|
| |
Shigellosis
Clinical Update: A supplement to Issue no. 44 - March 1991
pdf
 version of
this Issue version of
this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-4 Shigellosis
A supplement to Dialogue on Diarrhoea Online Issue 44
- March 1991
|
DDOnline Shigellosis
supplement to DD44  Page 1 2
Page 1 2
Clinical Update
SHIGELLOSIS
Shigellosis, or 'baciliary dysentery', is an intestinal infection that is a major
public health problem in many developing countries, where it causes about 5 to I0 per cent
of childhood diarrhoea. This special DD insert provides an overview of
shigellosis, including cause, effect and treatment.
Shigellosis is characterised by the frequent and painful passage of stools that consist
largely of blood, mucus and pus, accompanied by fever and stomach cramps.
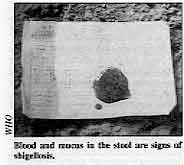 |
Blood
and mucus in the stool are signs of shigellosis.
In some developing countries more people die from shigellosis than from watery
diarrhoea. As many as 25 per cent of all diarrhoea related deaths can be associated with
Shigella.
|
What causes shigellosis? The symptoms of shigellosis result from infection with the Shigella bacterium. Two of
the four species of Shigella are common in developing countries. Shigella flexneri is
endemic (present at all times) in most communities. Shigella dysenteriae type 1
often occurs in an epidemic pattern; the organism can be absent for a number of years,
only to reappear and infect a large proportion of the population. These two species of
Shigella generally produce the most severe illness. In developed countries Shigella
sonnei is the most common and is the least virulent Shigella bacterium. Shigella
boydii causes disease of intermediate severity and is least common of the four, except
in the Indian sub-continent. Who gets shigellosis, and how common is it? Shigellosis is found throughout the world, mostly in children aged under five. Rates of
Shigella infection are highest where sanitation is poor. They are also influenced by
nutritional status, and environmental factors affecting transmission such as rainfall and
temperature. Shigella infections can occur throughout the year, but in most communities
the incidence is highest when the weather is hot and dry. This may be because the scarcity
of water limits handwashing and other hygiene measures that reduce transfer of the very
small number of bacteria needed to cause infection. Health workers are usually aware of the number of shigellosis cases, because symptoms
are severe, and therefore children with Shigella infections are more likely to be brought
to hospitals or clinics. Case fatality rates, even in hospitalised cases of dysentery, are
six to eight times greater than for watery diarrhoea. Dysentery is associated with
persistent diarrhoea. In rural north India, for example, nearly a third of all persistent
diarrhoeal episodes are dysenteric. During disease epidemics caused by Shigella dysenteriae type 1, as many as one
in ten people in affected communities will become infected, and as many as 10 to 15 per
cent of these will die. At the Diarrhoea Treatment Centre of the International Centre for
Diarrhoeal Disease Research in Bangladesh (ICDDR, B), over 700 patients a year with
shigellosis are admitted to an in-patient unit. Ten per cent of these patients die while
in hospital.
|
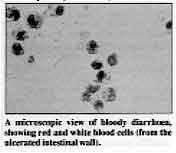
A microscopic view of bloody diarrhoea, showing red and white
blood cells (from the ulcerated intestinal wall).
Although these are patients with the most severe illness, their high mortality rate
shows the difficulties in treating patients with shigellosis, especially when they come
for care late in the course of the illness. Young children and elderly people are most
likely to die from the effects of shigellosis.
|
 |
At the ICDDR, B Treatment Centre, children under 12 months of age account for 21 per
cent of shigellosis admissions but up to 33 per cent of all fatal cases. Dysentery is
especially severe and more likely to be fatal in young infants, the malnourished, children
who are not breastfed, and following measles. Acute and particularly prolonged episodes of
dysentery often change marginal malnutrition to overt protein energy malnutrition, and can
lead to vitamin A deficiency. What are the effects of Shigella infection? Shigella infect the cells of the lining of the large intestine (colon). The bacteria
invade and damage these cells, producing breaks (ulcers) in the mucous membrane lining the
intestine.
