|
| |
Issue no. 52 - March-May 1993
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
updated: 4 March, 2016
Pages 1-8 Dialogue on Diarrhoea Online Issue 52 - March-May
1993
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 52 March-May
1993  Page 1 2
Page 1 2
ORT: a life-saving solution
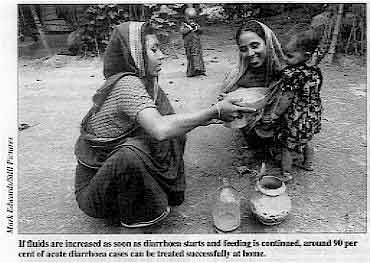 |
If fluids are increased as soon as diarrhoea starts and feeding
is continued, around 90 per cent of acute diarrhoea cases can he treated successfully at
home. About twenty-five years ago, scientists
discovered that a simple solution of water, salts and glucose had the potential to save
the lives of millions of children in developing countries.
|
That discovery - oral rehydration therapy (ORT) to treat dehydration caused by
diarrhoea - was described in the journal, The Lancet, as potentially the most
important medical advance this century. Unlike many medical 'solutions' to health problems, ORT has the advantage of being
low-cost and simple. It can be used by health workers and families everywhere to prevent
children dying of dehydration. Since ORT was developed, it has been actively promoted in every corner of the globe,
and has been a key strategy in the worldwide movement to reduce deaths from diarrhoea. Gains from using ORT have been impressive. Millions of lives have been saved, including
during the current cholera pandemic. Two-thirds of the world's population is estimated to
have access to packets of oral rehydration salts (ORS). This issue of DD goes back to basics. It describes what ORT is, how it works,
and how it should be given. Much has been learnt about the best methods of ORT. One key to successful treatment of
diarrhoea is early action in the home. The emphasis now is on educating mothers to
increase children's fluid intake as soon as diarrhoea starts and to continue feeding.
These two measures can ensure that 90 per cent of acute diarrhoea cases are treated
successfully at home, without requiring the assistance of a health worker. Fast action is also required to deal with cholera. This issue contains a centrespread
supplement which sets out guidelines for recognising and treating cholera. Prevention is
also important. The same measures that will help to prevent the spread of cholera - the
provision of safe water, better sanitation facilities, and improvements in hygiene
behaviour - will also prevent most other forms of diarrhoea. Many challenges remain. Despite high awareness about ORT, a low proportion of mothers
(around 30 per cent) actually increase children's fluid intake during diarrhoea. Many
families continue to buy drugs, wrongly believing medicines will stop the flow of
diarrhoea. In 1990 the World Summit for Children called for the halving of diarrhoeal deaths by
the year 2,000. Last year, 88 countries took a bold step towards that goal by pledging to
reach a target of using ORT in 80 per cent of cases of diarrhoea by 1995. We all have a role to play in achieving these goals. We can do this by passing on
messages to mothers about fluid and food intake, by taking time to convince parents that
they do not need to buy useless drugs, or by working with communities to improve their
water supplies and sanitation.
|
In this issue:
- Choosing an appropriate oral rehydration solution
- How to give ORT at home
- Controlling cholera - 6 page supplement
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 52 March-May
1993  1 Page 2 3 1 Page 2 3
Back to basics: What is ORT?
 |
A dehydrated child being given oral rehydration therapy by his mother. Most deaths from diarrhoea are caused by
dehydration (the loss of water and salts from the body). Oral rehydration therapy (ORT)
saves lives by replacing what has been lost during diarrhoea. If given early enough, ORT
can prevent dehydration. At a later stage it can reverse dehydration.
|
ORT means giving fluid by mouth to prevent or correct dehydration. The fluid can take
many forms, ranging from drinks available in most homes to a solution made by adding water
to oral rehydration salts (ORS) sold in packets. The key principle of oral rehydration therapy is that children with diarrhoea need to
drink more fluid than usual. The following is a summary of the different types of fluids that can be used for ORT. DDis not making recommendations about which fluid to use. Different fluids are
appropriate according to local circumstances. Ministries of health in most countries have
their own guidelines. Health workers should find out what is recommended for their
countiy.
Home fluids Drinking extra fluids in the early stages of diarrhoea is crucial to preventing dehydration.
