|
| |
Diarrhoea and Drugs
Health Update: A supplement to Issue no. 50 - September 1992
pdf  version
of this Issue version
of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-4 Diarrhoea and Drugs
A supplement to Dialogue on Diarrhoea Online Issue
50 - September 1992
|
DDOnline Diarrhoea
and Drugs supplement to DD50  Page 1 2
Page 1 2
Health Update DIARRHOEA AND DRUGS Despite widespread knowledge for the last 20 years that a simple oral rehydration
solution can prevent most deaths from acute watery diarrhoea, many doctors and pharmacists
continue to prescribe ineffective and expensive drugs. This DD insert reviews
research into prescribing practice and what can be done to change it.
|
Doctors and pharmacists continue to offer parents a wide range
of useless and sometimes dangerous drugs to treat diarrhoea.
Over-use of drugs for childhood diarrhoea is an important problem, detracting from use
of oral rehydration therapy (ORT) and costing money that could be better spent on other
things.
|
 |
In Lima, Peru, for example, medications and visits to the doctor because of childhood
diarrhoea cost on average a tenth of the monthly wage of poor families. If private doctors
are used, the cost rises to more than one third of the monthly wage (1) The vast majority of medications given for childhood diarrhoea are not only
ineffective, they can also be dangerous (2) (see="#Guidelines">guidelines below). Despite this, a variety of antibiotics and
'anti-diarrhoeal' preparations are prescribed by pharmacists and doctors, usually instead
of ORT (3). Reasons for drug use To try to understand why drugs are over-used and to change these ineffective treatment
practices, the Applied Diarrheal Disease Research (ADDR) project has funded 17 research
studies. These studies reviewed the practices of doctors, pharmacists, drug sellers and carers
of children. Seven are complete, two are in the final stages of analysis, and eight are
still collecting data. Study results have shown that there are important reasons for the apparently
'irrational' use of drugs. For example, childhood diarrhoea causes mothers additional work
and worry. They want it to stop quickly. They believe that pills and injections will give
speedy results. Such medicines are easily available and are thought to be the modern way
to cure illness. Health professionals are taught during training that diarrhoea often has a bacterial
cause, and that it is better to treat possible causes than to worry about antibiotic
resistance. Pharmaceutical company representatives often make regular visits to inform
doctors about new products and to encourage them to prescribe more medications. Mothers
ask for medicines for their children, and doctors report that if they do not give a
prescription they risk losing their patient. Finally, in many countries, sales of ORS (oral rehydration salts) packets give lower
profits than sales of antibiotics and anti-diarrhoeal drugs. In some countries, ORS
packets are distributed free of charge and pharmacists have no incentive to sell them. All
these factors must be taken into consideration when designing interventions that aim to
change prescribing and treatment practices.
|
Guidelines for correct use of drugs
- Antimicrobial drugs should be given only for dysentery (bloody diarrhoea) and suspected
cholera with severe dehydration. Inappropriate use of anti-microbials can kill off useful
gut bacteria and may lead to the development of resistant strains of bacteria. They can
also have toxic effects and cause allergic reactions.
- Anti-parasitic drugs should be used only for proven and symptomatic amoebiasis and
giardiasis.
- Anti-diarrhoeal drugs such as loperamide and diphenoxylate have no proven practical
value in reducing diarrhoeal fluid losses in children. They can have dangerous side
effects, for example depressing breathing and contributing to severe abdominal distension.
- Antispasmodics are only partly effective in inhibiting bowel contractions and should not
be used.
- Although adsorbents such as kaolin and pectin, charcoal and attapulgite can change stool
consistency, they do not decrease fluid losses and can reduce the effectiveness of other
drugs.
See DD42, 43 ,44
and 45 for more information on the use of drugs in treating
diarrhoea.
|
Produced by Dialogue on Diarrhoea and the Applied Diarrheal Disease
Research Project (ADDR). Harvard Institute for international Development. Cambridge, MA
02138. USA
|
|
DDOnline Diarrhoea
and Drugs supplement to DD50  1 Page 2 3 1 Page 2 3
What happens in practice?
Six studies have shown that drugs are the most common treatment for diarrhoea.
Many families buy antibiotics without seeking medical advice. Even when doctors or
pharmacists are consulted, they also recommend drugs more often than ORT - despite knowing
better. Families often combine modem medical treatment - ORT and drugs - and traditional
practices - changes in feeding, use of teas and herbal remedies - to manage childhood
diarrhoea. For example, buying a few capsules of tetracycline from a shop or a stall is
becoming as common a response to illness as giving herbal teas. Three studies in Nigeria, Thailand and Indonesia show that medications are frequently
used by families to treat childhood diarrhoea. Family response In Nigeria, a one year community based surveillance of 351 poor urban
households, measured diarrhoea episodes and reported treatment (4). It
found that ORT was used during only 15 per cent of the days that children had diarrhoea.
