|
| |
Issue no. 50 - September 1992
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 50 - September
1992
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 50 September
1992  Page 1 2
Page 1 2
DD turns 50: looking forward
Dialogue on Diarrhoea celebrates its fiftieth issue this month. Bert
Hirschhorn, an international editorial adviser since the start of the newsletter in 1980,
looks at progress in the control of diarrhoeal diseases over the last 12 years and
outlines future challenges.
|
The message for the future: child health not just child survival
Congratulations to Dialogue on Diarrhoea on its 50th issue, as fresh
today as its first, 12 years ago. DD now reaches more than a quarter of a
million readers in 172 countries and 10 languages. Diarrhoea used to be an impolite word.
|
 |
Now, thanks to health workers at all levels; the major international agencies -
including WHO, UNICEF and USAID; ministries of health: non-government
organisations; and Dialogue
on Diarrhoea, control of diarrhoeal diseases is an essential child health
programme in virtually every developing country. Since 1980 case management of diarrhoea has improved markedly - in the home, the
hospital and nationally. Where case management has improved, the number of deaths from
diarrhoea has decreased sharply, and fewer children are seen with severe dehydration.
During ; the current cholera epidemic in Latin America, remarkably, less than 1 per cent
of those affected have died, thanks to a decade or more of control of diarrhoeal disease
(CDD) training and preparation. WHO now estimates that up to 90 per cent of all diarrhoea
deaths of children may be prevented by rehydration, continued feeding and use of
antimicrobials in specific cases. The cost of CDD, whether expressed in cost per death
averted or in absolute terms compared with other programmes, is very low. In the past 12 years oral rehydration therapy (ORT) has proved to be effective as more
than just supportive treatment for mild illness. It saves lives under extreme conditions:
from low birth weight neonates in incubators to elderly people in nursing homes; in
conditions of stress in refugee camps and on mountain sides; in people with AIDS; and in
children with severe dehydration when intravenous fluids are unavailable. Research in CDD has also expanded dramatically. Significant findings include:
- Continued feeding during diarrhoea - with breastmilk, milk or weaning foods - protects a
child's nutrition, and also shortens the episode. Good case management, therefore, not
only saves lives, but strengthens those who recover.
- A highly effective cereal based oral rehydration solution can be made and used at home,
and improves the outcome.
- Confirmation that basic hygiene and sanitation - hand washing, and the availability of
sufficient clean water and latrines - definitely reduce the incidence of diarrhoea and
have the greatest effect when all these factors are combined.
- Up to 80 per cent of cases of diarrhoea seen at health facilities have an identifiable
microbe (viral, bacterial or protozoan) as the cause. Routes of transmission are now
better understood, and this knowledge will help in prevention.
- Social scientists have provided us with information about families' knowledge of and
response to their children's diarrhoea. Mothers search eagerly for a rapid cure, but ORT
takes time and patience to give and by itself does not stop diarrhoea. It has been useful
to discover that mothers worldwide are two to three times more likely to use ORT when the
child has specific serious symptoms - frequent watery stools, vomiting, listlessness, and
loss of appetite - than for simple diarrhoea. Children with these symptoms run a high risk
of death through dehydration.
- Mass education and modern communications have proved highly successful in promoting CDD
messages to families and health workers alike.
In the next 12 years, CDD has several new paths to explore. The important ones, in my
opinion, are to:
- Eliminate the unnecessary and harmful use of so-called anti-diarrhoeal drugs (and
over-use of antibiotics) through better and wider training of health workers; educating
the community; political and administrative actions; and better understanding of the
social and economic factors influencing the misuse of drugs. This requires working with
private medical practitioners as well as with government personnel (see="su50.htm">insert
in this issue of DDDD).
- Continue nutritional research - into local foods such as porridge, soured milk
and yoghurt, and fermented cereals; into micronutrients such as vitamin A, zinc, iron and
glutamine; into the use of cereal based ORT (both home made and packaged); and the effects
of all these on treatment and prevention of diarrhoea.
