|
| |
Controlling Cholera
Health Update: A supplement to Issue no. 52 - March-May 1993
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-6 Controlling Cholera
A supplement to Dialogue on Diarrhoea Online Issue 52
- March-May 1993
|
DDOnline Controlling
Cholera supplement to DD52  Page 1 2
Page 1 2
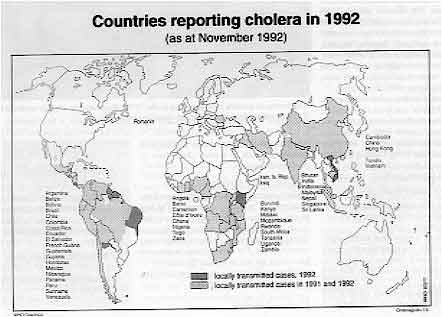
HEALTH UPDATE CONTROLLING CHOLERA The current cholera pandemic started in 1961 and shows no sign of ending. Although
much is being done to ensure that communities respond quickly and effectively to the
threat, longer term measures are needed to prevent its continued spread. This DD
insert looks at the latest trends, and provides guidelines on treatment and prevention.
|
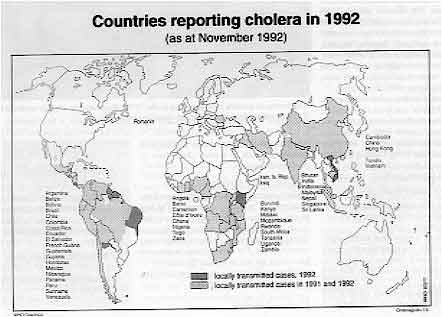
The horror of cholera in Bangladesh in the 1970s. However, the
disease need not be a killer if simple prevention and treatment measures are taken.
Cholera continues to spread throughout the
world. It is gaining a stronger foot-hold in places where it has been present for years,
as well as appearing in new areas.
|
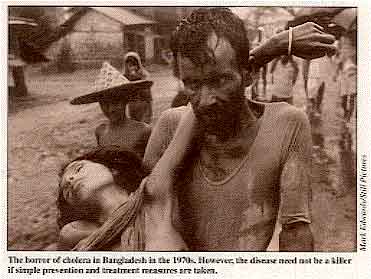 |
In Latin America. cholera appeared for the first time this century. in Peru in 1991. It
then spread rapidly throughout the continent. By the end of 1991 nearly 300,000 cases had
been reported (1). New outbreaks have recently occurred in Argentina and
Paraguay. The encouraging news. though, is that the mortality rate has been very low -
around 1 per cent (2). Recently cholera has taken its greatest toll in Africa. The disease swept across
southern Africa in the second half of last year. Large numbers of cases were reported in
Angola, Swaziland, Zambia, Malawi, Tanzania and Mozambique. In Zimbabwe, which had not
been affected by cholera since 1985, more than 4,000 cases were reported in the space of
three months. Although the total number of cases reported in Africa is much less than in the Americas
(3), the death rate is a lot higher - averaging 9 per cent in 1991. The
reasons for this have not been proven, but three possible causes are being investigated:
- less access to effective health care in Africa compared with Latin America
- not enough trained health personnel
- the fatality rate may be exaggerated because only the most severe cases are coming to
health centres.
Health planners believe that unlike other cholera outbreaks, this latest pandemic will
not go away. Instead, cholera is expected to become endemic in the Americas, as it has in
Africa. It is difficult to say where cholera will strike next, or how long it will remain a
problem. But despite these unanswered questions, much is known about how to prevent and
treat it. Prevention and treatment Cholera treatment is not very different from treatment of 'ordinary' diarrhoea. The key
is oral rehydration therapy. However. because dehydration can happen rapidly, it is
sometimes necessary to begin rehydration intravenously. For severe cases, antibiotics have
been shown to reduce the duration of diarrhoea. (See="#Antibiotic treatment">below
for more detailed guidelines.)
