|
| |
Oral Rehydration Therapy
Health Basics: A supplement to Issue no. 19 - December 1984
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-6 Oral Rehydration Therapy
A supplement to Dialogue on Diarrhoea Online
Issue 19 - December 1984
|
DDOnline Oral
Rehydration Therapy supplement to DD19  Page 1 2
Page 1 2
HEALTH BASICS
ORAL REHYDRATION THERAPY
ORAL REHYDRATION THERAPY Oral Rehydration Therapy (ORT) is the cheap, simple and effective way to treat
dehydration caused by diarrhoea. When diarrhoea occurs, essential fluids and salts are
lost from the body and must be quickly replaced. Many of the millions of children who die
every year in developing countries from diarrhoea could be saved if they were given ORT
promptly. This includes giving extra fluids at home such as tea, soups, rice water and
fruit juices to prevent dehydration, and the use of oral rehydration salts (ORS) solution
to treat dehydration. Made up with clean water the ORS drink contains the main elements
that are lost from the body during diarrhoea. It is effective in treating dehydration
resulting from all types of acute diarrhoeal diseases. Many countries now have diarrhoeal disease control programmes, but ORT is still not
nearly as widely used as it should be and more effective information dissemination and
promotion of ORT is necessary. This leaflet This leaflet answers some of the most common questions asked about ORT and we hope that
it will be useful. Please send us any comments about your own work with ORT. What is dehydration? Dehydration is the loss of water and body salts through diarrhoea. Early features are
difficult to detect but include dryness of mouth and thirst. The signs of dehydration
include: sunken fontanelle (in infants); fast, weak pulse; breathing faster than normal;
loss of skin elasticity; sunken, dry eyes and reduced amount of urine. Rehydration is the
correction of dehydration. What is ORT? ORT is the giving of fluid by mouth to prevent and/or correct the dehydration that is a
result of diarrhoea. As soon as diarrhoea begins, treatment using home remedies to prevent
dehydration must be started. If adults or children have not been given extra drinks, or if
in spite of this dehydration does occur, they must be treated with a special drink made
with oral rehydration salts (ORS). The formula for ORS recommended by WHO and UNICEF
contains:
3.5 gms sodium chloride
2.9 gms trisodium citrate dihydrate (or 2.5 gms sodium bicarbonate)
1.5 gms potassium chloride
20 gms glucose (anhydrous)
The above ingredients are dissolved in one litre of clean water. WHO has
recently recommended a change in the complete formula, replacing 2.5 gms of sodium
bicarbonate with 2.9 gms of trisodium citrate dihydrate. The new formula gives the packets
a longer shelf life and is at least as effective in correcting acidosis and reducing stool
volume. Packets containing sodium bicarbonate are still safe and effective. How does ORT work?
|
A Haitian mother gives ORS solution to her child.
Acute diarrhoea normally only lasts a few days. ORT does not stop the diarrhoea, but it
replaces the lost fluids and essential salts thus preventing or treating dehydration and
reducing the danger. The glucose contained in ORS solution enables the intestine to absorb
the fluid and the salts more efficiently. ORT alone is an effective treatment for 90-95
per cent of patients suffering from acute watery diarrhoea, regardless of cause. This
makes intravenous drip therapy unnecessary in all but the most severe cases.
|
 |
Can ORS he used for everyone?
ORT is safe and can be used to treat anyone suffering from diarrhoea, without having to
make a detailed diagnosis before the solution is given. Adults need rehydration treatment
as much as children, although children must always be treated immediately because they
become dehydrated more quickly.
|
|
DDOnline Oral
Rehydration Therapy supplement to DD19  1 Page 2 3 1 Page 2 3
USING ORT TO PREVENT AND TREAT
DEHYDRATION Preventing Dehydration Mothers must learn:
- to respond to diarrhoea immediately by giving extra suitable drinks (see paragraph
on home solutions below).
- to recognize the signs of dehydration which need ORS or special care.
If ORT is given at home early on, dehydration can often be prevented and many children
will not become so ill that they need to see a health worker. Home drinks to prevent dehydration
- Mothers can use household liquids, preferably those that have been boiled, such as rice
water or carrot soup. Ideally these drinks should contain starches and/or sugars as a
source of glucose and energy, some sodium and preferably some potassium.