- Determine the causes and best treatment of persistent diarrhoea.
- Integrate CDD activities with other programmes, notably immunisation, ARI control, water
and sanitation, and family spacing.
- Develop and deliver cost effective anti-diarrhoeal vaccines.
- Expand our understanding of the knowledge, attitudes and practices of mothers. It is
important that we know more about the constraints they face in case management -
particularly in safe preparation and use of ORT (why do some mothers know about ORT and
fail to use it?) - and in prevention of diarrhoea.
- Continue to demonstrate and publicise the direct link between poverty and illness,
between social injustice and malnutrition.
Some writers have recently proposed that saving lives only worsens the world's
population crisis. They refuse to recognise that health programmes such as CDD strengthen
children who would survive diarrhoea episodes without treatment, but would be left in a
weakened state. The choice in the coming decade, therefore, is between more children who
are chronically sick and listless or more children who are healthy and competent. In our
goals and evaluations, we must stress child health, not just child mortality. Dr Norbert Hirschhorn, c/o The Ford Foundation, PO Box 2030, Jakarta, Indonesia.
|
In this issue:
- The role of nurses
- Relactation
- Supplement on drugs and diarrhoea
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 50 September
1992  1 Page 2 3 1 Page 2 3
| Nurses and midwives play a vital role in preventing deaths through diarrhoea. Their
respected position in the community and frequent contact with mothers make them ideal
people to promote good health practices. They can also help ensure that children receive
correct treatment when they get diarrhoea. DD looks at the role of nurses
-in supporting breastfeeding and advising mothers on how to treat diarrhoea -and what can
be done to improve nursing training. |
Promoting the benefits of breastfeeding
Nurses and midwives have an important part to play in helping babies get off to a
good start in life by promoting breastfeeding which sustains and protects babies against
disease.
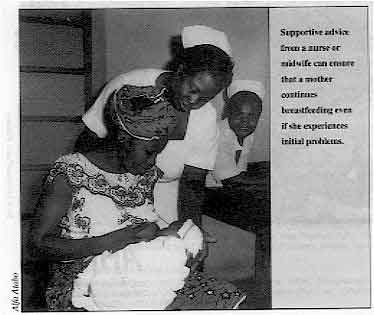 |
Supportive advice from a nurse or midwife can ensure that a
mother continues breastfeeding even if she experiences initial problems.
Good advice from a midwife or nurse can ensure that a mother prepares herself well for
breastfeeding, starts breastfeeding as soon as the baby is born and continues to
breastfeed until well after the child has begun to eat other foods.
|
It is important to discuss breastfeeding with a woman while she is pregnant, so that
she knows about the benefits to herself and her baby and is ready to persevere even if she
is offered formula milk or experiences problems at the beginning. Mothers should be
reassured about unnecessary worries such as concerns that their breasts are too small, or
that breastfeeding may make their baby constipated. Starting to breastfeed The following steps help a woman to initiate breastfeeding:
- Give the baby to the mother to hold immediately after birth.
- Encourage the mother to begin breastfeeding within half an hour of birth.
- Help the mother with the first feed. Ask her how she feels, observe her feeding and make
sure the baby is suckling in a good position.
- Do not give the baby any food or drink other than
breastmilk, unless there is a sound
medical reason.
- Let the baby stay in the same room as the mother, day and night from the time of birth
(sometimes called 'rooming-in').
- Allow unrestricted feeding with no limits on time or frequency (called 'demand
feeding').
Sustaining breastfeeding Nurses and midwives in health centres and in the community should make use of
opportunities when they come into contact with mothers to encourage them to continue
breastfeeding, for example during family planning discussions, immunisation days and
clinic visits. The advice to mothers should include:
- Continue with exclusive breastfeeding for at least four to six months.
- Continue with breastfeeding, in addition to giving other foods, up to age two years or
beyond.
- Encourage other mothers and pregnant women to breastfeed.
