|
| |
Issue no. 48 - March 1992
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
updated: 23 April, 2014
Pages 1-8 Dialogue on Diarrhoea Online Issue 48 -
March 1992
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 48 March 1992
 Page 1 2
Page 1 2
Best of both worlds
Over 3,000 years ago, practitioners of the Ayurvedic system of traditional medicine in
India were recommending that people with cholera be given quantities of a drink made by
dissolving rock salt and molasses in tepid water. This sounds very like a form of ORT,
developed only this century to prevent and treat dehydration due to diarrhoea. Doubtless
there may be other beneficial treatments in traditional medicine. Despite this, it is wise to be extremely cautious. Traditional remedies can be
dangerous and few have been scientifically tested. Similarly, any integration of healers
into health care services requires careful control and supervision. This issue of DDexplores aspects of traditional healing, a topic that is often raised in letters
from readers.
|
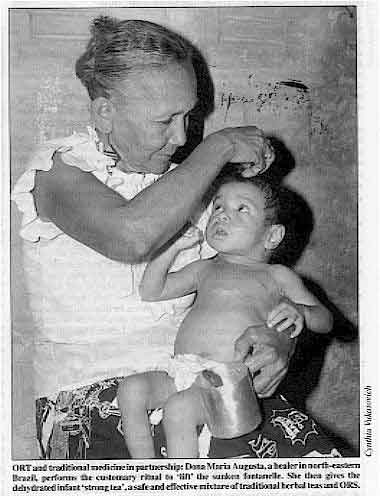
ORT and
traditional medicine in partnership: Dona Maria Augusta, a healer in north-eastern Brazil,
performs the customary ritual to 'lift' the sunken fontanelle. She then gives the
dehydrated infant 'strong tea', a safe and effective mixture of traditional herbal teas
and ORS.
The photo shows a child with diarrhoea being cared for by a traditional healer. The
healer knows that a sunken fontanelle is a sign of dangerous dehydration. She is laying
her hand on the child's head as part of a traditional treatment to 'lift' the fontanelle.
But she is holding in her other hand a cup which contains oral rehydration solution (ORS)
mixed with a herbal tea to give to the child, who is obviously recovering well.
|
 |
Ideal way forward?
Conflict and competition between modern and traditional health care systems within
communities can waste valuable resources and hold back vital progress. We are increasingly
realising the complex nature of health needs and the extent to which people use both
modern and traditional systems (see pages="#page2">2,="#page3">3
and 4). Surely the best from both systems ought to be tapped to meet
these needs. The kind of happy compromise illustrated here could be the ideal way forward
for the future in many societies.
|
In this issue:
- Decisions about diarrhoea: understanding people's treatment choices
- Traditional healers - potential for collaboration?
- Update on viral diarrhoeas
- Special supplement on persistent diarrhoea
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 48 March 1992
 1 Page 2 3 1 Page 2 3
When do people seek help
. . . and from whom? Understanding the reasons why and when families seek, or do not seek, help for
children with diarrhoea, can help health workers to make education messages and health
services more relevant and effective. Successful community based programmes depend on families knowing how to manage
diarrhoea at home with fluids and food, and recognising when children need treatment by a
health worker. Families often try different approaches - both modern and traditional - to
treating childhood diarrhoea. Choice of approach depends on the type of diarrhoea, what is seen as its cause, and the
availability of health care. When and where families seek help is called 'health seeking
behaviour'. The choices can include:
- home care without drugs;
- home care after asking the advice of a relative or neighbour;
- home medication with purchased drugs or home treatment using traditional remedies;
- visiting a traditional healer;
- seeking advice and/or prescribed treatment from a pharmacist;
- seeking advice and/or prescribed treatment from a health worker in government or private
practice.
To improve health, programmes often try to increase access to modern medical care. But the fact that a clinic or hospital is there does not necessarily mean that people
will use it or accept it. Many will continue to use traditional healers and remedies.
Numerous factors affect when and where families seek help, and why they may not use
modern health services. These include:
- availability e. g. distance from a hospital or health centre, or times
when health workers are on duty;
- affordability e. g. the cost of a consultation or medicines, or the
'cost ' of time required to travel to a health centre;
- acceptability e. g. the level of confidence of a family or community in
a health worker's diagnosis or advice.
