|
| |
Issue no. 31 - December 1987
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 31 - December
1987
|
DDOnline Dialogue
on Diarrhoea Online Issue 31 December 1987  Page 1 2
Page 1 2
Diarrhoea and city children
Oral rehydration therapy (ORT) must always be the first response to acute diarrhoea in
all settings. Giving appropriate fluids by mouth in adequate amounts prevents or cures
dangerous dehydration due to diarrhoea. Each year millions of young children in both urban
and rural areas of developing countries owe their lives to the spread of knowledge about
ORT through international, national and local diarrhoeal disease control programmes. Complications of prevention
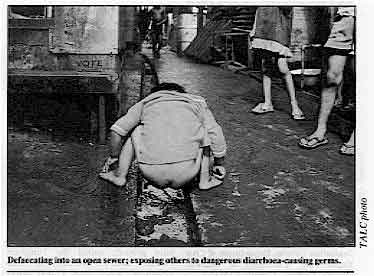
Preventing the spread of diarrhoeal infections is more complicated than preventing
their effects. Diarrhoea-causing bacteria, viruses and parasites are passed in faeces and
remain active for varying periods of time according to environmental circumstances.
Transmission of diarrhoeal diseases greatly diminishes where disposal of faeces is at a
safe distance from drinking water supplies and where people understand the importance of
hygiene, especially handwashing. Realities of urban poverty In the countryside there is enough space for simple sanitation methods to work well.
But space is a luxury among the urban poor. Yet the drift to the cities increases all the
time and it is predicted that, by the year 2000, more than 50 per cent of people in the
world will live in urban areas.
|
Defaecating into an open sewer; exposing others to dangerous
diarrhoea-causing germs.
Health risks increase wherever large numbers of people live in makeshift housing or
established slums, without proper water supplies, sanitation and drainage.
|
 |
Malnutrition and infections, particularly recurrent diarrhoea and acute respiratory
illness (see="#page6">page 6), threaten the survival of all poor city
children; and the need to earn money outside the home discourages many mothers from
breastfeeding. Need for innovation This issue of DD brings us to the end of 1987, designated as the International
Year of Shelter for the Homeless. Shelter for the urban poor is more often than not
atrocious and contributes to ill health. Improvements will only come about through
innovative approaches and integration of environmental, economic and other social welfare
programmes together with maximum community involvement. Meanwhile progress can be achieved
in the control of diarrhoea through simple interventions at family and community level and
suggestions for these are described in the insert in this issue. KME and WAMC
|
In this issue . . .
- Diarrhoea in urban slums
- Practical insert: water and sanitation
- CDD and ARI joint activities report
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 31 December 1987  1 Page 2 3 1 Page 2 3
Announcements A symposium on "Chronic Diarrhoea Associated with Carbohydrate Intolerance"
will be held at the Children's Nutrition Research Center, Baylor College of Medicine,
Houston, Texas from November 30 to December 2 1988. The organisers will welcome original
contributions in four poster workshops: Epidemiology, Treatment and Prevention, Histology
and Immunology. For more information contact: Dr Carlos Lifschitz, Children's Nutrition
Center, 6621 Fannin Street, Houston, Texas 77030, USA. The Department of Civil Engineering at the University of Ottawa will be offering a 4
day intensive course on 'Water Supply and Sanitation for Developing Countries' from June
6-9, 1988. This will cover low cost, renewable energy technologies and economic and
socio-cultural aspects of technology implementation. cost: $250 (Canadian) for those
attending the VIth IWRA World Water Congress, and $400 (Canadian) for others. For further
details, please contact: Dr Ron Droste, Water and Sanitation Course, Department of
Civil Engineering, University of Ottawa, Ottawa, Ontario, Canada K1N 6N5. Brazil: community financing The Fundacao Servidos Especiaias de Saude Publica (FSESP) has assisted over 1,000
communities in Brazil to install water and sewerage systems. FSESP has helped to create
municipal authorities with paid employees, to manage these systems and where necessary
provide technical and economic support. Most smaller communities' water systems were
financed by loans from development banks. Interest payments, operation and maintenance
costs were paid by charging users. Rates for the use of the water and sewerage systems
were based on the minimum salary in Brazil, adjusted for inflation, and were set to favour
poor household users rather than large commercial users. It was found that small Brazilian
communities are able to pay for maintenance and operation of water supplies if a suitable
financing system is used. This approach has been very successful and has in some cases
generated surplus cash, used to expand the systems. It seems that water supply coverage
can depend more on the method and efficiency of billing and collection than on the wealth
of the community and the amount charged for water. Taken from a report by Primary Health Care Operations Research (funded by USAID).