Extra help is needed for mothers with low birth weight babies, twins or babies with
disabilities. Mothers with problems, such as sore nipples or worries about their milk
supply, need individual help and advice. Mothers who work away from home also need support
to continue breastfeeding. With thanks to WHO.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 50 September
1992  2 Page 3 4 2 Page 3 4
How to help a woman to
re-establish lactation Almost all women are capable of breastfeeding, even those whose milk has dried up
after a gap in breastfeeding. Midwife Katherine Carter explains
how health workers can help mothers to re-establish lactation, by providing information
and support. What is relactation?
Relactation is the re-establishment of the milk supply after a woman has stopped
breastfeeding for anything from a few days to a few months (in general, it is taken to be
less than six months). It also includes increasing an insufficient milk supply. It is also
possible to induce lactation in women who have not lactated for years or who have
never been pregnant. The same principle applies to relactation as to induced lactation:
both are initiated and maintained by an infant suckling frequently at the breast. Breastfeeding and hence relactation are important for two reasons: Infant health: research shows that breastfed babies are less likely to suffer
from acute respiratory infections, diarrhoeal diseases, and malnutrition. Maternal health: the cost of buying formula, the time spent finding fuel and
preparing infant milk feeds or caring for a sick child mean that a mother also benefits
from breastfeeding. Reduced fertility rates caused by regular suckling may also improve
her health. What is needed for relactation? Motivation: the desire to breastfeed and to re-establish or increase lactation
is more important than a woman's physical condition. There are examples of post-menopausal
women who have relactated and been able to feed babies. Nipple stimulation: an infant sucking the nipple stimulates nerve impulses that
cause the release of a hormone called prolactin which acts on the breast to produce milk.
This is the best way to stimulate the breasts to produce milk. Support: a woman is affected by the views of her family and friends about infant
feeding. In some places, women work away from home, and have to leave their infants for a
relative to feed. In these circumstances, women need practical and emotional support and
encouragement to re-establish and maintain lactation and to breastfeed when they are at
home, and express breastmilk for feeding when they are not. Information: health workers have a key role in supporting and encouraging
women's confidence in breastfeeding and relactation. They need to know the basic facts:
- Increased nipple stimulation leads to increased milk supply.
- Only a tiny proportion (probably less than 1 per cent) of all women are physically
unable to breastfeed - if a woman has breastfed before it is very likely she can do it
again.
- Stress may temporarily inhibit the flow of milk, but does not affect its production, so
even in a stressful situation increased suckling will result in greater milk production.
- Except in famine conditions, malnourished mothers are able to produce enough milk. If
possible they should be given food supplements to help keep up their own body strength.
Relactation in practice Mulago Hospital, Uganda: a starving teenage mother was admitted with a
malnourished two month old infant. She had not produced any breastmilk for several weeks.
After admission, she was encouraged to suckle the infant frequently, even though the
infant's dietary requirements were met by formula milk. The young mother was also given
food. Within a few days of admission her milk production was reinstated and the infant
could be fed on breastmilk alone.
|
How to relactate
- Establish that the woman wants to relactate. Be confident but realistic. Persistence is
required, particularly during the first two to four days.
- Find out what sort of support is available to the mother, for example family, friends,
health worker, health facility.
- Decide whether treatment or referral is necessary (and available) for health problems of
the mother.
- Explain to the mother about the need for regular nipple stimulation in order to
re-establish the flow of milk. This needs to happen 8-10 times a day, which means
breastfeeding the infant every 2-3 hours, with a longer gap at night to give the mother
time to sleep.
|
A breastfeeding supplementer - a cup of milk with a
nasogastric tube leading to the breast - helps the baby get used to feeding at the breast
while the mother's milk supply is being re-established. The baby may need to learn to suckle at the breast if previously bottle or tube fed, or
if it has been too sick to breastfeed for a while. To help to do this, the mother should
keep the baby close to her at all times. The baby should be encouraged to suckle whenever
it is willing. Hold the baby close to the breast and make sure that it takes a mouthful of
the breast tissue (see="su37.htm">DD37 breastfeeding supplement).