Influence of beliefs
Cultural beliefs and attitudes especially affect how a family perceives a child's
illness, the health care and treatment options available to them, and what they decide
about where and when to seek help. Many societies have their own classification systems for illnesses. Diarrhoea, for
example, may not always be described as a single disease. Different types of diarrhoea can
have local names and there may be local beliefs about symptoms, causes and treatments of
the illness. Families may seek treatment for some types of childhood diarrhoea and not for
others, depending on how serious they think the illness is. When a child becomes ill, a family may seek advice from several sources and try a
variety of treatments. The first step is usually home medication, based on local beliefs
about the illness and the advice of family, friends and neighbours. Only later will they
visit a traditional healer, or a pharmacist or physician. People often visit a traditional
healer before taking a sick child to a health centre or hospital.
|
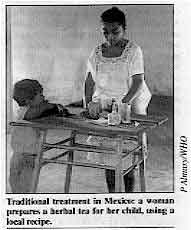
Traditional treatment in Mexico: a woman prepares a herbal tea
for her child, using a local recipe.
Families accept the diagnosis and advice that make the most sense. If there is a big
difference in cultural background and educational status between the community and the
health worker, people may not understand (and therefore not follow) advice, so the
treatment may not seem to 'work'. If advice does not make sense to them or the treatment
does not appear to work, they will usually try another source of health care.
|
 |
|
Checklist of questions for health workers Health workers need to find out what local people believe and what action they take
when a child has diarrhoea.
- What are the different names for diarrhoea?
- Do different names mean different types of diarrhoea?
- What do people believe are the causes of these different types of diarrhoea?
- What do people believe about giving food and drinks during diarrhoea? Do they think they
should give:
- extra water or other fluids
- breastmilk
- ordinary foods
- special foods
- Where do people go to seek help?
- What treatments are sold or prescribed by local health providers?
- In the treatment of diarrhoea, what do people believe about the use of:
- local herbs and remedies
- medicines
- pills
- injections
- intravenous drips
- Do people know about ORS? What do they think it is? Do they use it?
|
Dr Patricia Paredes, Instituto de Investigacion Nutritional,
AP18-0191, Lima 18, Peru.
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 48 March 1992
 2 Page 3 4 2 Page 3 4
Mexico
A group of mothers in the central highland region of Mexico were asked how they decided
about the severity of diarrhoea and whether their child was getting better or worse. For
them the most important signs were changes in the child's behaviour which interfered with
household activities, such as crying or restlessness. They also took notice of signs
associated with the eyes, and changes in the frequency and appearance of the stools. Most treated diarrhoea with a combination of home remedies and modern medicine. Only 5
per cent said they visited a traditional healer, although herbal teas (made from
more than 12 different herbs), and rice water were commonly given as home remedies. Just
over half of the mothers gave an over-the-counter drug, usually an antibiotic, aspirin, or
a mixture of kaolin and pectin, bought from the local community store or a pharmacy. Only
10 per cent of the mothers used oral rehydration therapy. A third of the mothers took the child to a doctor, either because of vomiting or
persistent diarrhoea. Modern medicine appeals to them because it is used by 'high-status'
people and has scientific authority. Doctors, however, are thought to be cold and aloof,
and people do not always understand what they have to offer. All mothers who went to a
physician continued to use home remedies along with the medicine prescribed. Martinez, H, and Saucedo, G, 1991. Mothers' perceptions about childhood
diarrhoea in rural Mexico. .I. Diar: Dis. Res. 9 no 3:235-243. Thailand
In central Thailand, people use both modern drugs and traditional remedies to treat
childhood diarrhoea. In one study, half of those asked had taken advice from a herbalist.
Modern drugs were widely and inappropriately used for the treatment of diarrhoea, whereas
oral rehydration therapy was only used in about half of cases. Poorer people mostly bought
medicines from local grocery stores. Most people, when asked, did not know anything about the modern medicines they gave
their children, but believed them to be good, particularly those given by injection. Choprapawon, C, et al., 1991. Cultural study of diarrhoeal illness in central
Thailand and its practical implications. J. Diar: Dis. Res. 9 no 3: 204-212. Peru
In a poor area of Lima, the capital city of Peru, we looked at how families chose
treatment for children with diarrhoea. Families sought help outside the home when a child
had signs and symptoms thought to be serious and based on folk beliefs about different
types of diarrhoea. Different treatments were tried as new symptoms appeared during the
course of the illness.