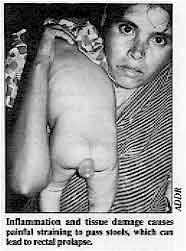 |
Inflammation and tissue damage causes painful straining to
pass stools, which can lead to rectal prolapse. These ulcers are most common in the rectum, which is the lowest part of the large
intestine. Ulceration of the intestinal lining results in increased production of mucus,
and the loss of blood and serum proteins into the intestinal cavity. This causes the
symptoms of dysentery, which include blood and mucus in the stool (bloody diarrhoea);
fever is also common.
|
The effects of Shigella infection on the intestine usually differ from those of
organisms such as enterotoxigenic E. coli and Vibrio cholerae, which cause
watery diarrhoea, without fever. These organisms infect only the small intestine and cause
little or no damage to the cells lining the intestine. Dehydration is the main
complication resulting from these infections. Occasionally Shigella causes only watery
diarrhoea and this will cause dehydration (unless appropriate rehydration fluids are
given). Shigella dysentery may also lead to a number of dangerous complications. These include:
- severe anorexia (loss of appetite)
- hypoproteinaemia (a low concentration of blood protein)
- hyponatraemia (a low concentration of blood sodium)
- dilation of the large intestine
- seizures
- anaemia
- kidney damage
- persistent diarrhoea
- weight loss and malnutrition
Produced by Dialogue on Diarrhoea and the Applied Diarrhoeal Disease Research Project
(ADDR), Harvard Institute for International Development, Cambridge, MA 02138, USA
|
|
DDOnline Shigellosis
supplement to DD44  1 Page 2 3 1 Page 2 3
How can shigellosis be identified?
- Stool culture
The most accurate way to find out if a person with diarrhoea is infected with Shigella
is to make a culture of the stool, to check if the bacterium is present. But this is often
impractical in developing countries. Making a culture is expensive and facilities are
often unavailable in the rural communities and urban slums where the incidence of
shigellosis is greatest. Moreover, the results are usually only available after two or
three days, and treatment should not be delayed - a decision regarding antibiotic use must
be made immediately. Stool microscopy for pus cells to identify shigellosis is not
necessary when visible blood is present in stools. It may help to identify cases of mild
shigellosis, when stools are mucoid without blood, but this is too non-specific to be of
any practical value.
Shigella bacteria are not always found in the stool cultures of children who are infected.
Even in the best conditions, a stool culture may only identify about 70 per cent of those
infected. If antibiotics are given to children with shigellosis before they come to the
clinic, the drugs may eliminate the bacteria from their stools. In most studies that have
been conducted in developing countries, Shigella were recovered from a stool culture in
half or more of all children who had dysentery (see Table 1).
Table 1: Percentage of stool culture showing positive
for Shigella
taken from children with dysentery |
Study site
(community and hospital based) |
Year of study |
Per cent of cases
showing Shigella |
| Dhaka, Bangladesh |
1979 |
55 |
| Nonthaburi, Thailand |
1986 |
44 |
| Rangpur, Bangladesh |
1988 |
50 |
| Bangkok, Thailand |
1991 |
37 |
- Clinical signs and symptoms
The use of clinical signs and symptoms is therefore very important in identifying
patients with shigellosis. Dysentery (bloody diarrhoea) is a very reliable indicator of
the infection in the majority of cases. In many developing countries Shigella infection is
the most common, and potentially the most severe, cause of dysentery. After Shigella, Campylobacter
jejuni and Salmonella are the next most common causes of dysentery, but these
usually produce self-limited illness that is rarely as serious or life-threatening as
shigellosis. The parasite Entamoeba histolytica, responsible for amoebic dysentery,
is a rare cause of dysentery in children, accounting for less than 5 per cent of all
episodes. Stool microscopy for protozoa may not be available and it is often unreliable.
