternal saliva would contain fewer enteropathogens
than a heavily contaminated water supply.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Editor Kathy Attawell
Editorial assistant Maria Spyrou Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), ODA (UK), UNICEF, WHO
|
Issue no. 28 March 1987
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
updated: 23 August, 2019
|