- More than half of the 168 children were given traditional fluids on the first day of
diarrhoea. These included strong teas, herbal teas, and panetela, a weak gruel of
toasted rice, bread and sugar. Over 80 per cent were given such fluids at some point
during the illness.
- Modern drugs were the second most common treatment used. These included
anti-diarrhoeals, antibiotics, or antiemetics - often the remainders of unused
prescriptions from a previous illness in the family. A combination of chloramphenicol and
tetracycline, known as Quemiciclina, used in a single dose, was particularly popular. A
third of these children with diarrhoea were given this drug.
Traditional medicine Traditional medicine is a term used to describe health care that does not fall
within the allopathic 'modern and scientific' health care system. Traditional health care
varies greatly from one country to another and covers a wide range of practices. It includes .systems of medicine with a definite body of knowledge which is written
down and taught formally, for example, traditional Chinese and Tibetan medicine, and
Ayurvedic and Unani systems in India. It also includes 'folk' healers, such as herbalists
and spiritualists, who learn from an older member of the family or special teacher: There are also many traditional 'home' remedies made using recipes that have been
learnt from older relatives.
|
When is outside help sought?
Symptoms which caused the family to seek outside help, from a modern practitioner or a
traditional healer (known as a curioso), included vomiting, listlessness or loss of
appetite. But the duration of diarrhoea was the most important factor - the longer the
diarrhoea continued, the more likely it was that the family took the child to a doctor or
traditional healer.
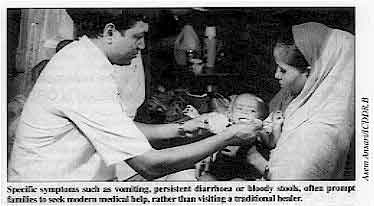 |
Specific symptoms such as vomiting, persistent diarrhoea or
bloody stools, often prompt families to seek modern medical help, rather than visiting a
traditional healer.
The choice of modern or traditional healer depended on the way in which the family
perceived and described a diarrhoeal illness. Children with blood in the stools or who
passed many stools were more likely to be taken to a modern health facility. Those with
fever were more likely to be taken to a traditional healer.
|
Cases thought to be due to some mystical cause were treated with a traditional healing
method. In contrast, cases described in bio-medical terms (such as infection and
diarrhoea) were more likely to be taken to a modern health facility. Families often used
both systems and were willing to try any and all options to treat their child's illness. Dr Nancy E Levine, Associate Professor of Anthropology, University of California,
Los Angeles, California, USA and Dr Patricia Paredes, Medical Researcher, Instituto de
Investigation Nutritional, Lima, Peru.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 48 March 1992
 3 Page 4 5 3 Page 4 5
| Why families choose traditional remedies |
"We tell mothers to use ORS
and they don't" Carol MacCormack explains why mothers in Jamaica use
traditional remedies for diarrhoea instead of ORS advised by health workers. In Jamaica ORS has been carefully promoted through the health service. Sick children
are seen by a health worker, a packet of ORS is given to the mother, its use explained,
and the mother shown, in the clinic, how to give the solution with a cup and spoon. Health
talks from nurses included the message never to use traditional remedies and only to use
ORS packets. We talked with 263 mothers who had brought children with diarrhoea to
out-patient clinics. Most mothers had heard the ORS message before - on the radio,
television, or from health workers. What mothers do
Diarrhoea symptoms that caused mothers to treat their children included frequent
stools, vomiting, fever and stools which were watery or contained mucus. Very few mothers prepared an ORS solution and gave it to their child. Mostly they gave
traditional remedies. The most common remedies used were coconut water, other fruit juice
or fruit syrup and water, black mint or spearmint tea with sugar, and other sweet 'teas'.