Amoebiasis can only be diagnosed with certainty when trophozoites of E. histolytica containing
red blood cells are seen in fresh stools. The microscopic detection of cysts alone is not
sufficient for a diagnosis of amoebiasis. Treatment of dysentery should therefore focus on
the management of shigellosis. Mothers are usually accurate observers of their children's
stools. If a mother reports that her child's stools contain blood and mucus, then it is
reasonable to assume that the child is infected with Shigella. Many communities have local
terms used to describe different types of diarrhoea, including dysentery, and health
workers should become familiar with these terms.
|
|
DDOnline Shigellosis
supplement to DD44  2 Page 3 4 2 Page 3 4
Treatment of shigellosis in children Children with visible blood in stools should be presumed to have shigellosis and be
treated accordingly. The key components of shigellosis treatment are:
- giving an effective antibiotic
- continued feeding
- replacement of fluid losses
- follow up
Children treated early in their illness with an appropriate antibiotic will be
considerably better 48 hours after therapy has begun. Those who do not receive effective
drug treatment may develop persistent diarrhoea, malnutrition, and other life-threatening
complications. Those who are infected with Shigella who are already malnourished need special
attention, as do infants under 12 months old, and those already dehydrated. The most
severely ill should be cared for in hospital and the others should be followed up at least
once every 48 hours until they are better. Infection of the bloodstream is common in these
patients, and is caused by bacteria, other than Shigella, normally found in the gut. The
signs of bloodstream infection are shock, low urine output and lethargy. Intravenous
antibiotics such as gentamicin and ampicillin should be given in addition to an oral
antibiotic for treatment of shigellosis. However, if ampicillin is given intravenously, it
should not also be given orally.
- Antibiotic treatment
Antibiotic treatment should be started as soon as acute dysentery is identified. The
chosen drug must be safe for use in children and inexpensive; a liquid formulation is
preferable but not essential. Most strains of Shigella in the community must be sensitive
to the drug, and it should have been shown to be effective in controlled clinical trials.
Ampicillin and cotrimoxazole fulfil these criteria, and for the last 15 years have been
the drugs of choice for treatment of shigellosis. Some doctors wrongly prescribe
metronidazole, believing that the drug will cure both shigellosis and amoebic dysentery.
Metronidazole should be used only if E. histolytica has been positively
identified, or if treatment for shigellosis has failed.
|
Table 2: Appropriate
antibiotics for shigellosis
|
| Antibiotic (1) |
Children |
Adults |
Comments |
Cotrimoxazole
(also called trimethoprim (TMP) - sulfamethoxazole (SMX) |
TMP 5mg/kg and SMX 25mg/kg twice a day for 5 days |
TMP 160mg and SMX 800mg twice a day for 5 days |
Not recommended for use in jaundiced and premature infants under 1
month old |
| or: |
| Ampicillin |
25mg/kg 4 times a day for 5 days |
1g 4 times a day for 5 days |
Safe for infants, and pregnant or lactating women |
| Alternative if Shigella in the local area are
resistant: |
| Nalidixic acid |
15mg/kg 4 times a day for 5 days |
1g 3 times a day for 5 days |
Not recommended for infants under two months |
1. All doses are for oral
administration. If a liquid form of the drug is not available for children, give the approximate
dose as crushed tablets.
|
|
Recently, however, resistant strains of Shigella have become common in some countries,
such as Bangladesh. Where resistance to ampicillin and cotrimoxazole exceeds 25 per cent,
nalidixic acid is used as an alternative (see="#Table 2">Table 2). This drug
is more expensive than cotrimoxazole and ampicillin but is similarly effective.