|
DEFINITIONS
- Endemic: a disease continually present in a region
- Epidemic: an outbreak of a disease, introduced from outside a community, which
attacks many people over a short period of time
- Pandemic: an extensive epidemic which affects the populations of several
countries or regions
|
|
DDOnline Controlling
Cholera supplement to DD52  1 Page 2 3 1 Page 2 3
Effective prevention methods are also the same as for other forms of
diarrhoea:
- provision and use of clean drinking water
- handwashing
- good home and environmental hygiene and sanitation
- avoidance of potentially contaminated foods
Common, but ineffective. prevention measures include:
- vaccination
- giving antibiotics to large numbers of people w are not sick
- restricting the movement of people (e. g. quarantine or 'cordon
sanitaire')
- restricting food imports from affected areas
Trying to enforce these measures takes attention away from the simple and effective
methods mentioned earlier. Cholera's reputation as a killer has been earned over the centuries, but modern
advances mean we now have the scientific and public health solutions. However, the
conditions which enable cholera to be spread - lack of knowledge, poverty and social
inequity - also need to be challenged. The key to eliminating cholera, as for other diseases linked to underdevelopment, lies
in improved education and communication systems, adequate and safe water supplies,
provision of sanitation systems, effective public health programmes and availability of
treatment Dr Ronald Waldman, CDD, WHO, CH-1211 Geneva 27, Switzerland. 1. 391,220 cases. WHO figures. The figures for 1992 were not
compiled at the time of publication.
2. 4,002 deaths
3. 153,367 cases in 1991
|
FACT FILE
- 90 per cent of cholera cases are mild. Many infected people have no symptoms, but can be
carriers and infect others.
- Even in a cholera outbreak, more children die from other types of diarrhoea.
- The main danger from cholera is rapid dehydration. It must be treated quickly. Unless
patients receive rehydration they can die, sometimes in a few hours.
- Most cholera cases can be treated successfully with oral rehydration therapy. However,
the few that become severely dehydrated need intravenous fluid initially
and antibiotic treatment.
- Neither vaccination, quarantine, nor travel restrictions prevent cholera from spreading.
- In the long term, improved water supply, sanitation and hygiene, and better living
conditions are crucial to preventing cholera.
|
|
DDOnline Controlling
Cholera supplement to DD52  2 Page 3 4 2 Page 3 4
How to assess and treat cholera patients
A step-by-step guide to diagnosis and management Cholera should be suspected when: a child over five or an adult develops severe dehydration from acute watery diarrhoea
or
anyone over two years old has acute watery diarrhoea in an area where there is an
outbreak of cholera. (Cholera may attack children under two, but this is unusual.)
STEP 1
Assess for dehydration The table below can be used to assess whether a patient is dehydrated. 'Some
dehydration' or 'severe dehydration' can be diagnosed if the patient has two or more signs
in the appropriate column. In the case of 'some dehydration' or 'severe dehydration', this
should include at least one of the signs in the coloured box.
|
Assessment of the diarrhoea patient for
dehydration |
| |
NO DEHYDRATION |
SOME DEHYDRATION |
SEVERE DEHYDRATION |
| CONDITION |
Well, alert |
Restless, irritable |
Lethargic or
unconscious, floppy |
| EYES |
Normal |
Sunken |
Very sunken and dry |
| TEARS |
Present |
Absent |
Absent |
| MOUTH & TONGUE |
Moist |
Dry |
Very dry |
| THIRST |
Drinks normally, not thirsty |
Thirsty, drinks
eagerly |
Drinks poorly or not
able to drink |
| SKIN PINCH |
Goes back quickly |
Goes back
slowly |
Goes back very
slowly |
|
STEP 2 Rehydration FOR SEVERE DEHYDRATION
- Give IV fluid immediately. Use Ringer's lactate solution or, if not available,
normal saline.
- For patients older than one year, give l00ml/ kg over three hours (30ml/kg within the
first half hour, then 70ml/kg in the next two-and-a-half hours).
- For infants under one year old, give l00ml/kg over six hours (30ml/kg in the first hour,
then 70ml/kg over the next five hours).
- Monitor the patient frequently. After the initial 30ml/kg has been given, the
pulse (taken at the wrist) should be strong. If the pulse is not yet strong, continue to
give IV fluid rapidly.
- Give ORS solution (about 5ml/kg/hour) in addition to IV fluid as soon as the
patient can drink.