A few gave glucose and water (without salt). When asked what fluids they gave, 3 per cent
of mothers said breastmilk, and 1 per cent, bottlemilk. When asked, 'What does your child like
to drink when he or she has diarrhoea?', most said breastmilk and none said oral
rehydration solution. A second category of traditional remedies was porridges made with
wheat flour, corn meal, arrowroot or banana, flavoured with salt and sweetened with sugar.
A few mothers gave other remedies and over-the-counter drugs, usually laxatives and 'salt
water'. Familiar and less costly
Most of the traditional drinks mentioned are helpful for preventing dehydration. They
were used because they were familiar, easily made or obtained and the child liked them.
Traditional home remedies were also seen to be less costly. It took the best part of a day
to travel to and from a clinic, wait to be seen, and rehydrate the child in the clinic
with a cup and spoon. Mothers went home with only one packet of ORS. The 'cost' of that
packet was a day's time, travel expenses, lost wages, and food for snacks while travelling
and waiting. Mothers could not buy packets of ORS from a nearby pharmacy because they are
not for sale. This meant that, wrongly, some bought laxative salts, done up in little
packets, as a substitute for ORS 'salts'.
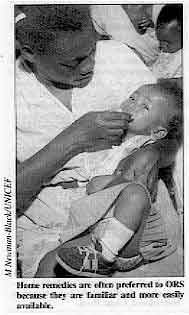 |
Home remedies are often preferred to ORS because they are
familiar and more easily available. Both health workers and mothers wanted to do their best for the children. But because
ORS packets were not sold commercially, and health workers warned mothers never to use
traditional remedies, fearing some to be dangerous, children often did not receive either
ORS or sufficient home fluids to prevent dehydration.
|
Carol MacCormack, Bryn Mawr College, Bryn Mawr, Pennsylvania 19010, USA. Healers and health services:
working together?
DD reports on recent studies and highlights some key issues. In many cultures, and for a variety of reasons, families often turn first to
traditional healers for advice when a child has diarrhoea. It would seem sensible to try
to ensure that healers give the right advice about fluids and feeding, and that harmful
practices are discouraged.
|
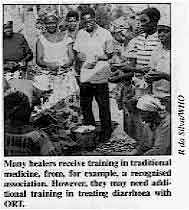
Many healers receive training in traditional medicine, from,
for example, a recognised association. However, they may need additional training in
treating diarrhoea with ORT. The potential for collaboration between the traditional and modern medical systems is
being explored in some countries. Researchers have looked at how traditional healers treat
diarrhoea and dehydration, and have tried to assess the extent to which it is possible to
incorporate ORT into their practices.
|
 |
Zambia: advantages and disadvantages
Recognising the important role of traditional healers, the Ministry of Health in Zambia
created a Department of Traditional Medicine, and supported the setting up of a
traditional practitioners' association. A survey by the national CDD programme identified
three groups: herbalists, spiritualists and faith healers. Most were aware of the commonly recognised causes of diarrhoea, including bad food,
poor hygiene and contaminated water. The usual treatment consisted of drinks of roots or
herbs mixed with water; in some cases, porridge was recommended. Most healers could
recognise the signs of dehydration and 79 per cent said they would be willing to advise
giving oral rehydration therapy. The majority of traditional healers were keen to learn about ORS, but an intensive
training effort would be required to overcome problems such as overdosing with toxic
herbal mixtures, and advising mothers to stop breastfeeding. Dr Paul J Freund, PRITECH, PO Box 37580, Lusaka, Zambia. Continued on next page
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 48 March 1992
 4 Page 5 6 4 Page 5 6
| Traditional healers and remedies |
Brazil: the ORT 'ritual' In north-eastern Brazil, diarrhoea is a serious child health problem. Families consult
a wide variety of traditional practitioners, as well as village health workers, nurses and
physicians. The variety of healers and therapies often results in mixed messages,
incomplete care and the child's eventual death. But 'modern' medicine is not always an
option, due to problems in health care delivery, and people continue to turn to the
traditional sector. In one study, it was found that 83 per cent of rural mothers first seek help from
traditional healers if their children have diarrhoea. Almost all urban mothers taking
their children to a rehydration centre for intravenous rehydration had already consulted a
healer. Diarrhoea is perceived by many parents as a variety of folk maladies - evil eye,
fright disease, spirit intrusion, intestinal heat, or sunken fontanelle - and traditional
healers are believed to have the spiritual power to cure a sick child. Realising that many families seek help from traditional healers, the primary health
care programme (PROAIS) at the Federal University of Ceara worked with them to deliver
ORT. Together, healers and researchers developed an ORS-tea which combines traditional
herbal anti-diarrhoeal teas with the correct mixture of salt and sugar, using a simple
bottle-cap measure. Teaching materials on the prevention and treatment of diarrhoeal
diseases were developed based on local beliefs about childhood illness, to be easily
understood by non-literate mothers. Healers integrate ORT into their customary rituals for
treating evil eye or a sunken fontanelle (as shown in the="#page1">picture on page
1). Intensive training of 400 traditional healers was shown to increase the number of
mothers using ORT, alter a number of dangerous health care practices, and reinforce
preventive behaviours to stop diarrhoeal disease transmission. Infant mortality was
significantly reduced, compared with control communities where healers were not
mobilised.