|
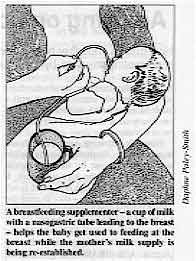 |
One way to get the baby to suckle when the breast is not producing a lot of milk is to
use a breastfeeding supplementer (pictured above). At its most basic, a breastfeeding
supplementer is a cup of milk from which a nasogastric tube leads to the nipple. The baby
can suck on the tube at the same time as suckling on the breast. Alternatively, milk can
be dripped over the mother's breast to get the infant to suckle. Even if an infant suckles
only a little to start with, often the case in babies over three months of age, this will
tend to increase after a week. Another method of encouraging the baby to suckle is to give
it to another woman who is producing milk so the baby can learn the suckling action.
- A safely prepared artificial formula may be needed for an infant who is starting to
suckle at the breast again while lactation is being established. There is no need to
dilute the formula. Reduce the volume of the formula by about 30ml per day, as the supply
of breastmilk increases, Check the baby' s weight to make sure it is receiving enough
milk. It is better to use a cup and not a bottle with a teat, because a bottle and a teat
are more difficult to keep clean and if a baby sucks from a teat it may be less willing
then to suckle from the breast because the sucking action is different.
- It takes about two to three weeks to re-establish an adequate supply of milk, although
this can vary. Mothers trying to re-establish lactation need constant encouragement,
especially in the first few days. Health workers should see women as often as possible
during this time. Other women who have successfully relactated can also help provide
support and advice.
- Lactogogues are substances said to increase milk supply. Those which are culturally
acceptable and not harmful, e. g. some herb teas, can be helpful. A nutritious diet is
probably more important. Hormone therapy is rarely used, and hormone stimulating drugs may
do no more than increase the medical acceptability of the process in the eyes of health
workers or the community.
Katherine Carter, 18 Belton Road, Bristol BS5 OJF, UK. A full list of references for this article is available on request from
AHRTAG.
Relactation in practice Saigon, Vietnam: women who volunteered for a programme to induce
relactation ended up successfully feeding two orphans each. Bangladesh: a relactation programme among refugees affected by famine was
also successful, with women (if not the infant's mother, then a relative or friend) being
induced to lactate within a few days. Makere Hospital, Kampala, Uganda: a relactation programme among
well-nourished women included strict frequent feeding of their infants (at least every two
hours), supplementary feeds, giving one pint of cow's milk daily to the mother, and
reassurance and information from staff.
|
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 50 September
1992  3 Page 4 5 3 Page 4 5
Advising on home management of diarrhoea
How nurses and other health workers talk to mothers about treating diarrhoea is
very important. WHO is promoting this step-by-step guide to informing mothers about good
practice. How a mother treats her child's diarrhoea at home depends largely on how well a nurse
or other health worker has advised her. Every nurse should consider herself to be an
adviser. However, advising mothers on home management of diarrhoea is usually the last activity
carried out by the busy health worker, and often the least well done. It may be difficult
to judge how much to tell a mother in a short time - how to cover the essential
information without overloading her with too much to remember. To assist nurses and other health workers with this task, WHO suggests the following
process: ASK - PRAISE - ENCOURAGE - ADVISE - CHECK ASK questions about what was done for the child before coming to the
health centre, specifically about the drinks, food and treatment the child has taken. PRAISE AND ENCOURAGE the mother's helpful actions. Every mother
bringing a child for care has done something right, even if it is only coming to the
health facility. Identify and praise correct action. This will encourage her and build her
confidence, and make it more likely that she will follow the health worker's advice. ADVISE - Even if a mother has done some things correctly, she may need
advice about other things to do and to be tactfully warned against harmful practices. She
will also need to know the signs to watch out for which mean her child should be brought
back for further care. CHECK - It is important to find out exactly what the mother has
understood so that any misunderstandings can be corrected. It is better not to ask: 'Do
you understand? ' She will probably answer 'yes', thinking she has understood or because
she is too afraid to say no. Ask her to describe what she will do when she returns home.