The combination of giving more fluid than usual as soon as diarrhoea starts and continuing
feeding is an effective home therapy for acute diarrhoea. It is estimated that if home
therapy is given early and correctly, fewer than 10 per cent of acute diarrhoea cases
would require care by a health worker. Readily available home fluids (as recommended by national ministries of health) should
be given as soon as diarrhoea starts. Liquids containing salt and either a starch, sugar, or protein are ideal because
they provide the necessary ingredients for absorption of both fluid and salt. Good
examples are: soups that are normally prepared with salt, salted rice water, or salted
yoghurt drinks. In addition, children should be given plenty of other fluids which do not contain salt,
such as plain drinking water, green coconut water, weak unsweetened tea and unsweetened,
fresh fruit juice. It is important that the recommended fluids are commonly found in most homes and that
mothers consider them acceptable to give to children with diarrhoea. Drinks containing sugar, such as fizzy drinks, or stimulants, such as coffee, should be
avoided. If the child is breastfed, it is important to continue breastfeeding. ORS solution Oral rehydration salts (ORS) solution is recommended by WHO for treating dehydration.
It can also be used, where practical, as a home therapy for preventing dehydration. ORS
packets contain a combination of glucose and salts which, when dissolved in water, makes
an effective rehydration solution. Most ORS packets require a litre of water to be added. ORS packets approved by the World Health Organization (WHO) and UNICEF contain:
- 3.5g sodium chloride
- 1.5g potassium chloride
- 2.9g trisodium citrate, and
- 20g anhydrous glucose.
Packets which use bicarbonate of soda (2.5g) instead of trisodium citrate are
acceptable but cannot be kept in storage very long. WHO estimates that more than two-thirds of the world's population can now obtain ORS
packets close to home. More than 60 countries produce ORS packets based on the WHO/UNICEF
formula. Some commercial oral rehydration packages are different from ORS. Some contain too much
sugar. Others contain too little salt. Health workers should use packets which have been
approved by their ministry of health.
GLOSSARY ORT Oral rehydration therapy:
the administration of fluid by mouth to prevent or correct dehydration caused by diarrhoea ORS Oral rehydration salts: the WHO/UNICEF recommended
formula. When the salts are dissolved in water the product is oral rehydration salts (ORS)
solution. SSS Sugar-salt solution: an oral rehydration solution
prepared from household salt and sugar (sucrose) dissolved in water.
|
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 52 March-May
1993  2 Page 3 4 2 Page 3 4
Sugar-salt solution Sugar-salt solution (SSS) is a home-made version of ORS containing salt (sodium
chloride), sugar (sucrose) and water. The following combination is recommended - 3g (half
a level standard 5ml teaspoon) of salt; 18g (four level teaspoons) of sugar; dissolved in
one litre of water. SSS is recommended for use in some countries as a first line of action in the home to
prevent dehydration. In a few places where ORS is not readily available, SSS is also used
to treat dehydration. However, teaching mothers to make up the correct recipe for SSS has proved to be
difficult in many countries. That is why WHO is now suggesting that mothers be taught to
give suitable home fluids or ORS solution rather than being taught a special recipe. Cereal-based solutions Several studies have suggested that replacing the 20g of glucose in ORS with 50g of
cooked rice powder (or other cereal powder) results in better absorption of the fluid and
less output of diarrhoeal stools. It now appears, however, that this is only true for
adults and children with cholera, but not for children with acute non-cholera diarrhoea. Recent studies in Egypt and Pakistan have shown that when children are fed a diet
including cooked cereal and vegetables as soon as rehydration is completed, stool output
and the duration of diarrhoea are the same with glucose or cereal-based rehydration
solution. The better results seen in earlier studies with cereal-based oral rehydration
solution were probably because the children were not fed adequately during the first 24
hours of treatment. These results support the use of standard oral rehydration solution
for children with acute non-cholera diarrhoea and emphasise the importance of continuing
normal feeding as soon as rehydration is corrected. Cereal-based fluids, such as rice water, are among the fluids useful for home therapy
to prevent dehydration during diarrhoea. They are most effective if they also contain some
salt. Where cereal porridges are used as a weaning food, these should be prepared as usual
and given as food. Dilution of porridge is discouraged because it will reduce the child's
intake of calories.