- A simple salt/sugar solution, if these ingredients are available, is also suitable for
early oral rehydration therapy. 1 level teaspoon (5 ml) of salt should be mixed with 8
level teaspoons of sugar in a litre of drinking water. Molasses and other forms of raw
sugar can be used instead of white sugar, and these contain more potassium than white
sugar. Do not use too much salt. If the solution has too much salt the child may
refuse to drink it . Also, too much salt can, in extreme cases, cause convulsions. Too
little salt does no harm but is less effective in preventing dehydration. (A rough guide
to the amount of salt is that the solution should taste no saltier than tears.)
Measuring home solutions Different countries and different communities use various methods for measuring the
salt and sugar. Finger pinch and hand measuring, and the use of local teaspoons can
be taught successfully. A plastic measuring spoon is available from Teaching Aids at
Low Cost (TALC) with proportions to make up 200 ml of sugar/salt solution. Whatever
method is used, people need to be carefully instructed in how to mix and use the
solutions. WHAT TO DO IF DEHYDRATION OCCURS If, despite extra home drinks, dehydration occurs, or the diarrhoea continues for more
than two days, the child should be taken to see worker to be given ORS solution. How to assess the degree of dehydration The table below describes what the health worker should ask and look for, and indicates
which treatment plan to follow.
|
1. Ask About |
liquid stools per day |
longer than
3 weeks duration |
| Diarrhoea |
Less
than 4 |
4
to 10 |
More
than 10 |
Chronic
diarrhoea |
| Vomiting |
None
or a small amount |
Some |
Very
frequent |
Blood
or Mucus in the stool |
| Thirst |
Normal |
Greater
than normal |
Unable
to drink |
|
| Urine |
Normal |
A
small amount, dark |
No urine for 6 hours |
|
|
2. Look At |
liquid stools per day |
Longer than
3 weeks duration |
| Less
than 4 |
4
to 10 |
More
than 10 |
| Condition |
Well,
Alert |
Unwell,
sleepy or irritable |
Very
sleepy, unconscious, floppy or having fits |
Severe
undernutrition |
| Tears |
Present |
Absent |
Absent |
|
| Eyes |
Normal |
Sunken |
Very
dry and sunken |
|
| Mouth & Tongue |
Wet |
Dry |
Very
dry |
|
| Breathing |
Normal |
Faster
than normal |
Very
fast and deep |
|
|
3. Feel |
liquid stools per day |
Longer than
3 weeks duration |
| Less
than 4 |
4
to 10 |
More
than 10 |
| Skin |
A
pinch goes back quickly |
A
pinch goes back slowly |
A
pinch goes back very slowly |
|
| Pulse |
Normal |
Faster
than normal |
Very
fast, weak, or you cannot feel it |
|
| Fontanelle (in infants) |
Normal |
Sunken |
Very
sunken |
|
|
|
liquid
stools per day |
Longer
than
3 weeks duration |
| Less
than 4 |
4 to
10 |
More
than 10 |
4. Take Temperature |
|
|
|
High
fever - 38.5ºC (or 101ºF ) or greater |
5. Weigh, if possible |
No
weight loss during diarrhoea |
Loss
of 25-100 grams for each kilogram of weight |
Loss
of more than 100 grams for each kilogram of weight |
|
6. Decide |
The
patient has no signs of dehydration |
If
the patient has two or more of these signs, he has some dehydration |
If
the patient has two or more of these danger signs, he has severe dehydration |
If
the patient has chronic diarrhoea, severe undernutrition, or high fever treat or refer to
the nearest health clinic for treatment. If there is blood or mucus in the stool and high
fever, suspect dysentery and treat with antimicrobials. |
Use
Plan A |
Use
Plan B |
Use
Plan C |
PLAN A: for NO DEHYDRATION * |
The health worker should discuss home drinks with the mother (see="#page1">page 1 and 3), feeding during diarrhoea and proper
home hygiene. The mother should be given enough ORS packets for two days if:
- her child has been on Plan B.
- it is national policy to give ORS solution to all children who visit a health centre for
diarrhoea treatment.
- the mother cannot come back if the diarrhoea gets worse.
Mothers given ORS packets to use at home must be carefully shown how to use them. The
amount of ORS solution she should give is:
AFTER EACH LOOSE STOOL:
- 50-100 ml (¼ - ½ cup) of ORS solution for a child less than 2 years old.
- 100-200 ml for older children. Adults can take as much as they want.