This is a better way of checking her understanding. When talking to mothers, nurses should also keep in mind the rules of case
management in the home:
- Give the child more to drink than usual.
- Encourage the child to breastfeed / eat.
- Bring the child in for care if s/he shows any of the following danger signs:
- Is eating or drinking poorly
- Passes many watery stools
- Is very thirsty
- Is vomiting frequently
- Has fever
- Has blood in the stools
- Is not getting better.
Thanks to WHO. UK nurses need basic ORT training
The UK could learn from developing countries about educating nurses on diarrhoea
management. Karen Whibley argues for better nurse training on
ORT in the UK. Nurses are in a key position to change public thinking about health issues. A major
part of the nurse's role is health education and this is reinforced by the public
perception that nurses have specialist knowledge. Much of nurses' knowledge is gained 'on the job'. The use of oral rehydration therapy
(ORT) is a case in point. Nurses in the UK usually receive little or no formal training on
the subject. As a result, many nurses are unsure what ORT is and how it works. They are
therefore unable to teach the public correctly and may, unintentionally, perpetuate
incorrect ideas about how to manage diarrhoea. For example, the main mistaken belief is
that ORT is a cure for diarrhoea. In addition, it is often recommended that young children
be 'starved' for some days. A typical scenario might involve a mother bringing her baby suffering from diarrhoea to
a casualty department, or to the practice nurse at a general practitioner's surgery. Once
seen by a doctor, oral rehydration salts (ORS) may be prescribed, but the mother may not
be told what ORS is, how to give it, how it will help her child, or that it will not cure
the diarrhoea. A joint and consistent approach is needed among doctors and nurses who deal with
parents of children with acute diarrhoea, to reinforce good practice. This is starting to
happen in many areas, and is reducing the number of children presenting to hospital
casualty departments with this problem. Although diarrhoea is less common in the UK and often less serious than in developing
countries, a number of babies do die every year in the UK as a result of diarrhoeal
dehydration, deaths which could easily be prevented by the timely use of ORT.
Unfortunately, the UK is lagging behind developing countries in the promotion of ORT and
training about ORT is often not included in nursing courses. Nurses should be taught the
physiology of diarrhoeal dehydration and the rationale of ORT. With that knowledge, they
would be able to explain to parents that it is not a cure but a mechanism by which fluids
are replaced, thus preventing progression to serious dehydration. Karen Whibley, Gastroenterology Research Nurse, Queen Elizabeth Hospital for
Children, Hackney Road, London E2 8PS, UK.
Resource package for nurse training The CDD programme of WHO is preparing a package of training materials to help nurses
and midwives to update their skills and knowledge. The package will include:
- a module on advising mothers
- resources on breastfeeding counselling
- a manual for trainers of nurses and other health care workers on teaching about
diarrhoeal disease control.
Available from The Diarrhoeal Diseases Control Programme, WHO, CH-1211 Geneva 27,
Switzerland.
|
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 50 September
1992  4 Page 5 6 4 Page 5 6
Sahel nurse training scheme
Suzanne Prysor-Jones reviews the experience of
introducing diarrhoeal disease control (CDD) teaching modules in schools of nursing in the
Sahel region of West Africa.
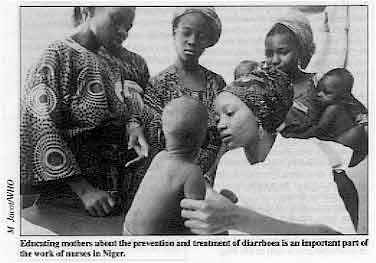 |
Educating mothers about the prevention and treatment of
diarrhoea is an important part of the work of nurses in Niger. Twenty-one schools of nursing, in Mali, Niger, Senegal, Burkina Faso, Mauritania and
The Gambia, were the focus for a joint PRITECH (1) - WHO initiative to
introduce a training package, which included teaching modules and a work book for use by
students during work placements.
|
The modules covered:
- an epidemiological overview and clinical concepts
- the treatment and prevention of diarrhoeal diseases
- cholera
- health education techniques
- the national CDD programme.