|
Weighing up the choices of solutions for home therapy Home fluids
ADVANTAGES
- Fluids are readily available in the home, therefore
- there is little extra cost involved
- children are likely to be familiar with the taste and less likely to reject them
- No special recipe is needed
- Mothers are encouraged to give fluids that are culturally acceptable for children with
diarrhoea
DISADVANTAGES
- Home fluids may not seem 'special' so may not satisfy mothers' desire for medicine for
their children
- The amount of salt in home fluids is variable, and may be less than is required for
optimal rehydration
ORS solution
ADVANTAGES
- A pre-packaged formula to which mothers need only add water
- Includes ingredients to correct potassium loss and acidosis
- Has been widely tested in a range of settings
- Packets are commonly available in many countries
- Is sometimes seen as 'medicine', therefore increasing its acceptability
DISADVANTAGES
- Is dependent on availability of packets, therefore
- it costs more than home-made solutions
- if packets are unavailable nearby, treatment may be delayed
- It increases mothers' reliance on outside resources
- Requires a standard container, usually 1 litre, and mothers need to be taught how to
make up the solution
- Incorrectly mixed ORS solution can be dangerous e. g. can cause high levels of sodium in
the blood (hypematraemia)
- Is sometimes seen as 'medicine', so mothers may give it in small sips like medicine or
reject it if diarrhoea does not stop
SSS
ADVANTAGES
- Ingredients are available in most countries
- Increases mothers' ability to manage their children's diarrhoea at home
DISADVANTAGES
- Incorrectly measured SSS can be dangerous e. g. can cause hypematraemia, especially if
the proportions of salt and sugar are confused
- Different sized containers and measuring implements increase the risk of incorrect
measurement
- It is not easy to teach mothers to remember the recipe and make it up correctly
- Sugar is not always available or can be too expensive
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 52 March-May
1993  3 Page 4 5 3 Page 4 5
|
Understanding dehydration To stay healthy, the body requires a correct balance of water and various salts in its
cells, and in fluids such as the blood. During diarrhoea, water, salts (electrolytes) and
alkali are lost in the stools. At first these losses come almost entirely from the blood
and the fluid that surrounds the cells of the body. As the amount of fluid lost increases,
the volume of blood decreases. Later, fluid is also lost from the cells. This loss of water and salts reduces the production of urine and tears, and the heart
beats faster to compensate for the reduced blood volume. The mouth and tongue become dry,
and the skin loses its elasticity (a skin pinch retracts slowly). Eventually the heart cannot beat fast enough to maintain the normal blood flow through
the body. The pulse become weak or cannot be felt, the blood pressure falls and the
patient becomes lethargic or unconscious. This is circulatory collapse (shock). If
treatment is not given quickly the patient will die. Treatment When diarrhoea is severe, and especially when there are signs of shock, the blood
volume must be restored very quickly, and lost electrolytes and alkali replaced fast. This
should be done with an intravenous fluid, such as Ringer's lactate solution. However, in most patients with diarrhoea, dehydration is not severe and the lost fluid
and electrolytes can be replaced by drinking. The most effective way is to give ORS
solution. It contains water and electrolytes in the correct proportion to replace what is
being lost. ORS solution also contains glucose, which is essential to help the absorption
of water and salt. This is the basis of oral rehydration therapy. Prevention Home therapy to prevent dehydration is based on the same principles. It involves giving
increased fluids and food. This provides water and starch (which breaks down to glucose
when digested). It is also important to provide some salt in either the food or fluid. Dr William Cutting
|
|
The experience of India Shanti Ghosh discusses the successes and challenges of
promoting ORT in India. The 1980s witnessed a remarkable decline
in infant mortality in India - from personnel - particularly doctors - and for improved
health education. 114 per 1,000 in 1980, to 80 in 1990. However, diarrhoeal diseases
continue to be a major health problem, accounting for almost a third of childhood deaths,
or one million deaths per year. The national programme for control of diarrhoeal diseases (also known as the national
ORT programme) aims to reduce diarrhoeal deaths by 30 per cent in the five years leading
up to 1995. The programme's policy on ORT is that the first line of management is fluids available
in the home, such as rice water, lentil water, tea, buttermilk and shakanjivi (a common
drink of lemon, sugar and a pinch of salt dissolved in water). If diarrhoea persists or
there is any sign of dehydration, then ORS solution is advised. If ORS packets are not
available, then it is recommended that sugar-salt solution (SSS) be given. A survey was undertaken by the government in 1989 to evaluate mothers' attitudes to
diarrhoea management in six states - Uttar Pradesh, Rajasthan, Orissa, Haryana,
Maharashtra and Tamil Nadu. It showed that the practice of increasing the amount of fluid given during diarrhoea
was discouragingly low. Fluids most commonly given were: water (38 per cent), milk (21 per
cent), and tea or coffee (12 per cent). ORS solution and sugar-salt solution (SSS) ranked
sixth and seventh among the ten fluids mentioned most frequently by mothers. Most mothers continued to breastfeed and a considerable number continued semi-solid
feeding. About a third of mothers were able to name three or more symptoms of dehydration. In about 65 per cent of diarrhoeal episodes a medical consultation took place. However,
the vast majority of mothers consulted private village 'doctors' who were neither fully
trained nor licensed. Less than 10 per cent consulted government health facilities. Free
medicine was considered to be of low quality. The village practitioners prescribed a variety of medicines in nearly every case. Only
11 per cent advised ORS as the first response to diarrhoea while even fewer - 3 per cent -
advised SSS. The survey showed a clear need for better training of health personnel -
particularly doctors - and for improved health education. While reduction of deaths due to oral rehydration is a landmark in recent medical
research, the aim should be to prevent and control this scourge altogether. For that to
happen, education, access to safe drinking water, better housing and sanitation, and
personal hygiene (especially handwashing) are essential. In other words, what is needed is
a comprehensive development strategy rather than only health inputs. Mothers' desire to stop the diarrhoea is a major barrier to the acceptance of ORT.