NOTE: Children receiving ORS solution must also be given the usual amount of
ordinary drinks they take each day. They should not also be given salt and sugar
solution. |
|
DDOnline Oral
Rehydration Therapy supplement to DD19  2 Page 3 4 2 Page 3 4
|
PLAN B : for SOME DEHYDRATION * |
1. Use this table to see how much ORS solution is suitable
for 4-6 hours treatment:
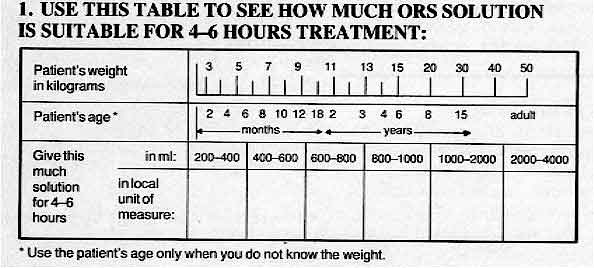
If the patient wants more ORS solution, five more. If the eyelids become puffy, stop
and give other fluids. Use ORS solution again when the puffiness is gone.
If the child vomits, wait 10 minutes and then continue slowly giving small amounts of
ORS solution.
2. If the mother can remain at the health centre
- tell her how much ORS solution to give her child
- show her how to give it
- watch her give it
3. After 4-6 hours reassess the child. Then choose the suitable treatment plan.
NOTE: For children under 12 months continuing treatment plan B after 4-6
hours, tell the mother to give:
- breastmilk feeds between drinks of the ORS solution,
or
- 100-200 mls of clean water before continuing ORS if she does not breastfeed her child.
4. If the mother must leave any time before completing treatment plan B, tell
here:
- to finish the 4-6 hours treatment as in 1. above
- to give the child as much ORS solution as he wants after the treatment
- to look for the signs of dehydration and, if the child has any, to return the next
morning.
Give her enough ORS packets for 2 days and show her how to prepare ORS solution.
Explain briefly how to prevent diarrhoea. |
|
DDOnline Oral
Rehydration Therapy supplement to DD19  3 Page 4 5 3 Page 4 5
What should be done if the child vomits? Vomiting does not usually prevent the therapy from being successful. Mothers must be
taught to persist in giving ORS solution, even though this requires time and patience. They
should give regular, small sips of fluid. Giving ORT reduces nausea and
vomiting and restores the appetite through correction of acidosis and potassium losses. Should feeding continue at the same time as ORT? Feeding, especially breastfeeding, should be continued once dehydration has been
corrected. Even if the diarrhoea continues or the child is vomiting, some of the nutrients
are being absorbed. Suitable food should not be withheld, as the child may become
malnourished. Once the diarrhoea episode has passed, the child should be given more food
than usual to make up for losses during diarrhoea. Breastfeeding is particularly
beneficial because breastmilk is easily digestible. It also contains protective substances
which help to overcome the infection causing the diarrhoea. What sort of foods are good during diarrhoea?
|
Small, frequent feeds of energy-rich local foods should be
given during diarrhoea.
- High energy foods such as fats, yoghurt and cereals are quite well absorbed during
diarrhoea. Small, frequent feeds of energy-rich local foods familiar to the child should
be given. A little vegetable oil can be added to foods such as millet or rice to increase
the energy content.
- Foods high in potassium are important to restore the body's essential stores depleted
during diarrhoea. Such foods include lentils, bananas, mangoes, pineapples,
pawpaw,
coconut milk and citrus fruits.
- Certain foods should be avoided during diarrhoea, for example those containing a lot of
fibre such as coarse fruits and vegetables, wholegrain cereals and spicy foods.
|
 |
Is it necessary to use drugs as well as ORT? Drugs should not be used except in the most severe cases. Even then they should
be administered with care, preferably after the organism causing the diarrhoea has been
identified. Small children with dysentery and fever require an antibiotic. Refer such
patients to a health service for advice. ORT on its own is usually enough to rehydrate the
child. Unnecessary antibiotic therapy upsets the normal bacteriological balance of the
intestine. Many anti-diarrhoeal preparations have proved to be either ineffective or too
powerful for very small infants. Can the solution be made with dirty water?
 |
Wherever possible, clean drinking water should be used to make
up oral rehydration solution. The benefits of fluid replacement in diarrhoea far outweigh the risks of using
contaminated water to make up oral rehydration solution. In situations where it is
difficult to boil water, mothers are advised to use the cleanest water possible. Can ORS solution be stored? Generally a made-up solution should be covered and not kept for more than 24 hours, due
to the risk of bacteriological contamination. Packets of ORS should be stored carefully
and not kept in temperatures of over 30°C or in conditions of high humidity. Where the
ingredients to make up ORS are being stored in bulk the glucose/sucrose should be kept
apart from the rest of the dry ingredients. The new citrate formula ORS has a longer shelf
life.