Further information available from PRICOR, 5530 Wisconsin Avenue, Chevy Chase, Maryland
20815, U.S.A. Thailand: village water tanks In Thailand, only about 25 per cent of people in rural areas have access to safe water.
In the north east, the country's poorest and driest area, villagers may have to walk up to
five kilometres a day to find water, often from open sources, which are also used by
animals. In 1980 the Population and Community Development Association (PDA) started a rainwater
catchment pilot project, called the Tungnam (' water tank') Project, in two provinces.
Since then 12,000 water tanks have been built by villagers under the guidance of the PDA
to collect rainwater from household roofs and store it for later use during the dry
season. Village participation is encouraged in several ways:
- payment does not have to be made by the household until after the tank has been built;
- villagers hold meetings two or three weeks before construction to discuss the project,
health aspects, building techniques and the responsibilities of the PDA and the villagers;
- villagers who have building skills are asked to become volunteer technicians assisting
with maintenance of the water tanks.
During the harvest season villagers often work together and help each other. This same
group co-operative spirit is easily carried over to the building of water-tanks. Payment When a tank has been completed the owner is expected to pay for all material and
construction costs. They can choose to pay a lump sum or monthly interest-free
installments. Almost every family has paid for their water tank. The total cost for a
bamboo reinforced tank is approximately 4,500 Baht (U.S. $173). Last year the PDA
introduced a steel reinforced tank which is slightly more expensive. Money received from
new owners is placed in a revolving fund, which is used to construct tanks in other
villages. The tank The water tanks hold approximately 11.3 cubic metres of water, enough to supply one
large or two small families during the dry season. There is a bypass drainage system to
remove grit and other impurities from the roof. When it rains, the first run-off from the
roof is caught in the sediment trap and cannot enter the storage tank. Once the trap is
full, water overflows into the storage tank. When the rain stops, a plug at the bottom of
the sediment trap opens to let the impure water escape. Replacing the plug makes the
sediment trap ready for the next rain. The PDA also provides other help with water supplies and storage such as giant water
jars, shallow wells and the construction and improvement of village ponds. Tavatchai Traitongyoo, Population and Community Development Association (PDA), 8
Sukhumvit, 12 Bangkok 11, Thailand. Waterlines, April 1987. Laboratory aids To assist in the microscopial diagnosis of tropical diseases and anaemia, a Bench Aid
Series (Price: £7.40 including postage and packing for a complete set) and two plastic
coated colour wall charts (£3.50 per pair) are now available from Monica Cheesbrough,
Tropical Health Technology, 14 Bevills Close, Doddington, Cambridgeshire, PE15 OTT,
England. A revised edition of Manual for Laboratory Investigations of Acute Enteric Infections
(Ref: CDD/83.3 Rev. 1 (1987) is now available free of charge from CDD/WHO, 1211 Geneva
27, Switzerland.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 31 December 1987  2 Page 3 4 2 Page 3 4
| Poor urban neighbourhoods |
Water and sanitation "do's and don'ts" Jim Arthur and Kevin Tayler
outline some important considerations for planning urban water and sanitation
improvements. These are intended to be a source of ideas rather than a rigid set of rules. In recent years, there has been a welcome emphasis on the effects that improved water
supply and sanitation can have on health. This has led to many initiatives to improve
facilities, especially in rural areas. Unfortunately, less attention has been paid to the
situation in low income urban communities.
|
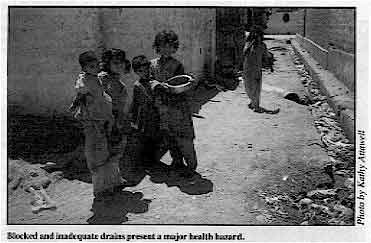
Blocked and inadequate drains present a major health hazard.