Lessons learned Lessons learned from the experience of introducing the training package include:
- Teaching modules can be introduced into a curriculum that is not run on a modular basis.
- Participation in developing the modules (through discussions of proposed modules and
attendance at workshops to review the drafts) motivated the schools to use them.
- Active involvement of the national CDD programme helps to ensure that the modules are
used.
- Making a set of teaching materials available to teachers and students increases
motivation and allows students to study outside the classroom, and to use the modules as
reference materials.
- Follow-up is necessary to solve some of the problems that arise. For example, one of the
schools in Mali's capital, Bamako, was distributing the modules to students without
actually teaching them. The teachers were finding it difficult to integrate them into
their teaching. A teacher from another school where the modules were being used well was
sent by the CDD programme to share experience of using the modules.
Common problems
- Student work experience is often hastily prepared and lacks supervision due to limited
resources. Most nursing schools do not have clear guidelines for work experience. Students
tend to be used mainly as extra workers for routine tasks.
- Case management is poor in some of the health facilities where students are placed and
it is usually difficult for teachers from the nursing schools to intervene in case
management. There are too few facilities with good case management practice to cater for
the large number of students. National CDD programmes have a key role to play in upgrading
case management practice to ensure consistency between what the students see in the field
and what they learn in training schools.
Evaluation
- Use of the modules has helped to create links between national CDD programmes and
training schools, providing a possible model for other priority public health programmes.
- The modules have resulted in more time being allocated to CDD in all schools using them.
- Informal interviews with teachers and students have revealed that many of them would
like similar clear and standardised materials for other health issues.
Suzanne Prysor-Jones, PRITECH, BP 3047, Dakar, Senegal.
The role of nurses in the Sahel There are very few doctors in the Sahel region of West Africa, particularly in rural
areas. A region of about 100,000 inhabitants might typically be served by only one or two
doctors, based in the district capital, often with administrative responsibilities. Public
health efforts rely mainly on the work of nurses for day-to-day implementation. Nurses are usually responsible for:
- the running of health centres or dispensaries
- diagnosing and treating sick children, particularly in rural areas
- following up diarrhoea cases even if the child has been seen by a doctor
- managing well-baby clinics
- most of the health education
- training and supervising village health workers.
It is therefore extremely important that nurses have solid pre-service training in
diarrhoeal diseases.
|
1 PRITECH (Technologies for Primary Health Care) is a
USAID funded project.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 50 September
1992  5 Page 6 7 5 Page 6 7
Gluten intolerance I was in Ecuador until a few years ago and developed chronic diarrhoea which was
diagnosed as amoebiasis. Drugs had no effect. When I returned to the UK I was diagnosed as
'coeliac'. Is gluten intolerance increasing in developing countries where people have only
recently started eating wheat based foods'? Gita Hahn, London, UK.
Professors Gordon Cook (Hospital for Tropical Diseases, London) and David Candy
(King's College Hospital, London) reply: Coeliac disease can be more accurately described as gluten intolerance. It is a
genetically determined abnormality of the small intestine. Symptoms are caused by eating
gluten (a mixture of proteins found in wheat and certain other cereals such as barley or
rye). which is harmless when eaten by most people. Exactly how gluten acts is unclear, but
it damages the mucosa (lining) of the small intestine, causing the villi (finger-like
protuberances which increase the absorptive area) either to become blunted or to
disappear. The result is that normal absorption of food cannot take place. This leads to weight
loss, or failure to thrive in infants and children, and deficiencies in some vitamins (e.
g. folic acid) and minerals (e. g. iron). There is usually diarrhoea with large, pale and
foul smelling stools, sore tongue and mouth ulcers, tiredness, abdominal discomfort and,
in longstanding cases, osteoporosis (poorly calcified bones) can result. Symptoms often
begin as soon as wheat based foods are introduced, although they may start in adults. The
severity of the symptoms varies. There is evidence that the disease exists in India, although it is not often diagnosed.