Although glucose and sugar-based solutions prevent dehydration, they do not reduce the
volume, frequency or the duration of diarrhoea. Mothers then resort to drugs in the
mistaken belief that these will reduce the number of stools. Although the production of ORS packets has increased substantially, it is still
inadequate. Because of distribution difficulties, ORS packets are not universally
available. According to the survey, ORS packets were used in only 19 per cent of diarrhoea
episodes. A variety of packets is commercially available, but many are expensive and the
different formulas are confusing. Instructions are written in very fine print which is
difficult to read. A large number of people cannot read anyway. Efforts are now being made
to persuade the Controller General of Drugs to standardise the formulation of ORS in
packets. Another problem both with ORS packets and SSS is the measurement of 1 litre of water.
The size of utensils varies in different parts of India, and it is not always possible to
explain how much 1 litre is. I used to advise mothers to measure 1 1/2 squash or sherbet
bottles. (We cannot talk in terms of beer bottles!) The mothers are advised to throw away
the left-over solution after 8-12 hours, but they are loathe to 'waste' this solution.
They tend to make a smaller amount and, in the case of ORS, to dissolve a portion of the
packet in a small quantity of water, usually a cup or a glass. In my opinion, the answer
is to make smaller ORS packets which can be dissolved in a glass (approximately 200ml) of
water. However, this would increase the cost considerably. While reduction of deaths due to oral rehydration is a landmark in recent medical
research, the aim should be to prevent and control this scourge altogether. For that to
happen, education, access to safe drinking water, better housing and sanitation, and
personal hygiene (especially handwashing) are essential. In other words, what is needed is
a comprehensive development strategy rather than only health inputs. Dr Shanti Ghosh, 5 Sri Aurobindo Marg, New Delhi 110016, India.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 52 March-May
1993  4 Page 5 6 4 Page 5 6
The pioneering years
Many scientists dream of being involved in a discovery that saves millions of
lives, but few achieve it. Dr Dilip Mahalanabis has had that satisfaction.
He contributed to early studies on ORT and then led the first large scale field trial. DDtalked to Dr Mahalanabis about the development of ORT. What have been some of the major milestones in the development of ORT? First, there was the development of an effective formula. Then there was the testing of
the scope and limits of ORT. At the beginning of this century a Scottish physiologist, Weymouth Reid, demonstrated
the role of glucose in increasing absorption of sodium from the small intestine. However,
the first practical demonstrations of a glucose-salt solution's ability to restore a
positive fluid balance when taken orally were not until the 1960s. Dr Norbert Hirschhorn
at the Cholera Research Laboratory in Dhaka, and Dr Nathaniel Pierce at the Johns Hopkins
International Center for Medical Research and Training in Calcutta, showed the
effectiveness of ORT in rehydrating cholera patients. Later studies proved that it could
rehydrate children and infants with non-cholera diarrhoea. By 1971 we knew that ORT worked in a hospital setting. However, its practical
importance in saving lives had not been established. The first proof of its power in the
field came during the Bangladesh liberation war in 1971. In one of the largest exoduses in
history, about 10 million people walked across the border into India. Cholera broke out in
the refugee camps. We gave up research and went into the camps to provide treatment. In no
time we ran out of intravenous solution. We started a mini factory for producing oral
rehydration solution. The majority of the treatment was oral because there was no
alternative. The situation gave us a sort of natural experiment. Patients were brought in
by rickshaw. Relatives filled up bottles with oral rehydration solution and gave the fluid
to patients. As a result, the mortality was reduced to just 3 per cent. from a previous
level of 15-30 per cent. The success of ORT in such severe conditions convinced health planners of its
usefulness and prompted WHO to start promoting ORT as a key element in the management of
diarrhoea. While ORT was being developed and tested, feeding during diarrhoea was also being
promoted. The two go hand-in-hand; neither is less important. A child may survive acute
diarrhoea. but then die from the consequences of malnutrition. Not giving any food for 48
hours used to be the standard recommendation. We now know better; continued feeding
results in faster recovery and better nourished children. Were there any problems which had to be overcome in promoting ORT? There was great resistance initially to the implementation of ORT, particularly among
paediatricians and academics in the UK and the USA. This was significant because a large
number of developing country paediatricians are trained in the UK or USA. When they go
home they tell their colleagues what they've learnt. Most of the scientists working on ORT development were cholera researchers. I was the
only paediatrician involved directly. My role was to give technical back-up in defending
ORT to paediatricians. It took some time for the medical community to come on board, but