Unfortunately, in areas where nalidixic acid is widely used, Shigella bacteria often
rapidly become resistant. It is important to use these drugs carefully to minimise the
problem of resistance. Their use should be restricted to patients with dysentery: patients
with watery diarrhoea do not require an antibiotic unless cholera is suspected. Health
workers need to know the resistance pattern of Shigella in their community in order to
make the right decision about which drug to use. Stool cultures should be obtained on a
regular basis, and isolates of Shigella tested for sensitivity to drugs commonly used for
treatment. The new fluoroquinolines (e. g. ciprofloxacin and ofloxacin) are highly active and
clinically effective when given by mouth, but because they cause cartilage damage in young
animals, there is still concern about their safety in young children. Studies are being
carried out to determine how important this is in humans. Antibiotics known to be less
effective and therefore not recommended include neomycin, gentamicin, the first generation
cephalosporins, kanamycin, amoxycillin and sulphaguanidine. In many parts of the world, a
significant proportion of Shigella strains show in vitro sensitivity to
furazolidine and many doctors who use it as initial therapy in India report anecdotal
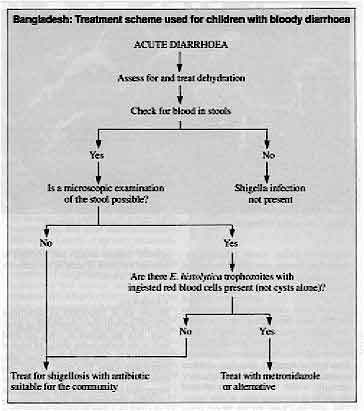
favourable results. However, controlled clinical trials are lacking. The diagram below shows a scheme which was developed for health workers to use when
treating children with bloody diarrhoea in Bangladesh. Similar schemes could be
established and evaluated for other countries.
|
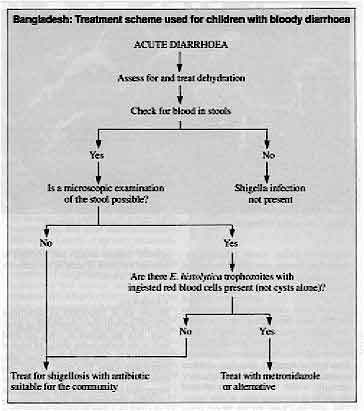 |
Bangladesh: Treatment scheme used for children with bloody diarrhoea
ACUTE DIARRHOEA
- Assess for and treat dehydration
- Check for blood in stools
- Yes No
- Is a microscopic examination of the stool possible?
- Shigelli infection not present
- No Yes
- Are there E. histolytica trophozoites with ingested red blood cells present (not
cysts alone)?
- No Yes
- Treat for shigellosis with antibiotic suitable for the community
- Treat with metronidazole or alternative
|
|
DDOnline Shigellosis
supplement to DD44  3 Page 4 3 Page 4
- Continued feeding
Nutrient absorption continues during shigellosis, because the disease does not affect much
of the small intestine, where most absorption takes place. However, the inflammation in
the large intestine affects nutritional status. Early effective antimicrobial therapy
cures the infection and inflammation and the child's appetite will return, soon followed
by weight gain. It is important to feed and/or breastfeed patients with shigellosis
frequently to prevent them developing hypoglycaemia (low blood sugar) and losing weight
during their illness. This can be difficult because they are often severely anorexic
(suffering from loss of appetite). However, children need not eat as much at each feeding
as they normally would. Small amounts of food should be given every three to four hours.
This will also keep up the blood sugar level. Foods rich in potassium, such as bananas,
are recommended. One extra meal should be given to the child every day for at least two
weeks after the diarrhoea stops.
Continued feeding also helps to prevent the acute weight loss that occurs during
diarrhoea. If a severely ill patient in hospital refuses to eat or to breastfeed, it may
be necessary to feed with a nasogastric tube initially.
- Replacement of fluid losses
Mild to moderate dehydration is common in patients with shigellosis. Dehydration is
caused by loss of fluid in stools, evaporation of water through the skin due to fever, and
reduced fluid intake because of anorexia. Hyponatraemia (low levels of sodium in the
blood) is a particular problem for those infected with S. dysenteriae type
1. Oral rehydration therapy should be given and in most cases fluids do not need to be
given intravenously. Giving intravenous fluids increases the risk of infection and is
expensive. Oral rehydration solution contains enough salt (sodium) to increase the level
of salts in the patient's blood, if it is low.