Antibiotics, however, were used on over half the days when children had diarrhoea. Among
the households using antibiotics, over half bought them without seeking medical advice. In Thailand, a six month diarrhoea surveillance study of 254 children under five
(5) identified 80 diarrhoea episodes. Pills or liquid medicines were
given in 91 per cent of episodes, but ORT was given in only 51 per cent. Other treatments
given included injections (28 per cent) and herbal medicines (20 per cent). This study
also asked parents how satisfied they were with these various forms of care. Very few (4
per cent) considered ORT the most important treatment for diarrhoea, while 60 per cent
considered pills or liquid medicines as most useful and 10 per cent believed injections
were best. Interviews in Indonesia with mothers of children under two admitted to hospitals
or health centres with diarrhoea, showed that half of the mothers had been given drugs to
treat their children. Although 68 per cent of mothers reported giving ORT to their
children, this was mostly home made sugar salt solution (SSS), which only 12 per cent of
mothers were able to make properly (6). Health workers' advice
The problem of inappropriate drug use in the community is paralleled by the
inappropriate prescription and sale of medications by doctors, pharmacists, and drug
sellers. Studies in Peru, Indonesia, and Nigeria show that drugs are prescribed more often than
ORT, and that practice can be quite different from what health workers say they do. In Peru, doctors prescribed drugs more often and ORT less often than they said
they did. A researcher interviewed 148 doctors about their practices, and observed 620
children being treated by them. Fifty-nine per cent of the children were prescribed
antibiotics, while only 26 per cent of the physicians reported that they prescribed
medications of any type. ORT was recommended in 54 per cent of cases, while 74 per cent of
doctors reported recommending some type of ORT. Instructions for how to use ORT
accompanied recommendations in only one in four cases (7). Similarly, in Indonesia, more doctors actually prescribed antibiotics and
anti-spasmodics than reported doing so, and slightly fewer prescribed ORT or adsorbents
than reported doing so (8). Doctors treating patients in government hospitals prescribed
more ORT (59 per cent of cases) than doctors treating patients privately (38 per cent of
cases). Even when ORT was prescribed. it was usually used after intravenous rehydration or
in conjunction with antibiotics. Doctors were most concerned about the possibility of
bacterial or viral infection causing the diarrhoea, and less concerned about dehydration.
Almost half the doctors in the study believed that ORS was unacceptable to their patients
because of its taste or colour.
|
A Nigerian study showed a vast difference between what
pharmacists and drug sellers said and their actual practice.
In north-east Nigeria (9) there were dramatic
differences between what pharmacists and drug sellers said and what they did. Research
assistants, posing as parents of children with diarrhoea, described standardised diarrhoea
cases to pharmacists or drug sellers and purchased the recommended remedies. The results
were compared with what the pharmacist or drug seller said they did.
|
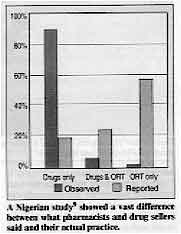 |
Almost all the respondents were observed to prescribe drugs only, although fewer than
20 per cent reported doing so. Almost 60 per cent reported prescribing ORT only, while
only 2 per cent were observed to do so. Knowledge not the key
The behaviour in these studies was not a result of lack of knowledge. Many health
professionals appeared to know that they should be prescribing more ORT and fewer
medications for childhood diarrhoea. At least they knew that was the 'correct' answer to
give to an interviewer. Providing them with more information may not be enough to change
their behaviour. There is also an important lesson in research methods here. Actual drug prescribing
behaviour in these studies is quite different from what is reported. Interviewing is,
therefore, not a reliable way to measure professional prescribing practices or to evaluate
the effects of interventions to change prescribing behaviour. Observation of actual
practice, or review of prescribing records, is essential. Doctors often say that they prescribe drugs because patients ask for them. This
explanation was tested by a study in Peru in which doctors were visited by mothers who had
been trained either to demand medicine or not to ask for it. The doctors did not prescribe
differently for the two groups of mothers. Patient demand for drugs was not an important
factor.
|
|
DDOnline Diarrhoea
and Drugs supplement to DD50  2 Page 3 4 2 Page 3 4
How can we change behaviour? The widespread use of drugs for treating diarrhoea is clearly a major problem. How
can prescribing practices be changed, so that doctors, pharmacists and drug sellers
emphasise the use of ORT to prevent dehydration and reduce the use of inappropriate
antibiotics and other drugs? Methods of changing behaviour can be grouped into four categories: educational,
regulatory, managerial and financial (see="dd45.htm#page6">DD45 page 6).