pressure was building up as more and more studies showed ORT was highly effective in
infants and children. There are still pockets of academia who are sceptical about it, but
we've made peace with most objectors, and if they don't agree, at least they won't
obstruct efforts to promote ORT. Have there been significant improvements on the original formula for ORT? The problem with ORS solution is that it does not reduce the amount or
duration of diarrhoea. Everyone runs for some kind of medicine to stop diarrhoea. But most
of the medicines are useless and some are dangerous. One of the major initiatives in the
1980s was to try to make ORS more absorption efficient. Two approaches were studied: replacing glucose with a cereal such as cooked rice
powder, and adding amino acids to ORS. Adding amino acids was not helpful, but the rice
powder yielded surprisingly positive results in cholera patients. It substantially reduced
the stool output and significantly decreased the duration of diarrhoea. Unfortunately, the
benefit of rice-based oral rehydration solution for children with acute non-cholera
diarrhoea was much smaller*. Rice-based oral rehydration solution is now recommended for use in patients with
cholera, provided it is operationally feasible. We find it very convenient to use it at
the International Centre for Diarrhoeal Disease Research in Bangladesh. However it is not
so easy to prepare in smaller treatment centres without cooking facilities. WHO is not
promoting a rice-based solution as a major option to glucose packets because it has no
advantage in the treatment of children with non-cholera diarrhoea and it would be
relatively expensive to produce in packets. However, I have a feeling that industry might
be able to solve the production and logistics of a cereal ORS in a packet more easily than
it now appears. Do you think that the misuse of drugs for diarrhoea can be curbed? It's not an easy matter to solve. It's deeply connected with pressure from the drug
industry. However I don't see why there can't be pressure groups to campaign against the
misuse of drugs. If we could succeed in the campaign against smoking, there's no reason we
can't succeed in cutting down the misuse of drugs. What are the future challenges? We are still looking for the magic bullet which will really stop the diarrhoea. We have
already reduced diarrhoea severity in cholera patients by as much as 35-40 per cent with
rice-based oral rehydration solution. If we could achieve the same reduction in infants
and small children with non-cholera diarrhoea it would be a major step forward. I don't
think we have exhausted the possibilities yet.
Dr Mahalanabis is an associate director of the International Centre for Diarrhoeal
Disease Research, Bangladesh. * Editors' note: Recent studies have shown that rice-based
oral rehydration solution has no advantage over a glucose-based solution when children are
fed as soon as dehydration is corrected. See="#page3">page 3
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 52 March-May
1993  5 Page 6 7 5 Page 6 7
Health workers' opinions
ORT has been promoted for twenty years. But how successful is it in the field? DD
asked three health workers to comment. Sister Cathrin Gyinokang is a public health nurse in northern Ghana. In Ghana, ORS was first introduced by UNICEF. Now Ghana produces its own ORS sachets
commercially. However, they are quite expensive and many mothers in my area cannot afford
to buy them. So we now teach mothers how to prepare sugar-salt solution at home. We even
use singing as a teaching method. The materials used in preparing it are local. Instead of
measuring water in bottles we use calabashes with the litre level marked on them. I know from my own experience that many children in our area recover from diarrhoea at
home these days after getting sugar-salt solution as first aid in the home. There are some problems though. For example, even though sugar is widely available,
some mothers cannot afford to buy it for SSS. It would be good if free sachets of ORS
could be made available again, so that health workers could give them to mothers who
cannot afford to buy sugar to make SSS. Also, some mothers do not use the right quantity of water when preparing sugar-salt
solution. Another big problem is that many mothers think sugar-salt solution is a cure for
diarrhoea, not a treatment for replacing lost water and salts. They tend to stop giving it
if the diarrhoea does not improve quickly. If they use ORS sachets, they sometimes use
just a small pinch in a little bit of water, thinking it is like a medicine. I would like to suggest to other health workers that we need to teach mothers why they
should give ORT, and stress that in addition to ORT, children with diarrhoea need to
continue their normal food intake. Mothers also need to know when a child should be taken
to a clinic. We should also stress the use of clean water, not boiled water, in making oral
rehydration fluids. Many mothers cannot afford enough firewood, and if they spend a lot of
time searching for wood, and then boiling water, the damage of dehydration may already
have been done. Mbalu Kallon is a nurse-midwife in charge of a clinic in Sierra Leone. In the past we used to rely on ORS sachets. But we realised that we would eventually
have to stop giving them out free, and that when mothers were back in their villages
without access to sachets, they wouldn't know how to help their children with diarrhoea.