Introducing ORT in this way worked because it did not try to alter popular medical customs
and beliefs, but built on them instead. Dr Marilyn K Nations, Rua dos Tabajaras 575/700, Fortaleza, Ceara, Brazil. Cameroon: interest in oral rehydration therapy Fifty traditional healers in the Cameroon were asked how they treat diarrhoeal
diseases. The healers were either herbalists, priests or diviners. Five different
organisations of traditional healers were active in the four regions visited, and most
were registered with the government. But not all healers belong to an association and they
do not have to be registered to practise. Those interviewed divided diarrhoeal diseases into two groups: those where a specific
cause cannot be determined, and those with a specific cause. Treatments included harmful
practices (65 per cent said they gave purging remedies) and beneficial ones (26 per cent
began by giving something to drink).
 |
Research is needed to find out whether traditional remedies are
safe, and effective for treating diarrhoea. Only a few had heard of or used oral rehydration therapy, and none knew how to make an
oral rehydration solution correctly or gave it in large enough quantities to be effective.
But, when the purpose of ORT was explained, the healers expressed great interest in using
it. Most had a favourable view of the role of modern medicine, except where the cause of
illness was believed to be "super-natural'. Patients were often treated
simultaneously by traditional and modern healers, and it is not unusual for healers to
send a remedy to a patient in hospital. Physicians also seemed impressed by the conviction
of health workers and patients that traditional medicine is effective.
|
Referrals took place between hospitals and healers, and between one healer and another.
The main issue, which is not easy to address, is that of how to organise collaboration. Flavien Ndonko, PRITECH/USAID, Rue Nachtigal, BP 817, Yaoundé, Cameroon. Uganda: first source of health care Nearly 300 traditional healers in Uganda were asked how they treated diarrhoea and what
they believed to be the causes. The healers saw many cases of diarrhoea, and their beliefs
about the causes mostly coincided with modern medicine - including poor sanitation,
unclean water, and eating contaminated foods. They used a great variety of herbs and plants, given with varying amounts of water, to
treat diarrhoea. Twenty five per cent considered extra fluids to be necessary, and almost
three quarters advised patients to take as much fluid as possible, including water, milk,
fruit juices, porridge, tea, sugar and salt solutions. A few. however, advised restricted
fluid and food intake. Many healers recognised their limitations and, if the diarrhoea had
not subsided after 1 to 3 days, advised patients to seek treatment at a hospital. These traditional healers provide the first source of health advice and treatment to
most people in rural areas. Since they live with the people and share their customs and
traditions they might have the potential to increase use of oral rehydration therapy,
given careful training to improve their existing techniques. Anokbonggo W et al., 1990. Traditional methods in management of diarrhoeal diseases
in Uganda. WHO Bull. vol68, no 3: 359-363. Continued on next page
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 48 March 1992
 5 Page 6 7 5 Page 6 7
| Traditional healers and remedies |
Issues to consider Some of the advantages and disadvantages of involving traditional healers in the
promotion of oral rehydration therapy are: Advantages
- Traditional healers are often the first providers of health care for many families in
both rural and urban areas.