Three recently completed studies, two in Mexico and one in Thailand, looked at using
educational and managerial techniques to change prescribing behaviour. Three other ADDR
supported studies of behaviour change are underway. Doctors' review group
Two techniques were used very successfully in Mexico. A workshop was held for a
group of doctors to review guidelines for treating cases of acute diarrhoea in children.
The doctors were later brought together for a weekly review of the cases they had treated
(10).
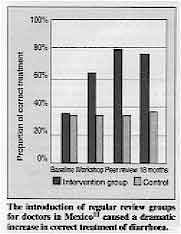 |
The introduction of regular review groups for doctors in Mexico(11) caused a dramatic increase in correct treatment of diarrhoea. Before the intervention, only a third of the doctors treated diarrhoea patients
appropriately: recommending ORT; advising mothers to continue feeding children: and
prescribing drugs only for Shigella and amoebic dysentery. Eighteen months later, 74 per
cent of doctors participating in the weekly review were treating cases appropriately (11).
|
In a control group of doctors from a similar background to those taking part in the
review there was very little change in treatment practice over the same period, with only
about a third of them (35 percent) treating cases appropriately. The study was then expanded to include 18 clinics in a district of Mexico City. Early
results were similar to the first study. The proportion of patients treated appropriately
increased from 12 per cent to 45 per cent in Social Security System (IMSS) clinics, and
from 13 per cent to 43 per cent in Ministry of Health clinics. IMSS control clinics which
did not receive the intervention showed no significant changes in practice over time,
while at Ministry of Health control clinics, the proportion of patients treated
appropriately decreased from 16 per cent to 11 per cent (12). Overall, the results were so positive that the IMSS has decided to adopt the
intervention in the state of Tlaxcala. If this is successful, IMSS, which provides health
care to more than 60 per cent of Mexicans. will adopt the same approach throughout the
country.
 |
Pharmacists need to be convinced that their job is to advise
appropriate treatment for diarrhoea - ORT to prevent dehydration - rather than to
recommend expensive drugs. |
Educational messages In Thailand an intervention aimed at pharmacists and drug sellers was not so
successful (13). One group of participants was educated in large groups about ways to improve
prescribing practice. Another group was given educational messages by telephone. Each
group received the same printed materials. Before the intervention about a third of
pharmacies prescribed ORT: 82 per cent prescribed antibiotics; and 76 per cent prescribed
anti-diarrhoeals. After the intervention the same proportion still prescribed ORT. Eighty
per cent of the pharmacies continued to prescribe antibiotics, while 77 per cent still
prescribed anti-diarrhoeals. Prescribing levels at control pharmacies were not
significantly different. The results suggest that the educational intervention was not successful in bringing
about behaviour change. However, because the campaign was directed at head pharmacists and
main drug sellers in the shops studied. it may not have reached all the people who sell
drugs in those outlets. Further studies are underway in Indonesia to compare face-to-face teaching methods with
teaching in large groups. These studies will also look at different ways of educating
urban doctors and owners of small shops. It is hoped that the studies will help policy
makers to decide which groups of health workers are easiest to influence and which methods
are most effective.
|
|
DDOnline Diarrhoea
and Drugs supplement to DD50  3 Page 4 3 Page 4
What is the way forward?
More information is needed about the motivation of doctors and pharmacists, and
how community expectations of health professionals can be changed. Changing inappropriate drug use is a complex issue. It is important that we understand
the habits and motivations of all the people involved in treating diarrhoea (doctors,
pharmacists, drug sellers and family members who buy drugs without seeking medical
advice). Studies supported by ADDR are currently looking at:
- pharmacists' prescribing practices and community drug use in Lima, Peru
- the factors influencing doctors' prescribing practices in Lima
- doctors' prescribing habits in Pakistan
- community drug use in Lahore, Pakistan.
Future ADDR studies may look at questions such as:
- What role does patient demand play in influencing a doctor's or pharmacist's prescribing
practices?
- What part do economic incentives play?
- How great is the public health risk of over-use of antibiotics as compared with
anti-diarrhoeals?
Enough is known already to predict some interventions which are most likely to be
effective in changing prescribing practice. Important factors include:
- involvement of the prescribers themselves in formulating policy for change
- use of different materials and messages for different audiences
- educational materials designed with the motivation of the target audience in mind.