A few reports exist from African countries and China. However, this does not necessarily
mean that these populations are rarely affected, but more likely reflects the fact that
they eat very little gluten. More research is necessary to find the true prevalence of the
disease in developing countries. In the UK about 1 in 2,500 of the population is known to
have coeliac disease. Treatment consists of strict elimination of gluten from the diet. Even the smallest
amount will rapidly cause damage to the small intestine, and strict avoidance of gluten in
an affected person must be life-long.
|
Handbooks for health Healthlink Worldwide (formerly AHRTAG) produces a wide range of health and development publications which are
available at low cost (or, in some cases, free to readers in developing countries). These include manuals on:
- making a cold box for vaccines
- refrigerator maintenance
- running a health centre store
- managing district dental services
- low cost disability aids
- and helping disabled children to move through play.
The manuals are available through TALC, a UK distributor.
Healthlink Worldwide also produces newsletters
on primary health care action and overview, acute respiratory infections, community based
rehabilitation, and AIDS prevention and care, as well as booklets on topics such as drug
packaging and laboratory investigations.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 50 September
1992  6 Page 7 8 6 Page 7 8
Glass-sized SSS In DD47, where you mentioned recipes for SSS, a Madras
reader's recipe for sugar salt solution (SSS) using one pinch of salt and four pinches of
sugar was corrected. I would like to point out, however. that the Madras recipe is for one
tumbler (200ml) of water, not for a litre bottle. Can you please publicise this. as I am
being questioned by DD readers here about it. Father Emmanuel Mariam Pillai, Educational Multi Media Association, 32 College Road,
Nungambakkam, Madras 600 006, India.
Dr William Cutting replies: Thank you for drawing this to our attention. Local recipes do often relate to locally
available containers, and the Madras recipe reflects this. WHO recommends an early start
to rehydration using 'home available' drinks (water, rice water, soup, yoghurt drinks,
etc). Sugar salt solution (SSS) can also be used if the ingredients are available and
mothers know how to prepare it correctly.
Super 'ORS' recipe Mutolere Community Based Health Care Programme in Uganda has been promoting a solution
to prevent dehydration known as super 'ORS'. Ingredients:
- 1.5 litres water (3 tumpeco mugs or 3 Uganda beer bottles)
- Handful of flour (sorghum. millet, or maizemeal)
- Level teaspoon salt (or large pinch using 3 fingers)
- Fruit if available (e. g. 3 medium tomatoes)
Method: Ensure all utensils to be used are clean and wash your hands. Mix the flour and salt
with a little of the measured water and heat the remaining water. When it is boiling, stir
it into the flour mixture. Cook for 10 minutes. Peel and chop the fruit finely (especially
if the solution is for an infant) and add it two minutes before the solution is ready. When cooled, give infants one quarter of a tumpeco mug after each loose stool (adults
and children half a tumpeco mug). Keep the solution covered and discard after 24 hours. Important: Super 'ORS' should be given to the person with diarrhoea in addition to other foods -
not instead of them. Mothers should continue to breastfeed their infants. Super
'ORS' is not a medicine. If the diarrhoea patient does not improve or becomes worse, take
them to a health centre. The addition of fruit is optional but makes the solution more palatable: tomatoes
provide potassium as well as a nice flavour. The ingredients for this recipe do not
require precise measurement: a handful of flour may vary somewhat from person to person
without affecting the solution's benefits. Super 'ORS' has been well received by villagers. Sugar is very expensive and is not a
standard ingredient in their homes. Promoting ORS sachets perpetuates the myth that
imported packages are better than what is locally available. In fact the reverse is true!