In fact, poor urban neighbourhoods are particularly at risk from poor water and
sanitation facilities as the crowded conditions increase the chances of disease
transmission.
|
 |
There is an urgent need for action in such areas but our experience is that this action
must be co-ordinated if it is to be effective. Isolated actions, for example, the
introduction of piped water supplies in areas with inadequate drainage, can in some cases
actually worsen conditions. With the above points in mind, here is a basic list of do's and don'ts:
- Do involve the community.
You can learn from the community through formal surveys but also and equally important,
from group discussions and by talking to people informally in order to find out about
their ideas and needs and, not least, their current responses to and ways of dealing with
their situation and problems. The best solutions to problems are not always produced by
outside experts and never by those who do not take the trouble to learn.
- Do consider how facilities are to be operated and maintained.
In general, the simpler the system the better, but remember that septic tanks have to be
emptied from time to time, water mains repaired, pumps maintained and so on.
- Do introduce public health education to improve hygiene before or
alongside facilities.
Without this, people are unlikely to use or care for equipment properly, and the potential
improvement in community health will not be realised.
- Do consider whether or not facilities are affordable, and how people will pay for and
maintain them.
Expensive one-off schemes which cannot be repeated because they are unaffordable
should be avoided.
- Do think ahead.
Solutions which seem practical today may prove inadequate as communities develop. It is
sometimes possible to adopt a phased approach; for instance, providing on-plot sanitation
facilities which can be adapted to fit into a water-borne sewerage scheme when the level
of water provision makes sewerage possible and desirable.
- Do consider the overall situation.
Will increased water supply result in ponds of stagnant water and an increase in
mosquito-related disease? Will drains be blocked because no provision has been made for
solid waste collection? Will more widespread water-borne sanitation result in higher
concentrations of faecal material in open drains?
- Try not to have pre-conceived ideas about appropriate actions.
The situation in an African town with large plots of land (e.g. 400 square metres) and
poor water supplies is quite different from that in crowded Asian cities where plot sizes
may be much smaller (50 square metres or less). Pit latrines may be the best sanitation
option in the first case but they are unlikely to be feasible in the second.
- Don't have a rigid approach.
If possible, try out ideas on a pilot basis and alter them as necessary in the light of
experience. Pilot schemes can be particularly important in introducing ideas to the
community and gaining their trust. On the other hand, do not forget the scale of the
problem or make do with token solutions. Also, beware of introducing completely untried
methods which may reduce community confidence if they go drastically wrong.
Jim Arthur and Kevin Tayler are engineers working with Gilmore Hankey Kirke, a
multi-discipline consultancy specialising in urban planning and development, with special
emphasis on the needs of the urban poor. They are currently working in Peshawar, Pakistan,
and have wide experience in water and sanitation programmes in the Philippines, Nigeria,
and Egypt.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 31 December 1987  3 Page 4 5 3 Page 4 5
Bombay
Urban growth in many countries is unprecedented. People move to cities to find
work and a better life, often making their homes in slums and squatter settlements. Gopa
Kothari describes the health problems associated with living in Bombay's
slums.