|
*Treatment plans on pages 4, 5 and 6 taken from the CDD/WHO Supervisory Skills
course, from the module on the treatment of diarrhoea.
|
|
DDOnline Oral
Rehydration Therapy supplement to DD19  4 Page 5 6 4 Page 5 6
ORT: COUNTRY EXAMPLES Trinidad and Tobago "In 1980, the Ministry of Health began a programme with the help of the
International Development Research Centre (IDRC) to promote ORT in Port-of-Spain. At that
time, a third of all infant mortality was due to dehydration from diarrhoea. In 1981, an
oral rehydration therapy unit was opened in the main hospital, run by nursing staff who
had been trained by a paediatrician from the University of the West Indies. The unit was
open daily and treated cases of mild to moderate dehydration using the locally produced
ORS-GESOL. Mothers were also given advice on using ORT at home, and about feeding and
diarrhoea. Some objections were raised to the leading role played by the nurses in the
unit - who only referred patients to doctors when they thought it necessary. However,
these attitudes changed when the success of the programme became clear. Over a six month
period there were 540 admissions to the unit and only 20 of these were unsuccessfully
treated. The oral rehydration programme also greatly reduced the number of admissions and
deaths in the gastroenterology ward. The nursery in the ward has now been closed. The ORT
facilities are now available all over the island and a massive health education programme
is continuing to promote the message of ORT ." India "In Narangwal, deaths in children aged between 8 days and three years have been
reduced by half through community workers using only oral rehydration therapy and
penicillin ..." Ethiopia "Since the Ethiopian national programme began in 1980, more than 50 CDD managers
have been trained successfully. Future plans include the establishment of an ORT training
centre in Addis Ababa, with UNICEF support, the training of more than 300 nurses in
diarrhoea management and supervisory skills, and the local production of ORS. The
Programme's overall impact will be assessed in 1985 ..." The Gambia "The role of oral rehydration therapy in diarrhoeal disease control has been
emphasized at two levels by the Gambian government. Health workers have been taught to
administer ORT using oral rehydration salts, and mothers have been taught to mix a safe
sugar-salt solution at home. The message has been successfully reinforced by a media
campaign - after one year 67 per cent of mothers could correctly mix a home solution and
47 per cent had used it once or more to treat their children. Not surprisingly, this early
preventive treatment at home has led to a drop in the number of mothers taking children
with diarrhoea to health centres from 85 per cent to 50 per cent ..." Philippines "The National ORT programme was introduced in the Philippines after encouraging
field trials. ORT was accepted by mothers who saw the beneficial results of using it. An
early problem was finding an easily available measuring device - initially local beer
bottles were used as they were found in most homes. Later a drinking glass, originally the
container for a popular brand of coffee, was found to be more practical. Good overall
co-ordination of the national programme was essential to its success. Problems arose in
the early stages when, for example, packets of salts were delivered without proper
instruction to mothers by staff who were not trained properly ..." HEALTH BASICS: ORT RESOURCE LIST Publications and newsletters The Management of Diarrhoea and use of Oral Rehydration Therapy - A Joint WHO/
UNICEF Statement, 1983. Available from WHO and UNICEF (see list of addresses). * Free. Oral Rehydration Therapy (ORT) for Childhood Diarrhoea, 1984. (Revised edition).
Population Reports, Series L, No. 2, Issues in World Health. Available from Population
Information Programme, John Hopkins University, USA (see list of addresses). Free. Proceedings of the International Conference on Oral Rehydration Therapy
(ICORT),
1983. Available from the United States Agency for International Development (see list
of addresses). Free. Oral rehydration therapy - Information for Action Resource Guide, 1983. Prepared
for UNICEF by the World Federation of Public Health Associations (see list of addresses). Journal of Diarrhoeal Diseases Research. Published quarterly by the
International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR, B). Cost US$15.00
to developing countries for four issues. (see list of addresses for ICDDR, B details). WHO Training Materials* A Manual for the Treatment of Acute Diarrhoea - for use by physicians and other
senior health workers. Guidelines for the Trainers of Community Health Workers on the Treatment and
Prevention of Acute Diarrhoea. 'For a full list of all WHO materials on clinical management of diarrhoea, training,
development of diarrhoeal disease control programmes etc. write to the Director of the CDD
Programme at the address given on the resource list. Bibliographies Resource Guide on Oral Rehydration Therapy, 1983. US $5.00 (prepaid, airmail).
