|
| |
Issue no. 37 - June 1989
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 37 - June 1989
|
DDOnline Dialogue
on Diarrhoea Online Issue 37 June 1989  Page 1 2
Page 1 2
Persistent diarrhoea
Most episodes of diarrhoea are acute - they start suddenly and are quite short, lasting
between two and seven days. Most are due to infections in the bowel. A proportion of acute
cases, about one in ten, become persistent, lasting more than two weeks. Their importance
is that they account for almost half of diarrhoea deaths. They also require extra
treatment in addition to the oral rehydration therapy which is so effective for most cases
of acute diarrhoea. Chronic diarrhoea, which does not start with an acute infectious
episode, may be due to a variety of metabolic or structural conditions or to parasitic
infections. Chronic diarrhoea, which can often continue for months and years, is a
different type of problem from persistent diarrhoea and is not considered in this issue.
 |
Continued feeding is essential for treating both acute and
persistent diarrhoea. Clean and appropriate food A most important aspect of the management of persistent diarrhoea is appropriate diet.
This issue of DD concentrates on the linked themes of persistent diarrhoea
and dietary management. It includes a report of an important WHO meeting and an article on
the dietary management of diarrhoea.
|
Lactose intolerance Lactose or milk sugar, is the main carbohydrate source of energy for infants. Lactase,
the gut enzyme required to digest and absorb lactose, is easily damaged by infections and
malnutrition. How important is lactose intolerance, how is it diagnosed and managed? A
number of readers have asked these questions to which DD replies on="#page6">page 6. WAMC and KME
|
In this issue:
- Persistent diarrhoea and dietary management
- Lactose intolerance
- Health Basics: Breastfeeding
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 37 June 1989  1
Page 2 3 1
Page 2 3
| WHO: Meeting report and guidelines |
WHO meeting on
Persistent Diarrhoea in Developing Countries
(WHO/CDD/88.27) Children in developing countries may experience as many as ten episodes of acute
diarrhoea per year. The vast majority of these episodes can be successfully treated with
oral rehydration therapy (ORT) and continued feeding. Antibiotics should be used only for
dysentery or suspected cholera. What is less certain is what to do if the diarrhoea does
not stop. If diarrhoea lasts for more than two weeks (persistent diarrhoea) the effect
upon nutritional status may be especially serious, and the chances of death increase as
much as 20 times. Studies from various developing countries have shown that between three
and 20 per cent of episodes of acute diarrhoea become persistent, and up to one half of
all diarrhoea-associated deaths occur during episodes of persistent diarrhoea. The World Health Organization held a meeting of paediatricians, epidemiologists,
nutritionists and microbiologists to summarise current knowledge of persistent diarrhoea
and define research priorities. Although many of the studies reported were incomplete,
certain preliminary conclusions could be drawn. Risk factors
- 1. Age
Persistent diarrhoea occurred most frequently during the first year of life when, in
healthy infants, rates of growth and weight gain are most rapid.
- 2. Malnutrition
Persistent diarrhoea causes more malnutrition than acute attacks. The mean duration of
episodes of diarrhoea in malnourished infants was also longer than in adequately nourished
children.
- 3. Impaired immune defences
The risk of persistent diarrhoea was also increased by impaired immunity (as measured
by skin testing). Presumably a healthy immune system is required to fight off gut
infections. Measles and malnutrition, which can damage immunity, did not appear to be the
cause of defective immunity in these studies.
- 4. Previous diarrhoea
Children who had recently had an episode of acute diarrhoea or who had ever experienced
persistent diarrhoea were more likely to have persistent diarrhoea in future. This may be
because of damage caused to the gut by the previous episode, or some other change in the
child's defences against infection. Other infections do not predispose to persistent
diarrhoea.
- 5. Specific gut infections
Infection with certain micro-organisms (especially Shigella, enteropathogenic E
coli and, in malnourished children, cryptosporidium) appears to increase the
risk of persistent diarrhoea. Increased numbers of bacteria which normally grow in the
large intestine have been found in the small intestine of infants with persistent
diarrhoea, but it is not known whether this abnormal colonisation caused the diarrhoea to
go on longer.
Treatment Continued feeding is an essential part of the treatment of persistent diarrhoea, to
counter the impact of persistent diarrhoea on nutritional status and maintain hydration.
Persistent diarrhoea affects nutrition because of:
- decreased intake of food;
- impaired absorption of food;
- loss of nutrients from the body through the damaged lining of the intestine; and
- increased energy requirements because of fever or the need to repair intestinal damage.