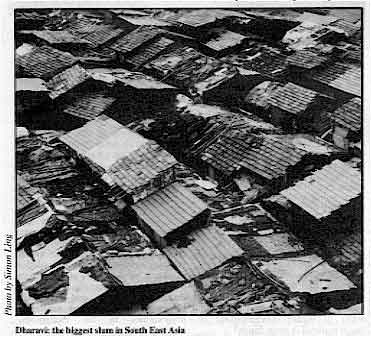 |
Dharavi: the biggest slum in South East Asia
Bombay is one of the most developed, cosmopolitan cities in India. Nearly half the
population live in slums; 400,000 of them in Dharavi, the biggest slum in South East Asia,
and in 500 other shanty colonies. These slums are characterised by unhygienic living
conditions, overcrowding, poor housing and lack of basic amenities.
|
In addition, slum dwellers are caught in a vicious cycle of low income and insecurity
leading to a situation of permanent poor health.
|
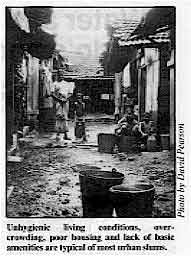
Unhygienic living conditions, over-crowding, poor housing and
lack of basic amenities are typical of most urban slums.
Health hazards are directly related to poverty, a polluted and stressful environment,
social instability and insecurity. People living in the slums are more vulnerable to
communicable diseases and malnutrition. Women of child bearing age and children are
particularly at risk.
|
 |
Child health The health of children below three years of age is closely related to the poor living
conditions and lack of hygiene. Shortage of water, open drains, inadequate latrines, piles
of rubbish and human excreta encourage flies to breed and spread diseases like diarrhoea
and dysentery. Frequent episodes of diarrhoea during early childhood often contribute to
malnutrition, which increases the severity of diarrhoea, thus setting off a vicious cycle.
Although living in an urban area, the slum dwellers share similar socio-cultural values to
people living in rural areas. Their beliefs, customs and values affect the health and
health care of young children. One common practice is to withhold breastmilk and food
during diarrhoea and to give unsuitable home remedies. The incidence of infectious diarrhoea is greatest at the time of weaning and is more
frequent during the monsoon and the summer. Poor maternal personal hygiene, for example
preparing food with hands and water contaminated with excreta, is also responsible for
diarrhoea in children. Working and bottle-feeding A survey carried out in various slums in Bombay found that, due to lack of money, 35-40
per cent of mothers start working again soon after giving birth. The infant is bottle-fed
by older sisters or brothers or other family members who do not always understand the
importance of bottle sterilisation and personal hygiene. While some mothers prolong
breastfeeding, they also use formula milk diluted with contaminated water. They also use
incorrect quantities because they do not know how to mix up formula milk.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 31 December 1987  4 Page 5 6 4 Page 5 6
Strategies to reduce diarrhoea Promotion and maintenance of breastfeeding is an important strategy in urban slums, to
reduce diarrhoea incidence, malnutrition and death during infancy. The traditional
practice of only putting the child to the breast on the third day after birth should be
replaced by putting the infant to the breast within hours of birth. Also important are the
adequate and timely supplementation of the infant's diet to prevent chronic malnutrition
and stunting, and improving literacy and health awareness in mothers. Many families do not
use oral rehydration for diarrhoea. However, oral rehydration can only prevent death from
dehydration, not the spread of diarrhoea. Female literacy The studies in the Dharavi slums have shown that educated mothers are more receptive to
health education messages. Messages have focussed on the importance of breastfeeding,
immunisation, simple hygienic measures like washing hands after using the toilet and
before handling food, using clean kitchen utensils, protecting food from flies and dust,
preparing oral rehydration fluids from locally available materials and adequate
supplementation of the infant's diet. Diarrhoea has diminished in the developed countries through safe drinking water, better
sanitation, improved food handling and other public health measures. Higher female
literacy rates in particular have also led to improvement in personal hygiene and better
child care. Diarrhoea control in urban slums requires a multi-pronged effort to increase literacy
among mothers - to improve awareness of the causes of diarrhoea, importance of early
rehydration, preparation of home made fluids for treatment, breastfeeding, proper weaning
and hygienic feeding habits. This must go hand in hand with implementation of better
public health services. Dr Gopa Kothari, Professor and Head, Department of Preventive & Social Medicine,
L.T.M. Medical College, Sion, Bombay, 400 022, India. Karachi
Lyari General Hospital in Karachi is situated in an urban slum and is used mostly
by people from the poorest families with low literacy rates. In one study the families who
came to the paediatric outpatients department were asked about diarrhoea and ORT, to find
out what they knew and where they had learned it. Most of the children attending were less
than 5 years old, had some malnutrition, and almost half of them had diarrhoea. Dr
Ali describes the results in this article.