World Federation of Public Health Associations. Available from the American Public Health
Association (see list of addresses). Oral Rehydration Therapy: An Annotated Bibliography, 1983. Scientific
Publication No. 445. Pan American Health Association. (Second edition). (see list of
addresses). This insert has been produced by
Diarrhoea Dialogue
with support from OXFAM
|
|
DDOnline Oral
Rehydration Therapy supplement to DD19  5 Page 6 5 Page 6
Newsletters Diarrhoea Dialogue. Quarterly newsletter on all aspects of the prevention and
control of diarrhoeal diseases. Available in English, Spanish, French, Portuguese and
Arabic. Order from AHRTAG, UK. (See list of addresses.) Glimpse. A newsletter reporting on the activities at ICDDR, B. Published 8 times
a year. Free. (See list of addresses.) Mothers and Children. Published three times a year in English, French and
Spanish. Free to developing countries / US$ 5.00 to others. Available from American Public
Health Association, USA. (See list of addresses.) Salubritas. Published quarterly in English at US$10.00 / year. Update on
community health resource material. Available from American Public Health Association,
USA. (See list of addresses.) World Neighbours in Action. Quarterly 'how-to-do it' newsletter on primary
health care published by World Neighbours. (See list of addresses.) Oral Rehydration: Bulletin of the Oral Rehydration Scheme of RUHSA. Published
bi-monthly by RUHSA, Christian Medical College, Vellore, P. O. Tamil Nadu 632 209, India.
Health education and teaching aids Diarrhoeal Diseases Control: Examples of Health Education Materials 1982. WHO/CDD.
Examples of posters, flashcards and leaflets from diarrhoeal disease control worldwide. Medex Workbook for Community Health Workers, No. 32: Prevention and Care of
Diarrhoea. 1983. (US$5.80, inc. surface mail. Available from The Medex Group - see
address section). Helping Health Workers Learn. Available from TALC, UK and the Hesperian
Foundation, USA. (See list of addresses.)
Specific country materials
Bangladesh: Manual on Treatment and
Prevention of Diarrhoea. 1980. International Centre for Diarrhoeal Diseases Research,
Bangladesh. (See address section.) Small training manual and flipchart for
CHWs. The Gambia: Health Workers Manual for
the Management of Acute Diarrhoea in the Gambia. December 1981. Health Education Unit,
Department of Medical and Health Services, Banjul, The Gambia. India: Better Care During Diarrhoea. Voluntary
Health Association of India (see address section) Small booklet about diarrhoea and
dehydration for CHWs. Well illustrated with photographs. Gives teaching advice and health
messages. Indonesia: Lina Regains her health
with Sugar and Salt Solution. Save the Children Fund, USA (see address section).
Pamphlet and flip chart. Jamaica: What to do when your baby has
diarrhoea. 1982. Ministry of Health, P.O. Box 478, Kingston, Jamaica. Liberia: Caring for Children and Diarrhoea. UNICEF/Inservice
Education Division, Ministry of Health and Social Welfare, P.O. Bag 9009, Monrovia,
Liberia. Nicaragua: Diarrhoea control and prevention
material: Jornadas Populares de Salud, Ministerio de Salud Publica, Managua,
Nicaragua. In Spanish. Zambia: Special position paper on
Nutrition and Diarrhoea. Health Education Unit, P.O. Box 30205, Lusaka, Zambia.
Sources of information Code:
- Development of diarrhoeal disease control programmes (D)
- Health education and information (H)
- Training (T)
- Operational and applied research (R)
- Supply and distribution of ORS (S)
- International Centre for Diarrhoeal Diseases Research, Bangladesh (ICDDR, B) (H)
(T) (R) Contact: Dr W B Greenough III
P. O. Box 128
Dhaka
Bangladesh
|
Oral Rehydration Therapy
Health Basics:
A supplement to Issue no. 19
December 1984
Page Navigation
This edition of Dialogue on Diarrhoea Online is
produced by Rehydration Project.
Dialogue on Diarrhoea was published four times a year in English,
Chinese, French, Portuguese, Spanish, Tamil, English/Urdu and Vietnamese and
reached more than a quarter of a million readers worldwide.
The
English edition of Dialogue on Diarrhoea was produced and distributed by
Healthlink
Worldwide.
Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any
uses made of the material.
|
updated: 23 August, 2019
updated: 23 August, 2019
|
version of this Issue