Therefore, we decided it was important to teach mothers how to prepare oral rehydration
fluids themselves. We have involved our traditional birth attendants in spreading messages
about ORT. We advise mothers to use local drinks such as rice water, and coconut water, and we
also teach home preparation of SSS. The SSS recipe is printed on the back of our mother
and child health cards. It is not just written, there are also pictures of how to measure
the ingredients. We are planning to provide mothers with spoons for measuring the right
quantity of sugar and salt. We want to use the spoons as incentives to give to mothers who
have brought their children in for a full course of immunisation. My experience is that child mortality from diarrhoea has decreased since ORT has been
promoted - especially during cholera epidemics. One night my neighbour was seriously sick
with frequent stools. Her relatives came and woke me up. I prepared some ORS solution and
got her relatives to give it to her throughout the night. Next morning she still had
frequent diarrhoea so we took her to the clinic where she was put on an intravenous drip.
I am sure that without ORS solution she would have died before morning. However, there are some difficulties in promoting ORT. We have seen that not even all
health workers teach mothers how to prepare the fluids correctly. Some demonstrate wrong
quantities so mothers become confused. Another problem is that people in my area like medicine very much, especially
injections. They think that home-made SSS is too simple. Also, some people cannot afford
to buy sugar. That is why health workers should not just emphasise one type of solution.
There have to be choices based on local circumstances. I would like to encourage health workers to continue to teach mothers and even children
about oral rehydration therapy. Dr Ni has worked in a large hospital in China for several years. In China people use both traditional and Western medicine. We have used traditional
medicine for more than 3,000 years and it is very effective. When a child gets diarrhoea, parents start treatment at home with traditional medicine
such as herbs and rice water. But most people also believe in modem medicine. If the child
does not get better after treatment with traditional medicine, parents go to a barefoot
doctor (the Chinese equivalent of a community health worker) or to hospital. ORS is mostly used in rural areas. Barefoot doctors give ORS solution as first aid. I
think ORS is very good because it has saved a lot of lives. It is also very cheap in China
and barefoot doctors do not have time to teach parents how to make sugar-salt solution.
However, some rural people are very hesitant to use ORS because they are superstitious and
don't trust it. In our hospitals we do not usually use ORS. Instead antibiotics are often given.
Antibiotic abuse is serious. I would like to point out the importance of teaching parents what to do when a child
has diarrhoea, and advising mothers that babies should continue to be breastfed. Parents
need to know the danger signs of dehydration. They also need to learn about the causes of
diarrhoea and to be encouraged to practise good hygiene. Interviews by Anette Laakso, Pentecostal Church Association of Tanzania.
|
MAIN POINTS
- Teaching about how and why to use oral rehydration therapy must continue.
- ORS packets should be made more widely available and cheaper.
- SSS is an alternative to ORS, but careful and thorough teaching about how to
prepare it must be standardised for each country and sustained.