|
Overcrowding in urban housing
When parents were asked what they thought had caused diarrhoea in their children,
almost half believed it was due to ignorance about hygiene, 18 per cent gave other reasons
such as artificial milk or teething, and 34 per cent did not know what causes diarrhoea,
although two thirds knew that diarrhoea can be serious and a cause of death.
|
 |
Treatment Although 68 out of 100 respondents were aware of the benefits of oral rehydration
therapy, the answers they gave regarding correct treatment for diarrhoea were as follows:
| Drugs and ORT |
63 |
| Drugs alone |
29 |
| ORT alone |
5 |
| Not known |
3 |
When asked specifically about ORT, 55 said that they would use oral
rehydration salts and 13 said they would use salt sugar solution. But nearly a third did
not know what they would use. Little more than half the families questioned said they had
learned about ORT through doctors and hospitals (see="#Source">table). Only a
few families had complaints about ORS, and these were only small problems. Three
complained that ORS tastes bad, two that it did not relieve the diarrhoea, and one that it
caused swelling around the eyes. Knowledge about ORT Over 40 of the families had access to radio or TV, and sometimes both, but few said
that they had learned about ORT through TV or radio. This is probably because government
media have only recently started to publicise ORS. The response however has been very
encouraging. Since the start of ORT publicity, awareness has definitely increased and
successful use of ORT has started to result in a decrease in morbidity in the under five
age group. Dr S M Inkisar Ali, Assistant Professor of Paediatrics, Dow Medical College,
Karachi, Pakistan.
Source of knowledge about ORS |
| Doctors |
38 |
| Hospital |
16 |
| T.V. |
6 |
| Radio |
3 |
| People |
4 |
| No knowledge |
42 |
More than one source in some cases. |
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 31 December 1987  5 Page 6 7 5 Page 6 7
| Acute respiratory infection and diarrhoea |
A natural collaboration
There are a number of similarities between the CDD and ARI Programmes. If these
similarities are recognised it should be possible not just for the ARI programme to
benefit from the experience of CDD, but for the two programmes to work together more
closely. The WHO Diarrhoeal Diseases Control Programme (CDD) has been operational since 1980.
Since that time nearly all of the countries of the developing world have planned and
implemented control programmes. While there remains a great deal of work to be done,
results so far are encouraging. At the end of 1985, the most recent year for which
statistics are available, 51 per cent of the developing world population has access to
Oral Rehydration Salts (ORS), and 18 per cent of childhood diarrhoea cases have been
treated with either ORS or a sugar-salt solution. This may have prevented 500,000
diarrhoeal deaths. Over 8,000 health staff have been trained in the CDD Supervisory Skills
training course, and a number of other training guidelines have been developed and used. Some of the features which the ARI and CDD programmes have in common are: the
importance of the diseases, an identical target population, primary emphasis on treatment
or case management, secondary emphasis on prevention, the basic simplicity of the
treatment intervention, the need for sound management and clinical training, the
importance of health education or communication, similar approaches to evaluation, and a
need for vaccine and clinical research. Importance Diarrhoeal diseases and acute respiratory infections each account for 3-5 million
childhood deaths a year. Thus, together these two disease groups are responsible for half
to two thirds of all the childhood deaths in the developing world. In terms of morbidity
they easily account for at least half of all visits to health facilities in many
countries. Target population Both programmes have as their target population children aged 0-4 years, although both
also address, as a lower priority, disease in older children and adults. Primary concern
is in those groups with the highest mortality rates. Not only are the target age groups
the same, but research results suggest that other variables, such as nutritional status,
family socio-economic status, and mother's literacy level, have a similar relationship to
severity and mortality for both diseases. Case management Both programmes emphasise improvements in treatment, particularly at health facilities,
as a critical strategy. This distinguishes them from others, such as EPI, which are
preventive. While everyone would prefer prevention wherever it is possible, in the case of
AR1 and CDD, prevention is clearly a long term effort, and proper treatment can save
millions of lives. There is also a distinct advantage in programmes based on treatment.