Furthermore the sachets may not be available when needed. Super 'ORS' is proven to be more
effective in actually reducing diarrhoea. It is more nutritious than alternative recipes.
The ingredients are more readily available to people in rural areas. Communities elsewhere
can adapt super 'ORS' according to flour, fruits and measurements available. Vivienne Lumley, Health Visitor, VSO Uganda.
Dr William Cutting replies: ORS usually refers to the standard WHO / UNICEF formula of oral rehydration salts. Here
it is used for a special home made oral rehydration solution, which is apparently easily
made and well accepted in Uganda. These are important advantages. However, in cases where
a child is dehydrated, the WHO / UNICEF formula is more effective because its precise
formulation is designed to replace all of the salts and water lost in the liquid stool.
The formula used in Uganda is undoubtedly effective and should be encouraged, provided
mothers prepare and use it correctly.
Rice electrolyte solution I work at a paediatric clinic in a remote eastern village in Tamil Nadu, south India,
where gastroenteritis is a major problem. The concept of oral rehydration therapy (ORT)
has made a real breakthrough in reducing mortality from acute gastroenteritis. For the
past ten years, we have been using rice electrolyte solution (RES). We get about 150 cases
per month and 90 per cent of them are treated with RES alone. RES is willingly accepted by both high and low socio-economic groups. Now most of our
children have started taking RES at home before coming to our clinic. We feel that the
confidence they have in ORT is due to supervised therapy given at our clinic, even while
intravenous fluids (which are only given when ORT fails) are available. Dr D Meikandan, Avvai Child Care Clinic, Avvai Street, Bharathi
Nagar, Ramanathapumm 623 535, Tamil Nadu, India.
Soya bean success I am the co-ordinator of a self help programme which aims to combat malnutrition
and child mortality through the use of soya beans. Since we found a way of preparing soya which suited local tastes. soya has become well
known and used throughout Zambia. As we are mainly dealing with malnourished children. we
are confronted with diarrhoea every day. Our programme includes education, child monitoring and practical cookery demonstrations
and teaching mothers general health care. We advise the mothers of children suffering from
diarrhoea to make their own oral rehydration fluids and to add to this fluid three
tablespoons of cooked soya flour. The mixture is cooked and cooled, then fed to the child.
We have used this method for four years with great success. We have found that the
addition of soya breaks the vicious cycle of malnutrition -> inability to digest food
-> diarrhoea -> no food to the body -> malnutrition. We feel that spreading the use of soya, thus reducing malnutrition, would automatically
reduce the problem of diarrhoea. Renate Schempp, Co-ordinator, Soya Nutrition Project, PO Box 90612,
Luanshya, Zambia
Dr William Cutting replies:
If adding soya makes the oral rehydration fluid more acceptable then that is good.
Beware of confusing the replacement of lost fluids and electrolytes (rehydration) with the
need for good nutrition. Cereal based ORT has very little nutritional value and will not
break the diarrhoea / malnutrition cycle. As soon as children are rehydrated, they should
be given their usual diet again, possibly in increased amounts.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue no. 50 September
1992  7 Page 8 7 Page 8
Correction - ORS tablets Page 7 of DD47 featured questions and
answers about ORT. It mentioned the availability of ORS tablets which dissolve in water.
The Program for Appropriate Technology in Health (PATH) informs us that the ORS tablet
(Servidrat oral rehydration salts) is manufactured by Ciba-Geigy. For further information
please contact Ciba-Geigy AG, Klybeckstrasse 141, CH-4002 Basel, Switzerland.
|
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Executive editor Kate O'Malley
Production Katherine Miles Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Nicole Guérin (France)
Dr Norbert Hirschhorn (USA)
Dr Sharon Huttly (UK)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Dang Duc Trach (Vietnam)
Professor Andrew Tomkins (UK) With support from AID (USA), Charity Projects (UK),
Ministry of
Development Cooperation (Netherlands), ODA (UK),
SIDA (Sweden), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 50 September 1992
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
|