- Reassess the patient after three hours (or six hours in the case of infants).
- If there are still signs of 'severe dehydration' (this is rare) repeat the IV therapy.
- For signs of 'some dehydration', continue as indicated below.
- If there are 'no signs of dehydration', go on to STEP 3.
FOR SOME DEHYDRATION
- Give ORS solution according to the amount recommended in the table below. If the
patient passes many watery stools or wants more ORS solution, then give more.
|
Approximate amount of 0RS solution to
give in the first 4 hours |
| AGE (1) |
WEIGHT |
ORS SOLUTION |
| Less than 4 months |
Less than 5kg |
200-400ml |
| 4-11 months |
5-7.9kg |
400-600ml |
| 12-23 months |
8-10.9kg |
600-800ml |
| 2-4 years |
11-15.9kg |
800-1200ml |
| 5-14 years |
16-29.9kg |
1200-2200ml |
| 15 years or more |
30kg or more |
2200-4000ml |
1 Only use a patient's age if you do not know
their weight.
- Monitor the patient frequently to ensure that ORS solution is being taken and to
identify those passing frequent watery stools, who will require closer monitoring.
- Reassess the patient after four hours. If the patient has developed 'severe dehydration'
(this is rare), rehydrate with IV fluid as described earlier. If there is still 'some
dehydration', continue to give ORS solution at the same rate and start to offer food and
other fluids. If there are 'no signs of dehydration', go on to STEP 3.
NO SIGNS OF DEHYDRATION Patients first seen with 'no signs of dehydration' can be treated at home.
- Give ORS packets to take home. Give enough for two days. See="dd52.htm#page7">DD
page 7 7 for guidelines on how much ORS solution to administer.
- Instruct the patient or caregiver to return if any of the following signs develop:
- Passing many watery stools
- Eating or drinking poorly
- Marked thirst
- Repeated vomiting
- Fever
- Blood in stool
|
|
DDOnline Controlling
Cholera supplement to DD52  3 Page 4 5 3 Page 4 5
STEP 3
Maintain hydration
When a patient who has been rehydrated using IV fluid or ORS solution no longer shows
signs of dehydration, continue to give ORS solution to maintain normal hydration. As a guide, give the patient:
Approximate amount of ORS solution to give to
maintain hydration |
| AGE |
AMOUNT OF ORS SOLUTION AFTER EACH LOOSE STOOL |
| less than 24 months |
l00ml |
| 2-9 years |
200ml |
| 10 years or more |
As much as wanted |
- Continue to reassess the patient for signs of dehydration at least every four
hours to ensure enough ORS solution is being taken.
A few patients whose stool output is very large may have difficulty in drinking enough
ORS solution. If such patients become tired, vomit frequently or develop abdominal
distension, ORS solution should be stopped and hydration maintained intravenously until
the rate of stool output slows. Source: WHO, 1992. Management of the patient with cholera. STEP 4
Antibiotic treatment An effective antibiotic can reduce the volume and duration of diarrhoea in patients
with severe cholera. It will usually stop the diarrhoea within 48 hours. Antibiotics
should only be used for patients who develop severe dehydration. Over-use of antibiotics
can lead to the development of resistant strains of bacteria. If the patient is severely dehydrated, over two years old and cholera is suspected,
give an antibiotic. Start the antibiotic after the patient has been rehydrated (usually in 4-6 hours) and
vomiting has stopped. There is no advantage in using injectable antibiotics, which are expensive. No drugs
other than those described in the next column should be used to treat cholera. Doxycycline is the antibiotic of choice for adults (except pregnant women)
because only one dose is required. Tetracycline is just as effective, but must be
given for three days. Trimethoprim-Sulfamethoxazole (cotrimoxazole) is the antibiotic of choice for
children below 12 years. Tetracycline is equally effective; however in some
countries it is not available for paediatric use because in large doses it can cause
staining of children's teeth. Furazolidone is the antibiotic of choice for pregnant women. Erythromycin or chloramphenicol may be used when the antibiotics listed above
are not available, or where Vibrio cholerae O1 is resistant to them.
|
Antibiotics used to treat cholera |
| ANTIBIOTIC |
CHILDREN |
ADULTS |
Doxycycline
a single dose |
|
300mg |
Tetracycline
4 times a day for 3 days |
12.5mg/kg |
500mg |
Cotrimoxazole
(Trimethoprim -TMP
Sulfamethoxazole -SMX)
twice a day for 3 days |
TMP 5mg/kg and
SMX 25mg/kg |
TMP 160mg and
SMX 800mg |
Furazolidone
4 times a day for 3 days |
1.25mg/kg |
100mg |
|
STEP 5 Feed the patient
- Resume feeding with a normal diet after the patient is fully hydrated and
vomiting has stopped.
