|
| |
Dehydration Treatment Plans
Download Charts
|
*Treatment plans taken from the CDD/WHO Supervisory Skills course, from the module on the treatment of diarrhoea.
What to do if dehydration occurs
Using ORT to Prevent and Treat Dehydration
Preventing Dehydration Mothers must learn:
- to respond to diarrhoea immediately by giving extra suitable drinks (see paragraph on home solutions below).
- to recognize the signs of dehydration which need ORS or special care.
If ORT is given at home early on, dehydration can often be prevented and many children will not become so ill that they need to see a health worker.
Home drinks to prevent dehydration
- Mothers can use household liquids, preferably those that have been boiled, such as rice water or carrot soup. Ideally these drinks should contain starches and/or sugars as a source of glucose and energy, some sodium and preferably some potassium.
- A simple salt/sugar solution, if these ingredients are available, is also suitable for early oral rehydration therapy. 1 level teaspoon (5 ml) of salt should be mixed with 8 level teaspoons of sugar in a litre of drinking water. Molasses and other forms of raw sugar can be used instead of white sugar, and these contain more potassium than white sugar. Do not use too much salt. If the solution has too much salt the child may refuse to drink it . Also, too much salt can, in extreme cases, cause convulsions. Too little salt does no harm but is less effective in preventing dehydration. (A rough guide to the amount of salt is that the solution should taste no saltier than tears.)
Measuring home solutions
Different countries and different communities use various methods for measuring the salt and sugar. Finger pinch and hand measuring, and the use of local teaspoons can be taught successfully. A plastic measuring spoon is available from Teaching Aids at Low Cost (TALC) with proportions to make up 200 ml of sugar/salt solution. Whatever method is used, people need to be carefully instructed in how to mix and use the solutions.
What to do if Dehydration Occurs
If, despite extra home drinks, dehydration occurs, or the diarrhoea continues for more than two days, the child should be taken to see worker to be given ORS solution.
How to assess the degree of dehydration
The table below describes what the health worker should ask and look for, and indicates which treatment plan to follow.
|
1. Ask About |
liquid stools per day |
longer than
3 weeks duration |
| Diarrhoea |
Less than 4 |
4 to 10 |
More than 10 |
Chronic diarrhoea |
| Vomiting |
None or a small amount |
Some |
Very frequent |
Blood or Mucus in the stool |
| Thirst |
Normal |
Greater than normal |
Unable to drink |
|
| Urine |
Normal |
A small amount, dark |
No urine for 6 hours |
|
|
2. Look At |
liquid stools per day |
Longer than
3 weeks duration |
| Less than 4 |
4 to 10 |
More than 10 |
| Condition |
Well, Alert |
Unwell, sleepy or irritable |
Very sleepy, unconscious, floppy or having fits |
Severe undernutrition |
| Tears |
Present |
Absent |
Absent |
|
| Eyes |
Normal |
Sunken |
Very dry and sunken |
|
| Mouth & Tongue |
Wet |
Dry |
Very dry |
|
| Breathing |
Normal |
Faster than normal |
Very fast and deep |
|
|
3. Feel |
liquid stools per day |
Longer than
3 weeks duration |
| Less than 4 |
4 to 10 |
More than 10 |
| Skin |
A pinch goes back quickly |
A pinch goes back slowly |
A pinch goes back very slowly |
|
| Pulse |
Normal |
Faster than normal |
Very fast, weak, or you cannot feel it |
|
| Fontanelle (in infants) |
Normal |
Sunken |
Very sunken |
|
|
|
liquid stools per day |
Longer than
3 weeks duration |
| Less than 4 |
4 to 10 |
More than 10 |
4. Take Temperature |
|
|
|
High fever - 38.5ºC (or 101ºF) or greater |
5. Weigh, if possible |
No weight loss during diarrhoea |
Loss of 25-100 grams for each kilogram of weight |
Loss of more than 100 grams for each kilogram of weight |
|
6. Decide |
The patient has no signs of dehydration |
If the patient has two or more of these signs, he has some dehydration |
If the patient has two or more of these danger signs, he has severe dehydration |
If the patient has chronic diarrhoea, severe undernutrition, or high fever treat or refer to the nearest health clinic for treatment. If there is blood or mucus in the stool and high fever, suspect dysentery and treat with antimicrobials. |
Use
Plan A |
Use
Plan B |
Use
Plan C |
Plan A: for No Dehydration * |
The health worker should discuss home drinks with the mother feeding during diarrhoea and proper home hygiene. The mother should be given enough ORS packets for two days if:
- her child has been on Plan B.
- it is national policy to give ORS solution to all children who visit a health centre for diarrhoea treatment.
- the mother cannot come back if the diarrhoea gets worse.
Mothers given ORS packets to use at home must be carefully shown how to use them. The amount of ORS solution she should give is:
After Each Loose Stool:
- 50-100 ml (¼ - ½ cup) of ORS solution for a child less than 2 years old.
- 100-200 ml for older children. Adults can take as much as they want.
NOTE: Children receiving ORS solution must also be given the usual amount of ordinary drinks they take each day. They should not also be given salt and sugar solution. |
Plan B: for Some Dehydration * |
1. Use this table to see how much ORS solution is suitable for 4-6 hours treatment:
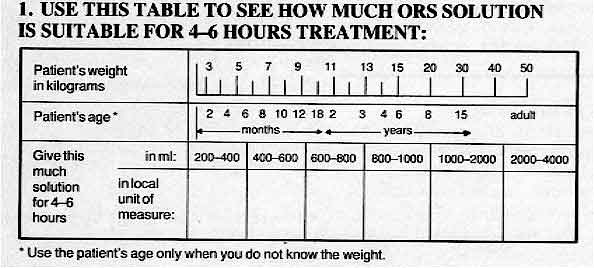
|
|
If the patient wants more ORS solution, five more. If the eyelids become puffy, stop and give other fluids. Use ORS solution again when the puffiness is gone. If the child vomits, wait 10 minutes and then continue slowly giving small amounts of ORS solution.