- Follow up
Follow up is important to determine whether patients have responded to treatment. Ask the
mother to bring her child back to the health centre within 48 hours if the child is less
than one year old, dehydrated when first seen, or still has blood in the stool. Diarrhoea
may take longer than two days to stop altogether, but the visible blood in stools should
disappear within that time. If the blood does persist, the child may be infected with a
strain of Shigella that is resistant to the drug used. Such patients should be treated
with a different agent for shigellosis unless another cause of dysentery is found. If
there is still no improvement after two days of treatment with an alternative drug, the
child should be taken to hospital. Amoebiasis should be considered.
How can shigellosis be prevented?
Shigella bacteria infect only humans and monkeys, and do not survive for long outside
the body. Therefore, for infection to occur, Shigella bacteria must pass quickly from one
person to another. This usually occurs through 'faecal-oral' transmission. This takes
place when a person with shigellosis defecates, does not wash his or her hands adequately
afterwards, and transfers Shigella germs to food (or water). The bacteria are then
swallowed when the contaminated food is eaten by another person.
 |
Handwashing after defecation is the best way to prevent the
spread of shigellosis.
Fewer than ten ingested bacteria are enough to cause a Shigella infection; in contrast,
thousands of Vibrio cholerae are required to cause disease.
|
Once a member of the family has dysentery, infection can spread from person to person
very quickly. Community health education must include information on hygiene. The most
effective way to reduce the incidence of shigellosis is to ensure proper washing of hands
following defecation, and adequate disposal of faeces. It is not only adults who need to
wash their hands. Children are probably the most common carriers of infection, and they
must also be shown how to wash their hands. Adults caring for children need to wash their
hands often too. Even if soap is not available, a good scrubbing with water, and use of an
abrasive such as sand, is helpful in reducing the spread of infection. Household food and
water also have to be protected from faeces and unwashed hands. There are no effective
vaccines for the prevention of shigellosis, although research into vaccines, especially
ones for oral use, is being carried out.
Steps to eradication Of all the diarrhoeal illnesses, shigellosis is the one most closely linked with
underdevelopment. Features of underdevelopment that produce a high incidence of
shigellosis include poor housing and insanitary conditions, overcrowding, absence of
adequate water supplies for cleaning and washing, and childhood malnutrition. In all
countries where economic and social conditions have improved, the most virulent forms of
shigellosis, caused by Shigella dysenteriae type 1 and Shigella flexneri, have
virtually disappeared. Thus the prevention of shigellosis is closely linked to efforts to
improve the economic and social conditions of people living in areas where shigellosis is
now endemic. On a national level, Diarrhoeal Disease Control Programmes need to research patterns of
antibiotic use, investigate resistance of Shigella strains to drugs in different regions,
develop treatment schemes appropriate for local conditions, and train doctors in the
correct case management of dysentery. Acknowledgements This supplement is based on material prepared by Drs M Bennish and J Griffiths of
the New England Medical Center (Tufts University), Dr A Salam of the International Centre
for Diarrhoeal Disease Research, Bangladesh and Dr M Bhan, of the All-India Institute of
Medical Sciences, New Delhi, India; and developed by the ADDR Project, Harvard Institute
for International Development.
Produced by Dialogue on Diarrhoea, AHRTAG, UK, and the Applied Diarrhoeal Disease
Research Project (ADDR). Harvard Institute for International Development, Cambridge, MA
02138. USA
|
Shigellosis
Clinical Update - A supplement to Issue no. 44 March 1991
Page Navigation
This edition of Dialogue on Diarrhoea Online is
produced by Rehydration Project.
Dialogue on Diarrhoea was published four times a year in English,
Chinese, French, Portuguese, Spanish, Tamil, English/Urdu and Vietnamese and
reached more than a quarter of a million readers worldwide.
The
English edition of Dialogue on Diarrhoea was produced and distributed by
Healthlink
Worldwide.
Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any
uses made of the material.
|
updated: 4 March, 2016
updated: 4 March, 2016
|
version of this Issue