- Continue breastfeeding infants and young children.
|
|
DDOnline Controlling
Cholera supplement to DD52  4 Page 5 6 4 Page 5 6
The low fatality rate in Peru
The appearance of cholera in Latin America two years ago caused alarm among health
workers. However, the good news is that fatality rates have been low. Enrique
Jacoby and Bruno Benavides review possible reasons
for the low death rate in Peru.
|

|
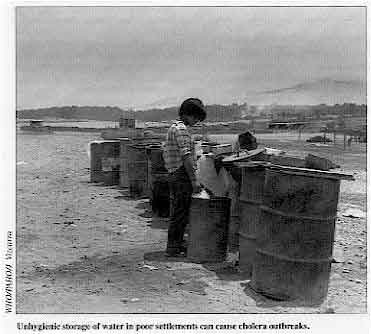 |
Unhygienic storage of water in poor settlements can cause
cholera outbreaks.
A hot summer and a water shortage along
Peru's coastal strip proved to be a fatal combination in early 1991, providing the setting
for Latin America's first cholera outbreak this century.
|
The cholera-causing organism, Vibrio cholerae 01, appeared simultaneously in
three coastal cities. An explosive epidemic followed, affecting all the major cities and
later spreading to rural areas. Five months later 200,000 cases had been reported. But, despite the fact that Peru had
no recent experience of treating cholera, the death toll was surprisingly low - on average
1 per cent of reported cases. The information available showed high attack rates and low fatalities in the cities,
and the opposite in rural areas - lower rates of illness, but higher mortality. We tried
to learn what caused these differences. First, we looked at access to health facilities to see whether that affected the
fatality rate. Surveys of two urban areas with low death rates, the northern city of Piura
and the capital, Lima, showed that about 90 per cent of people with cholera went to a
health facility. A study in the Amazon region showed that villages with poor access to
health services had the highest death rates. A second possible explanation was tested. Some health planners believed that home use
of oral rehydration salts (ORS) solution helped to reduce the death toll. We conducted a
case-control study among patients registered in the main hospitals in two cities. Piura
and Sullana, comparing the home use of ORS solution among cholera survivors and those who
died. We found no significant differences in the rate of use of ORS solution before reaching
hospital by survivors and those who died. This was probably because those who had used ORS
solution had only consumed, on average, less than one litre, a completely inadequate
amount for patients with cholera. Seeking medical help A third possible explanation was posed: Did people's action in seeking medical help
contribute to low mortality? Surveys in Lima and Piura carried out in September 1991 asked
what people would do if they or a member of their family had cholera. In both places over
80 per cent said they would go straight to a health facility, while less than 1 per cent
would take ORS solution exclusively. Few (1.2 per cent) said they would go to a community
oral rehydration unit, probably because it is easy for most people in cities to reach a
hospital - 96 per cent of urban dwellers in Peru are within an hour's travel of a
hospital. So. what have we learnt from the experience of Peru? We believe that in cities and
towns, people should be encouraged to go quickly to hospitals, since immediate seeking of
appropriate treatment seems to have saved many lives in Peru. Case management at hospitals
should be improved and standardised, through better training. In rural areas, however, a strategy based on treatment with ORS solution by a trained
health worker in a community oral rehydration unit is likely to be most effective.
especially in those regions where a hospital is not within reach. Enrique Jacoby and Bruno Benavides, Instituto de Investigación Nutritional,
Apartado Postal 18-0191, Lima, Peru. Study supported by UNICEF.
|
|
DDOnline Controlling
Cholera supplement to DD52  5 Page 6 5 Page 6
How to prevent the spread of disease
Communities can take the following steps to reduce the transmission of cholera The stools of people infected with Vibrio
cholerae 01 contain the cholera organism even if they themselves are not sick.