- Common home fluids, such as soup, rice water, yoghurt drinks and plain water,
should be encouraged to prevent dehydration.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 52 March-May
1993  6 Page 7 8 6 Page 7 8
A useful guide to giving ORT at home Dr A N Alam explains when and how mothers should administer ORT. The two most important treatments for
diarrhoea are oral rehydration therapy and continued feeding. ORT should be started as
soon as diarrhoea begins in order to prevent dehydration. Any delay may mean the child's
condition gets worse. A dehydrated child (see="su52.htm#page 3">page 3 of cholera
supplement for signs of dehydration) is usually thirsty and will want to drink the
rehydration fluid. How to give ORT Oral rehydration fluids can be given in either of the following ways:
- teaspoon (or cup)
- plastic dropper (for small infants)
The spoon is the best method for most infants and young children because it allows
fluid to be given at a steady rate in small amounts, which reduces vomiting. A cup may be used for children older than five years and for adults. Very small babies
should be given rehydration fluid with a spoon or a plastic dropper. However, a plastic
dropper is difficult to clean and should only be used when good hygiene is possible. The
mother should insert the dropper between the cheek and teeth and the contents should be
gently squeezed at a rate of 5ml every 3-4 minutes. Babies should not be given fluid too quickly as they might vomit or choke. Feeding
bottles should not be used as they are difficult to clean and the rate of flow of the
fluid cannot be controlled. Be patient and persistent when giving fluid. If a child refuses to drink, it usually
means that enough fluid has been given. How often Rehydration fluid should be given at a steady rate in small amounts. One teaspoonful
every 2-3 minutes is a useful guide (see="#How much">below for amounts
according to age). This allows time for it to be absorbed and reduces the risk of
vomiting. How much The amount of rehydration fluid given should be about the same as the volume of vomit
and stool passed. However, it may not always be possible to accurately measure the volume
lost, so guidelines are as follows:
- A child under two years old should be given about 50-l00ml (¼ - ½ cup) of rehydration
fluid after each loose stool.
- Older children will require l00-200ml (½ -1 cup).
- Children over ten years old and adults can take as much as they want.
If a child is usually breastfed, continue breastfeeding in between giving oral
rehydration fluid. It is important to emphasise giving plenty of rehydration fluid. The mother should be
advised that just giving a few sips of rehydration fluid is not enough; the amounts
described earlier should be given until diarrhoea stops. If the child has many watery stools, vomits repeatedly, is very thirsty, or is eating
or drinking poorly, he or she should be taken to the nearest health centre. The child
should also be taken if there is fever or blood in the stool. Potential problems If the child is vomiting, ORT should not be stopped. Instead, the mother should wait
for five to ten minutes, then continue giving the solution but more slowly, a teaspoonful
every 3-4 minutes. How to teach mothers The best time to teach a mother to give ORT is when she brings her child for treatment
of diarrhoea. It is important to show mothers the correct method of preparing and giving
rehydration fluid. First show the mother how to give ORT, then encourage her to try it
herself, while a health worker is present to give advice. Take time to explain to her the
need to give extra fluids and find out what fluids are available in her home. Then suggest
which fluids would be especially useful for ORT at home. Dr A N AIam, consultant physician, ICDDR, B, GPO 128, Dhaka-1000, Bangladesh.
WHO's guidelines for home care to prevent dehydration As soon as diarrhoea starts: 1. Give more liquids than usual
- Give the child more fluids than usual, including plain water.*
- If possible, also give a fluid that contains salt, e. g. ORS solution, salted soup,
salted rice water.
- Other good drinks include yoghurt drinks, water in which a cereal (such as rice) has
been cooked, unsweetened tea, green coconut water and unsweetened, fresh fruit juice.
2. Continue to feed the child
- If the child is breastfed, continue to breastfeed, as often and for as long as the child
wants.
- Continue the child's normal diet, including milk. Encourage the child to eat.
- Give small meals frequently, at least six times a day.
- If possible, give a food that contains salt.
3. Further care
- Take the child to a health worker if s/he does not get better in three days or develops
any of the following:
- many watery stools
- repeated vomiting
- is very thirsty
- eats or drinks poorly
- fever
- blood in the stool
* Exclusively breastfed infants under six months old should
continue to be breastfed and receive ORS solution. If ORS is not available, give plain
water. Other fluids should not be given.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 52 March-May
1993  7 Page 8 7 Page 8
TREATMENT OF CHOLERA Duration of antibiotic therapy Is antibiotic therapy only advisable for severe cases of cholera? If so, is
giving the recommended dose of antibiotic for three days long enough to completely destroy
Vibrio cholerae? I think 500mg tetracycline four times a day for five days (or reduced to three times a
day on the fourth and fifth day) is more effective. Neye Odimbite, Pharmacist, State Hospital, Ikirun, Osun State,
Nigeria.