- Traditional healers are present in far greater numbers than modern medical personnel in
many countries.
- Traditional healers are already treating many cases of diarrhoea.
- The cost of providing ORS and training for traditional healers might be lower than
training costs for medical staff.
- Traditional healers work in the community and are familiar with what people think about
illness and the attitudes of mothers. Promotion of ORT may be more readily accepted from
traditional healers.
Disadvantages
- Traditional healers are not always organised and may be hard to reach with training
programmes; targeting and selecting healers may be difficult and not all are motivated to
collaborate.
- There is still mistrust of traditional medicine by the medical establishment and of
doctors by healers.
- The problem of overdosing and use of potentially dangerous and toxic substances in young
children in particular is a serious issue.
- There are harmful practices, such as purging (which need to be discouraged).
- If traditional healers do not treat diarrhoea correctly, children may develop more
serious dehydration and be taken too late to clinics.
- There may be inappropriate adaptation of treatments - for example not giving enough
fluid to combat dehydration.
|
Problems with purging practices Use of enemas and purgatives has been recorded in many parts of the world, but the
extent is not well documented. Jemima Hayfron-Benjamin writes
from Ghana and warns of the dangers. Taking an enema is common in Ghana. Elderly people, pregnant women, children and the
sick are given enemas regularly, especially in rural areas where there are inadequate
health services, and in urban slums. It is a traditional technique, culturally accepted
and popular, and is often the first treatment at home for fever, cough, constipation,
flatulence, diarrhoea and pain. Enemas are used in medicine to clean the bowel before surgery or during labour, and to
stimulate bowel motility after surgery. The practice of giving enemas and purging with
strong herbs and other substances can be very harmful, especially in young children. If
the active ingredients are toxic or corrosive, these can damage the intestines, leading to
ulceration, perforation, peritonitis, septicaemia and even death. I have seen many children who have collapsed after being given enemas containing a
range of concoctions from cassava and ginger to remedies from traditional healers. For example, an 8 year old girl presented with acute abdominal pain. The mother said
her daughter had been feeling ill for a few weeks, with abdominal pains, loss of appetite,
vomiting, severe weight loss and diarrhoea, so the mother gave her enemas from time to
time. After the last enema. she noticed her daughter's condition was deteriorating and
rushed her to hospital. The girl was pale looking, dehydrated and emaciated, feeling
thirsty, vomiting occasionally and feverish. We diagnosed typhoid fever with a perforated bowel following an enema, peritonitis and
septicaemia. Because of the seriousness of the condition, she was rushed to theatre for an
emergency laparotomy. Fortunately the child survived. In another instance, a 9 month old baby girl was brought to us unconscious, with
rolling eyeballs, signs of pulmonary oedema, early cardiac failure, severe anaemia and
twitching. The child had diarrhoea two days before and was given an enema that morning.
Afterwards the child collapsed and was rushed to hospital where she died an hour later
from acute cardiac failure and cerebral oedema caused by poisoning from the enema. Unanswered questions Giving enemas to children is widely practised, but we do not know enough about the
problems this may cause. Unanswered questions include:
- When and why do families give enemas to their children?
- Are they aware that enemas may be dangerous?
- Which substances are used for purging and which of these are toxic, and in what
concentrations?
- To what extent do enemas contribute to mortality in small children?
- How can this traditional practice be made safer or discouraged?
'Modern' enemas: toxic chemicals In South Africa some traditional healers were found to have caused harm to patients by
'modernising' their use of purgative enemas. Whereas enemas traditionally consisted of
plant extracts, given through a truncated cow horn or hollow reeds, these have been
replaced by domestic and industrial chemicals given with syringes or through rubber
tubing. Some of these chemicals are toxic, and can cause severe damage to the bowel. Dunn, J P et al., 1991. Colonic complications after toxic tribal enemas. Br.