Whereas families may have difficulty in appreciating the relationship between an
intervention, such as vaccination, and the non-occurrence of an event, such as measles, it
is easy for them to appreciate the relationship between treatment and the immediate
improvement in the health of a sick child. These two programmes, because they are
curative, may be particularly important "entry points" for other elements of
primary health care. Prevention The CDD Programme has recently identified three strategies which appear to be
particularly cost effective approaches to prevention: good nutrition, particularly
breastfeeding and weaning; the use of adequate quantities of safe water; and personal and
domestic hygiene. Some of these strategies may be appropriate for ARI as well. The process
used to identify priority interventions, including careful review of the available
literature, could be useful in ARI. Simple interventions The use of ORS, when it is needed for the treatment of moderate dehydration, and the
administration of antibiotics, when they are needed for the treatment of moderately severe
lower respiratory tract infection, are both technologically simple and relatively
inexpensive. Management and technical training This is an area where the two programmes are already working very closely together.
When CDD developed its Supervisory Skills training course in 1983, it was designed to
cover all of the basic elements of supervision, such as planning, community involvement,
training, monitoring, and evaluation. It also included a module on the treatment of
diarrhoea, and a recent revision has added a module on prevention. ARI has added to the
common base provided by the Supervisory Skills course two modules which provide technical
guidelines on case management of children with cough, and ear, nose, and throat
infections. Increasingly, countries are choosing to use the full set of training materials
and this should lead to the integration of the skills taught in this course in control
programmes. Health education and communication If both programmes have the advantage of a simple intervention for treatment, they also
share a common problem - how to communicate the importance of receiving this treatment to
families. Specifically, both programmes need to learn more about the extent to which
families, particularly mothers, can be taught to do two things: first, recognise when
their child is not responding to simple or supportive measures intended to prevent mild
cases from becoming serious, and either take the child to a health worker or obtain
treatment elsewhere; and second, administer the treatment, ORS or antibiotics, correctly
for a long enough period of time. Joint exploration of these critical questions should be
very useful.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 31 December 1987  6 Page 7 8 6 Page 7 8
| Acute respiratory infection and diarrhoea |

ORS is estimated to have saved over half a million lives since 1980.
Evaluation As in the area of training. the evaluation methodologies developed by CDD should also
be useful for ARI programmes. Such methods as community surveys to measure morbidity,
treatment, and mortality; sentinel systems to monitor performance and output in selected
areas; and comprehensive programme reviews to provide a formal independent assessment of
programme accomplishments and problems, could all be adapted to include ARI as well as
CDD. Research While control programmes are being developed, based on technologies which are already
available, research to develop new technologies is needed by both programmes. CDD has now
funded over 300 research projects, and two of its three Scientific Working Groups are
responsible for research areas of particular relevance to ARI. The Immunology,
Microbiology and Vaccine Development SWG is actively supporting work on promising vaccines
against cholera, rotavirus, E. Coli, typhoid, and shigella. The Case Management SWG
is responsible for developing improved ORS formulations, and for investigating other
existing or new therapeutic agents. The interest of ARI in vaccine development and therapy
suggests that this is further ground for close collaboration. Given all these similarities between two of WHO's priority programmes, the interest to
see them working more closely together is natural. At global and regional levels, staff of
both programmes are increasingly coordinating their activities, and their priorities. At
country, province, district, and peripheral levels, the opportunities for not just
coordinating but combining these programmes into one delivery system would appear not only
desirable but inevitable. Integration of all the interventions and elements of primary
health care has been the subject of a great deal of discussion, but often the problems