If cholera germs from these stools contaminate food or water, they can be swallowed by
other people, which spreads the disease. This process is called faecal-oral transmission. Health workers and families can do much to reduce the spread of infection. The most
important actions are: Safe food
- Wash your hands before preparing food and especially after using the toilet
- Cook food thoroughly
- Eat cooked food immediately. However, if cooked food is stored, boil or heat it
thoroughly before eating it.
- Fruits and vegetables should be cooked and peeled. Raw, unpeeled fruit should not be
eaten.
Safe drinking water Wherever possible obtain drinking water from a safe, uncontaminated source (e. g. a
sealed well, a borehole, rainwater, a well maintained piped water supply). If you are not
sure that the water is safe:
- disinfect it with alum potash or chlorine (see="su45.htm#page2">DD45, page
2 of supplement for instructions)
- bring water to the boil, then boil it vigorously for one minute.
Store water in a clean, covered container. Use a ladle with a long handle for taking it
out, so that hands do not come into contact with the water. Hygiene and waste disposal
- If possible, wash kitchen dishes with soap, rinse with clean water and use a clean cloth
to wipe dishes dry (or leave dishes to dry in sunlight in a clean place).
- Dispose of all stools and faecally-contaminated materials in a latrine or bury them if
latrines are not available.
Public health measures If an epidemic occurs, local authorities should take the following actions:
- provide / maintain safe and adequate community facilities for excreta disposal
- ensure an adequate supply of safe drinking water
- prevent the use of contaminated drinking sources
- provide information about how people can purify water at home
- ensure immediate and hygienic disposal of dead bodies
- discourage large gatherings such as feasts or funerals
- establish emergency treatment centres with sufficient amounts of essential supplies,
such as oral rehydration salts and intravenous rehydration solution
- train medical personnel, if necessary, so they can identify patients early and treat
them correctly
- treat cholera patients in a separate area and disinfect contaminated materials (e. g.
bedding, drinking vessels).
|
COMMON SOURCES OF INFECTION
- water contaminated at its source (e. g. by faeces leaking into an incompletely sealed
well) or during storage (e. g. by contact with faecally-contaminated hands)
- contaminated foods that are eaten raw or undercooked, or stored at a temperature at
which bacteria can rapidly multiply
- raw vegetables that have been washed with contaminated water
|
RESOURCES World Health Organization
WHO has recently revised its cholera information pack which contains the following
documents, available free:
- Management of the patient with cholera - treatment guidelines.
- Guidelines for cholera control - for managers of national programmes and others
responsible for cholera control.
- WHO guidance on formulation of national policy on the control of
cholera - for senior health officials and development agencies.
Requests to CDD. WHO, CH-1211 Geneva 27, Switzerland.
The Child-to-Child Trust
Child-to-Child produces resources for teachers and health and community workers. for use
in teaching children how to improve the health of other children.
- Activity sheets are available on prevention and treatment of disease, personal
and community hygiene, child development, nutrition, safety, disability and helping
children in difficulty. The sheet on cholera is available free to people in developing
countries. The full set of activity sheets is £2.
- Children's readers Attractive storybooks are available on ORT -A Simple Cure (£1.20),
and the need for clean water -Dirty Water (£ 1.05 ).
Requests to Child-to-Child. Institute of Education, 20 Bedford Way,: London WC1H 0AL
UK.
PRITECH
- Technical Literature Update, special cholera issue - A summary of the latest
information on cholera, including control, treatment, news on the epidemic and prevention.
Available free.
- Development of a cholera checklist for cholera control - Aimed at ministries of
health, cholera committees and international consultants to assess national preparedness
for preventing and controlling cholera outbreaks.
Requests to PRITECH Information Centre, 1925 North Lynn Street, Suite 400,
Arlington, VA 22209-1707, USA.
|
Produced by Dialogue on Diarrhoea with funding from the
States of Jersey
Controlling Cholera
Health Update - A supplement to Issue no. 52 March - May 1993
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 4 March, 2016
updated: 4 March, 2016
|
version of this Issue