J. Surg. 78: 545-48.
|
Dr Jemima Hayfron-Benjamin, Central Hospital, PO Box 174, Cape Coast,
Ghana. DD would be interested to hear from readers about this subject.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 48 March 1992
 6 Page 7 8 6 Page 7 8
Developments in diagnosis and vaccines
Viral infections account for over a quarter of severe childhood diarrhoeal
episodes in developing countries. Ruth Bishop discusses the
importance of different viruses and reports on recent progress in rotavirus vaccine
development. Viruses are an important cause of diarrhoea in young children. More than 50 per cent of
diarrhoea in children admitted to hospital in industrialised countries is associated with
viruses infecting the intestinal tract. Bacterial enteric infections are more common in
children in developing countries, so the proportion of severe diarrhoea due to viruses is
less, approximately 25 to 30 per cent, but is still important. Rotaviruses Rotaviruses are the single most important infectious cause of severe acute diarrhoea in
young children throughout the world. The CDD programme at WHO considers development of a
vaccine to prevent rotavirus infection to be a priority. Field trials of vaccines have been held in Europe, USA, South America, Africa and Asia.
The trials have used animal rotaviruses (from calves or young monkeys) that are very
similar to human rotaviruses.
 |
Rotavirus particles in diarrhoeal faeces, as seen using an
electron microscope.
These animal rotaviruses are grown in cell culture and are given orally as live
viruses. They seem to grow in the human intestine and produce serum antibodies without
causing disease. The monkey rotaviruses have occasionally caused mild fever, but are
considered safe for children.
|
Initially the effects of the vaccines were studied mainly in children aged 6 to 18
months. But the importance of early vaccination has now been realised, and most vaccine
trials now involve infants aged 3 to 4 months. In breastfed infants there may be some
interference with vaccine 'take' from high levels of maternal antibody in breastmilk, but
this might be overcome by giving more than one dose of the vaccine, perhaps at monthly
intervals. In trials to date, the vaccines have performed best in children in Europe and
the USA, where efficacy rates up to 70 to 80 per cent have been seen. There are four main rotavirus serotypes. To be effective, a vaccine must be able to
protect against disease caused by each serotype. One approach is to develop a combined
vaccine that contains all four serotypes. These combined vaccines have been shown to be
safe, and a major trial of the effectiveness of one mixture will start soon in Venezuela. The rotavirus vaccines tested so far are not suitable for release by their
manufacturers because of their limited efficacy. If the trial in Venezuela is successful,
it is possible that this vaccine could be made available for more widespread use by 1994.
It is hoped that a rotavirus vaccine could be combined with oral polio vaccine, without
decreasing the 'take' of either vaccine. There is preliminary evidence that the oral
rotavirus vaccines tested so far do not interfere with the effectiveness of oral polio
virus vaccine when given in combination. If this proves to be correct, then it is probable
that oral rotavirus vaccines could be incorporated in the EPI schedule. Researchers are also trying other approaches to the production of rotavirus vaccine.
These include attenuated human virus, and production of genetically engineered vaccines.
All strategies have focused on development of oral vaccines as it is thought that
parenteral vaccines are less likely to be effective. Enteric adenoviruses Adenoviruses of serotypes 40 and 41 have been shown to cause severe acute diarrhoea in
6 to 8 per cent of young children admitted to hospital in developed countries. The
diarrhoea is generally of longer duration than that caused by rotaviruses. Enteric
adenoviruses also cause severe diarrhoea in young children in developing countries, but
their importance seems to vary from country to country, and further studies are needed to
see whether they are involved in chronic illness and development of malnutrition.
|
Adenovirus particles in diarrhoeal faeces. Diagnosis by
electron microscopy is no longer necessary, as special chemical tests have been developed.
Diagnosis of infection by electron microscopy is no longer necessary; sensitive and
specific ELISA assays are now available.
|
 |
'Small' viruses These include astroviruses, caliciviruses, Norwalk viruses and others. It seems likely
that infection due to a number of different small viruses could explain many diarrhoea
episodes from which no pathogen is isolated. Several 'small' viruses have been shown to
cause epidemics of food-borne or water-borne diarrhoea and may prove to be important in
developing countries. Recently some laboratories have developed specific ELISA assays for
these viruses, and it may soon become possible for laboratories in developing countries to
find out how important these viruses are as a cause of severe disease in young children. Professor Ruth Bishop, Department of Gastroenterology, Royal Children's Hospital,
Parkville, Melbourne, Victoria 3052, Australia. Barnes, G L, 1991. Intestinal viral infections. in: Paediatric Gastrointestinal
Disease, ed Walker WA et al., B C Decker lnc, Philadelphia, pp538-546. Cook, S M et al., 1990. Global seasonality of rotavirus infections. Bull WHO 68:
171-177. Madeley; C R. 1986. The emerging role of adenoviruses as inducers of
gastroenteritis. Paed. Infect. Dis. 5: 563-574.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 48 March 1992
 7 Page 8 7 Page 8
Deworming for older children? Following William Cutting's comment in DD47, Andrew
Tomkins discusses some benefits of deworming programmes.