Dr Nathaniel Pierce, CDD/WHO, replies: Antibiotic treatment for cholera is only recommended for patients with severe
dehydration. This is because the benefit of antibiotics has only been demonstrated in such
cases. Also, cholera in patients who do not show signs of dehydration, especially young
children, cannot be accurately distinguished from other sorts of diarrhoea for which
antibiotics are useless. Three days of treatment with tetracycline is sufficient, provided the strain of V.
cholerae causing the illness is sensitive to the antibiotic. A single dose of
doxycycline (300mg) is equally effective, but is only advised for people over 12 years
old. Isolates of V. cholerae should be monitored at regular intervals to
test their sensitivity to tetracycline and other antibiotics. If the illness continues for
more than 48 hours after starting antibiotic treatment, antibiotic resistance should be
suspected.
Editors' note: See also page 4 of the cholera supplement.
Misuse of tetracycline We had an outbreak of cholera in Kirinyaga district, 100km north-east of Nairobi. The
water is dirty and village sanitation is poor. We had more than ten deaths. The majority
died of dehydration before reaching hospital. Treatment started in hospital with IV solution and tetracycline. However, it was found
that V. cholerae was resistant to tetracycline, so ampicillin was used instead.
Tetracycline has been misused in Kenya for years. It is readily available in shops, bars
and bus parks, and is sold by bush 'doctors'. I would be interested in hearing from other
readers whether the situation is similar in their countries. Joel Kibet Kirui, Medical Technician, PO Box 14, Marigat, via Nakuru, Kenya.
Dr Pierce replies: Excessive use of any antibiotic leads to bacterial resistance to that antibiotic. The
experience with tetracycline in Kenya emphasises this. Antibiotics should only be used to
treat people with severe cholera, or to treat family members of patients in areas where it
has been shown that the risk of second cases occurring within a family is 20 per cent or
more. Antibiotics should not be used for other forms of preventive treatment. When resistance to tetracycline is encountered, alternative antibiotics are
cotrimoxazole, furazolidone, erythromycin or chloramphenicol. The clinical efficacy of
ampicillin has not been proved. Editors' note: See also page 4 of the cholera
supplement.
Advice welcomed The article about cholera in DD49 challenged the
misconceptions I had about cholera treatment. During the cholera epidemic last year in
Nigeria most hospitals based the treatment of cholera solely on fluid replacement without
any form of antibiotic therapy. However, one of my doctor friends combined both antibiotic
treatment and fluid replacement. His patients had a more rapid recovery than those managed
in the general hospitals. I would appreciate your comments on this issue, Ibiang Usani Obono, Eja Memorial Joint Hospital, Itigidi Abi LGA, Cross River State,
Nigeria.
Dr Pierce replies: An effective antibiotic is not a substitute for correct treatment of dehydration, but
it does shorten the duration of cholera. This in turn reduces the duration of treatment
and the need for supplies such as ORS or IV fluids. This is a practical benefit during a
cholera epidemic.
DOES TEETHING CAUSE DIARRHOEA? I would like your advice on a question which comes up often in my work. There is a
strong belief here that the emergence of a child's first milk teeth causes diarrhoea. It
is extremely difficult for me to convince mothers that this is not so. I received no
education about how to do this during my training. Boyd Kumwenda, Clinic Assistant, Fulaza Clinic, PO Box 540089, Chama, EP, Zambia.
Dr Dhiman Barua, formerly of WHO, replies: There is no scientific evidence that teething itself causes diarrhoea. However,
diarrhoea is common at the time of teething. This is probably because teething coincides
with the weaning period, when the child is exposed to infection through new foods and
feeding methods. Also, children who are teething often put things in their mouths to chew.
This is another way in which germs are transmitted. An episode of diarrhoea at the time of
teething should be treated in the same way as diarrhoea at any other time. Diarrhoea
during teething should never be neglected because it is thought to be 'normal'.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Executive editor Kate O'Malley
Design & production Ingrid Emsden
Editorial advisory group
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Dr Shanti Ghosh (India)
Dr Nicole Guérin (France)
Dr Norbert Hirschhorn (USA)
Dr Sharon Huttly (UK)
Dr Claudio Lanata (Peru)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Professor Dang Duc Trach (Vietnam)
Professor Andrew Tomkins (UK) With support from AID (USA), Charity Projects (UK),
Ministry of
Development Cooperation (Netherlands), ODA (UK),
SIDA (Sweden), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Turkish Medical Association (Turkey)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 52 March-May 1993
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 4 March, 2016
updated: 4 March, 2016
|