inherent in such combined efforts are overlooked. In the case of ARI and CDD, however, the
advantages are so great that the opportunity for joint action should be recognised as a
priority for the immediate future. Robert Hogan, Programme Management Officer, Diarrhoeal Diseases Control Programme,
WHO, 1211 Geneva 27, Switzerland.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 31 December 1987  7 Page 8 7 Page 8
Asking too much I write to share a concern which is increasingly being voiced about the role of women
in health programmes. I hope that other DD readers may be able to suggest ways to
address this issue in policy and in practice. My concern is: what are the implications of requiring women to become extensions of the
health care delivery system in primary health care strategies; what are the realities for
mothers of giving ORT and do these realities affect ORT use? I wonder how many of us have
ever tried to spoon-feed a crying child who may have diarrhoea and is vomiting while
another child cries to be breastfed, with little time and many household chores to be
done. How many of us have had to deal with choices about resources as precious as water -
whether to rehydrate a sick baby or to feed the other children, for example? Those
involved in diarrhoeal disease control programmes, whether as planners, policymakers, or
practitioners, need to look at these realities practically and with sensitivity to women's
lives. We must also address the burdens as well as the benefits of innovation and improved
technologies. EIayne CIift, Deputy Director, HEALTH-COM, Academy for Educational Development, 1255
23rd Street, NW, Washington DC 20037, U.S.A. Learning through doing The National Rehydration Treatment and Training Centre at the San Lazaro Hospital in
Manila, the Philippines, ran its ninth national training course in August 1987.
Participants in this clinical case management course were regional training and CDD
coordinators who learned the skills of oral rehydration therapy (ORT). One of the
practitioners, Dr Cynthia J. Javelosa of the Western Visayas Medical Centre in Mandurriao,
Iloilo City, describing the previous day's experience in her presentation said: "The
actual handling of cases is indeed a good way for us to acquire the knowledge and skills
of clinical management of acute diarrhoea - the ORT way. For some of us, it has been a
means of knowing what our mistakes in the field have been, for others, it has been a new
experience to discover that ORT is not synonymous with ORS alone.
|
Learning
the skills of oral rehydration therapy.
And for some it has been an experience of "seeing is believing" the actual
effectiveness of ORT, convincing us that ORS does not only save time and money, but most
important - people's lives. This reminds me of a Chinese saying "to save a single
life is better than building a seven floor pagoda". It is with hope that when we go
back to our respective regions, whatever knowledge and skill we acquire from this training
will be effectively and efficiently put into actual practice, so that in time we shall be
able to say that: "our pagoda has been built" - this will be our true
legacy."
|
 |
Dr Mariam Claeson, International Child Health Division, UppsaIa University, Sweden. Editors note: See="dd29.htm">DD issue 29 Drugs, diet and diarrhoea I work in a suburban and rural part of South India. Diarrhoea remains the major cause
of mortality and long term morbidity in children. Yet, understanding of the disease and
its management is still lacking among the majority of general practitioners. Many doctors
still believe in giving combinations of too many medicines to stop diarrhoea. The self
limiting nature of most diarrhoeal illnesses is forgotten and use of too many drugs with
peculiar combinations and frequent changes leads to complications. Another problem with
doctors is their advice regarding diet. Emphasis is not given to a nutritious dietary
regimen. A bland diet such as gruel is often prescribed as the only food. I feel that DDneeds to reach every family physician. It will go a long way in eliminating these
pitfalls in the management of diarrhoea. Dr P Natarajan, No. 18 Nehruji Road, Villupuram, 605602, India. Public latrines Do any of your readers have any experience or ideas about building public latrines in
urban areas, and helping to set them up as 'small businesses', with customers (including
possibly tourists) being charged to use them? The funds could then be used to provide
income for the owner/keeper and to provide cleaning materials. Might there be a positive
health effect on the surrounding area? Would people pay to use a clean public latrine? Ms. Carrie Osborne, PO Box 4231, Kathmandu, Nepal.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 31 December 1987
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
updated: 23 April, 2014
|