Dr Cutting raises important issues about appropriate strategies against
helminths.
While it is true that pre-school children suffer a considerable burden of ill health, I am
concerned that the current emphasis on child survival programmes has led to the neglect of
the health of school-age children. The impact of helminths on growth and development of
school-age children needs to be seriously considered. While it is important to emphasise the need to improve water supplies and sanitation,
after a decade of highlighting these issues many children still live in disadvantaged
environments. Is it, therefore, reasonable to rely on environmental control and improved
personal hygiene alone to reduce the prevalence of gut parasites? Many parents would argue
that it is not, and in many countries purchase of anti-helminthic drugs, even by poorer
families, is seen as a high priority. Drug costs have fallen quite markedly over the last few years. In a programme in
Indonesia, over 80 per cent of parents with children attending schools pay US$0.50 per
year for a service which, among other aspects of health care, involves distribution of
anti-helminthic drugs. In Zanzibar, the Department of Education has decided to distribute
them through schools. Environmental improvements and oral rehydration are crucial, and should be emphasised
at all times. They are not sufficient, however. Programmes which emphasise the importance
of personal hygiene, sanitation and safe water supply can act in tandem with
deworming. These approaches are not just part of another vertical programme to be imposed on a
community. Parents are looking to schools as an investment in the future of their
children. They may well regard initiatives in parasite control as something to be
welcomed. Professor Andrew Tomkins, Institute of Child Health, 30 Guilford Street, London WC1N
1EH, UK.
Traditional handwashing The Shona community in Zimbabwe customarily teaches children to wash their hands before
meals. People used to pour water over their hands from a locally made earthenware vessel
with a long, narrow spout. Families now tend to wash their hands communally, using a
wide, flat dish, with the youngest children washing their hands last. I wanted to find out if this way of handwashing involves a greater risk of infection
than the traditional method, and if teaching people to wash their hands under running
water would affect the incidence of diarrhoea. I selected the mothers of 70 children who
came to the local hospital with severe diarrhoea. Half were taught about washing hands
under a running tap or in water poured over them from a vessel. The other half were not
taught this method. After nine months, fewer than half the children of mothers in the first group had come
to the hospital again with diarrhoea infections, whilst nearly three quarters of the
children in the 'control' group had been brought to the hospital. Although very small, the
study encouraged us about the health benefits of educating people about washing their
hands under running water. Dr Vitalis Chipfakacha, Senior Regional Medical Officer, PO Box 5,
Tsabong,
Botswana.
Note: In this community there was no shortage of running water.
'Keep animals out of your house!' The health team of WaterAid is trying to help people in rural and semi-urban
communities of Nepal to build and use hygienic toilets. After reading DD45 we will also try to prevent the spread
of disease by animals, especially chickens.
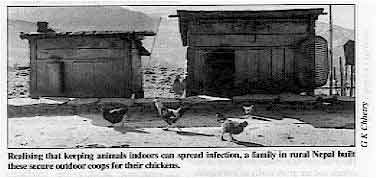 |
Realising that keeping animals indoors can spread infection, a
family in rural Nepal built these secure outdoor coops for their chickens. |
Chickens are kept for economic and religious reasons. In poorer communities, ' people
keep them inside their houses. We now intend to try to encourage people to build chicken
coops and to keep chickens out of the house. G K Chhetry, Health Co-ordinator, WaterAid, Nepal.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Assistant editor Nel Druce
Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Nicole Guérin (France)
Dr Norbert Hirschhorn (USA)
Dr Sharon Huttly (UK)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 48 March 1992
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
updated: 23 April, 2014
|