Understanding motivation
Researchers need to develop more creative strategies to understand behaviour. Health
workers need to pay more attention to the public health impact of their actions. They have
to make sure their patients understand that a 'good doctor' is not defined simply by how
many drugs he or she prescribes. Parents of children with diarrhoea need to have a new image of what good doctors or
pharmacists prescribe. Strategies for changing their views need to be developed. Looking beyond diarrhoea These studies emphasise that drug use is a barrier to proper management of most kinds
of diarrhoea. Many illnesses apart from diarrhoea, such as malaria and acute respiratory
infections, are also common in developing countries. People use drugs for these illnesses
too. If people reduce the use of drugs for diarrhoea, will they increase their use of
drugs for other illnesses? Would community campaigns to change drug use just for diarrhoea
have less impact than campaigns to change drug use for other diseases as well? We do not
yet know the answers to these important questions. These studies should also raise concerns about what people want from their doctors and
pharmacists. Are patients most interested in receiving a diagnosis, advice, or a
prescription? People often think they will get well more quickly if they receive a pill or
an injection. Professionals know this, and they know they can see more patients if they
spend more time prescribing drugs and less time diagnosing and educating. How then can
doctors and pharmacists help education and ORT to become acceptable substitutes for drugs? Established practice
These questions are relevant not only to the treatment of diarrhoea. They involve
fundamental issues about how professionals should practise medicine, and what happens when
'proper case management' seems to interfere with established routines, take more time, and
bring in less money. Finally, these studies also remind us that we know little about how professionals
establish their own treatment habits and later maintain them. How important are training,
peer pressure, pharmaceutical representatives, continuing education and patient pressure
at different times during a professional's career? Will a newly qualified doctor respond
to the same message as one who has been practising for 30 years? Answers to these questions will allow more effective interventions to be designed to
improve treatment of diarrhoea as well as other diseases, This supplement is based on material prepared by Drs James Trostle and Jonathan
Harrington of ADDR, which is funded by USAID. References 1. Paredes P et al., 1992. The abuse of medication use during
diarrhoea in children. Paper presented at a meeting organised by the Institute for
Nutrition Research, Lima, Peru (in Spanish).
2. WHO, 1990. The rational use of drugs in the management of acute
diarrhoea in children. Geneva: WHO.
3. Harris S, Black R, 1991. How useful are pharmaceuticals in
managing diarrhoeal diseases in developing countries? Hlth. Policy Planning 6: 141-147.
4. Oni G, et al., 1991. Diarrhoeal disease morbidity, risk factors
and treatments in a low socioeconomic area of Ilorin, Kwara State, Nigeria. J. Diarr Dis.
Res. 9: 250-257.
5. Choprapawon C, et al., 1991. Cultural study of diarrhoeal
illnesses in central Thailand and its practical implications. J. Diarr Dis. Res. 9:
204-212. (Reported in="dd48.htm#page3">DD 48: 3.)
6. Muninjaya AA, et al., 1991. Home treatment of acute diarrhoea in
Bali, Indonesia. J. Diarr Dis. Res. 9: 200-203.
7. del Aguila R, 1989. Prácticas médicas en el tratamiento de
diarrea infantil. In Medicamentos Inapropriados en Diarrea: La Magnitud del
Problema.
Colección Cienttfica I: 34-40. Organización Panamericana de la Salud, Lima, Peru.
8. Gani L, et al., 1991. Physicians' prescribing practice for
treatment of acute diarrhoea in young children in Jakarta. J Diarr Dis Res 9: 194-199.
(Reported in="dd44.htm#page5">DD 44: 5.)
9. Igun U. 1991. Prescribing practices for diarrhoeal
diseases by formal and unlicensed pharmacies in Borno State, Nigeria. Final report
submitted to the ADDR Project, December
10. Gutiérrez G, et al., 1988. Conclusiones y
perspectivas. Arch.
Invest. Med. Mex. 19: 437- 444. (Reported in="dd43.htm#page3">DD 43: 3.)
11. Gutiérrez G, et al., Changing physician prescribing patterns:
evaluation of an educational strategy for acute diarrhoea in Mexico City. Submitted for
publication.
12. Guiscafré H. Personal communication.
13. Varavithya W, et al., 1991. Impact of an education program on
the knowledge and treatment practices of diarrhoeal diseases among pharmacists and
drugsellers. Final report submitted to ADDR.
Produced by Dialogue on Diarrhoea and the Applied Diarrheal Disease Research Project
(ADDR). Harvard Institute for International Development. Cambridge. MA 02138. USA
|
Diarrhoea and Drugs
Health Update - A supplement to Issue no. 50 September 1992
Page Navigation
This edition of Dialogue on Diarrhoea Online is
produced by Rehydration Project.
Dialogue on Diarrhoea was published four times a year in English,
Chinese, French, Portuguese, Spanish, Tamil, English/Urdu and Vietnamese and
reached more than a quarter of a million readers worldwide.
The
English edition of Dialogue on Diarrhoea was produced and distributed by
Healthlink
Worldwide.
Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any
uses made of the material.
|
updated: 4 March, 2016
updated: 4 March, 2016
|
version of this Issue