2. If the mother can remain at the health centre
- tell her how much ORS solution to give her child
- show her how to give it
- watch her give it
3. After 4-6 hours reassess the child. Then choose the suitable treatment plan.
NOTE: For children under 12 months continuing treatment plan B after 4-6 hours, tell the mother to give:
- breastmilk feeds between drinks of the ORS solution,
or
- 100-200 mls of clean water before continuing ORS if she does not breastfeed her child.
4. If the mother must leave any time before completing treatment plan B, tell here:
- to finish the 4-6 hours treatment as in 1. above
- to give the child as much ORS solution as he wants after the treatment
- to look for the signs of dehydration and, if the child has any, to return the next morning.
Give her enough ORS packets for 2 days and show her how to prepare ORS solution.
Explain briefly how to prevent diarrhoea. |
|
Frequently asked questions:
What is dehydration?
Dehydration is the loss of water and body salts through diarrhoea. Early features are difficult to detect but include dryness of mouth and thirst. The signs of dehydration include: sunken fontanelle (in infants); fast, weak pulse; breathing faster than normal; loss of skin elasticity; sunken, dry eyes and reduced amount of urine. Rehydration is the correction of dehydration.
What is ORT?
ORT is the giving of fluid by mouth to prevent and/or correct the dehydration that is a result of diarrhoea. As soon as diarrhoea begins, treatment using home remedies to prevent dehydration must be started. If adults or children have not been given extra drinks, or if in spite of this dehydration does occur, they must be treated with a special drink made with oral rehydration salts (ORS). The formula for ORS recommended by WHO and UNICEF contains:
- 2.6 gms sodium chloride
- 13.5 gms glucose (anhydrous)
- 1.5 gms potassium chloride
- 2.9 gms trisodium citrate, dihydrate
The above ingredients are dissolved in one litre of clean water. This new formula gives the packets a longer shelf life and is at least as effective in correcting acidosis and reducing stool volume. Packets containing sodium bicarbonate are still safe and effective.
How does ORT work?
Acute diarrhoea normally only lasts a few days. ORT does not stop the diarrhoea, but it replaces the lost fluids and essential salts thus preventing or treating dehydration and reducing the danger. The glucose contained in ORS solution enables the intestine to absorb the fluid and the salts more efficiently. ORT alone is an effective treatment for 90-95 per cent of patients suffering from acute watery diarrhoea, regardless of cause. This makes intravenous drip therapy unnecessary in all but the most severe cases.
Can ORS he used for everyone?
ORT is safe and can be used to treat anyone suffering from diarrhoea, without having to make a detailed diagnosis before the solution is given. Adults need rehydration treatment as much as children, although children must always be treated immediately because they become dehydrated more quickly.
What should be done if the child vomits?
Vomiting does not usually prevent the therapy from being successful. Mothers must be taught to persist in giving ORS solution, even though this requires time and patience. They should give regular, small sips of fluid. Giving ORT reduces nausea and vomiting and restores the appetite through correction of acidosis and potassium losses.
Should feeding continue at the same time as ORT?
Feeding, especially breastfeeding, should be continued once dehydration has been corrected. Even if the diarrhoea continues or the child is vomiting, some of the nutrients are being absorbed. Suitable food should not be withheld, as the child may become malnourished. Once the diarrhoea episode has passed, the child should be given more food than usual to make up for losses during diarrhoea. Breastfeeding is particularly beneficial because breastmilk is easily digestible. It also contains protective substances which help to overcome the infection causing the diarrhoea.
What sort of foods are good during diarrhoea?
- High energy foods such as fats, yoghurt and cereals are quite well absorbed during diarrhoea. Small, frequent feeds of energy-rich local foods familiar to the child should be given. A little vegetable oil can be added to foods such as millet or rice to increase the energy content.
- Foods high in potassium are important to restore the body's essential stores depleted during diarrhoea. Such foods include lentils, bananas, mangoes, pineapples, pawpaw, coconut milk and citrus fruits.
- Certain foods should be avoided during diarrhoea, for example those containing a lot of fibre such as coarse fruits and vegetables, wholegrain cereals and spicy foods.
Is it necessary to use drugs as well as ORT?
Drugs should not be used except in the most severe cases. Even then they should be administered with care, preferably after the organism causing the diarrhoea has been identified. Small children with dysentery and fever require an antibiotic. Refer such patients to a health service for advice. ORT on its own is usually enough to rehydrate the child. Unnecessary antibiotic therapy upsets the normal bacteriological balance of the intestine. Many anti-diarrhoeal preparations have proved to be either ineffective or too powerful for very small infants.
Can the solution be made with dirty water?
The benefits of fluid replacement in diarrhoea far outweigh the risks of using contaminated water to make up oral rehydration solution. In situations where it is difficult to boil water, mothers are advised to use the cleanest water possible.
Can ORS solution be stored?
Generally a made-up solution should be covered and not kept for more than 24 hours, due to the risk of bacteriological contamination. Packets of ORS should be stored carefully and not kept in temperatures of over 30°C or in conditions of high humidity. Where the ingredients to make up ORS are being stored in bulk the glucose/sucrose should be kept apart from the rest of the dry ingredients. The new citrate formula ORS has a longer shelf life.
|
updated: 22 April, 2018
|