Food Breastfed babies should continue to breastfeed during persistent diarrhoea. Children
with persistent diarrhoea may be intolerant of animal milk because of their inability to
digest lactose; this is most likely to be a problem when the child's diet consists
entirely of milk from animals. Decreasing the lactose content of animal milk by the
traditional method of yoghurt making may be beneficial in some patients. When this is not
effective, soy milk, which contains neither lactose nor milk proteins, can be tried. For
children above six months of age, weaning foods which are locally available, high in
energy, low in bulk, nutritious and culturally acceptable, are recommended. Alternatively,
a diet based on finely ground chicken may be tried. Vitamins such as A, folic acid and
B12, and minerals such as zinc and iron may help the repair process of the gut and boost
immune defences. Rehydration Hydration is maintained by giving extra drinks and ORS if needed. Very occasionally a
child may fail to absorb glucose and require intravenous fluid. Antimicrobials and other medicines Antibiotics are currently reserved for dysentery (diarrhoea with blood and pus in the
stools). Use an antibiotic to which most Shigella strains in the community are
sensitive. Studies are in progress to define more accurately the possible role of
antibiotics for other specific infections in persistent diarrhoea, for example in
enteropathogenic E coli infections, for which oral gentamicin may shorten the
duration of the illness. Other drugs are of no proven benefit. Research priorities
Further research is required into all the areas discussed above, but the following were
highlighted. 1. Epidemiology Community based studies are required to define the relationship of persistent diarrhoea
to age, season, infectious agents, morbidity and mortality and to define risk factors for
persistence. 2. Infection and immunity
- Does the type of micro-organism present in the small intestine or stool culture during
acute diarrhoea determine whether the illness will become prolonged?
- Is there a role for antibiotics and other drugs in the treatment of persistent
diarrhoea?
- Can the risk of persistent diarrhoea be reduced by appropriate feeding and the use of
cereal-based oral rehydration solutions, rather than standard ORS, during acute diarrhoea?
The death rate from acute diarrhoea can be cut by ORT. The next challenge is to reduce
mortality due to persistent diarrhoea. It is hoped that the recommendations and research
generated by this meeting will help to meet this challenge. A full report of the meeting
was published in the Bulletin of the World Health Organization 66: 709-717 1988. Professor David Candy, Department of Child Health, King's College Hospital, London
SE5 8RX, UK.
WHO Guidelines Nutritional management of persistent diarrhoea
There have been few studies of the dietary management of persistent diarrhoea, but
experience in the nutritional therapy of acute diarrhoea, of chronic diarrhoea of infancy
in industrialised countries, and of severe protein-energy malnutrition provides valuable
guidance. Several clinical studies have shown that continued feeding during acute
diarrhoea results in improved nutritional outcome and, in some cases, less severe
diarrhoea. Although the benefits of continued breastfeeding in persistent diarrhoea have
not been determined, it is recommended that breastfeeding be maintained during such
episodes. Weaning foods
Studies during acute diarrhoea and experience gained in the rehabilitation of severely
malnourished children show that weaning mixtures prepared from locally available foods are
generally well tolerated. These food mixtures should be energy-rich, have low viscosity,
and have low osmolality. In selecting a diet: complementary protein sources should be
used; complex carbohydrates (starches) should be used to avoid hyperosmolality and reduce
the problem of lactose maldigestion - e. g. milk-cereal mixtures are preferable to milk
given alone; and fats that are most readily digestible should be preferred, especially as
a means of increasing the energy intake. Giving small feeds more frequently during illness
may help to maximise nutrient absorption Vitamins and minerals Folate, zinc, iron, vitamin B12, vitamin A, and possibly other micro-nutrients are
involved in intestinal mucosal renewal and/or a variety of immunological responses.
Supplementary vitamins and trace elements should be given during persistent diarrhoea, if
possible. Milk from animals Animal milk should not be routinely restricted during the treatment of acute diarrhoea.
Nevertheless, in some infants with persistent diarrhoea, milk intolerance plays an
important role in prolonging diarrhoea. This occurs mostly in infants who receive animal
milk as the sole food. Reducing the amount of lactose in the diet can reduce the severity
and possibly the duration of persistent diarrhoea. Convalescent feeding Appropriate nutritional therapy during convalescence ensures that children return at
least to their pre-illness nutritional state. Studies have shown that the desired level of
energy intake (420-670J/ kg/ day) can be achieved by children who are given energy-rich
(low bulk), low viscosity diets. This level of intake can promote a rate of growth far in
excess of that expected for normal children of the same age group, thus achieving rapid
nutritional recovery. CDD Update, No. 4, March 1989, WHO, Geneva
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 37 June 1989  2
Page 3 4 2
Page 3 4
A source of faecal contamination
Baby feeding bottles are a dangerous source of diarrhoea germs. Claudio
Lanata reports from Peru. Several risk factors for diarrhoea have been identified and have been the focus of
specific interventions to reduce diarrhoeal diseases. These include contaminated water,
improper disposal of faeces, poor hygiene practices, and contaminated foods. In a recent
study of 153 children living in a poor community on the outskirts of Lima, Peru, (1)
in which we looked at the preparation and administration of weaning foods in the first
year of life, an important vehicle of faecal contamination was identified: the baby
bottle. The dangers of this must be emphasised because of the widespread use of feeding
bottles in many developing countries where diarrhoeal diseases are endemic. Contrast with cups The first clue came when microbiologic cultures were taken of foods given to children
at different times during preparation. For example, teas, which were often given,
beginning in the first month of life, had a low frequency of contamination immediately
after heating (three per cent of 87 samples) (1). If served in a cup, teas also had low
levels of contamination at the time of consumption (two per cent of 49 samples). However,
if served in baby bottles, a high frequency (31 per cent of 74 samples) were contaminated
with faecal germs, most of them with colony counts of 10,000 or more per
millilitre. When several household articles used for food were cultured, the items most frequently
contaminated with faecal coliforms were bottle nipples (37 per cent of 26 samples) and
feeding bottles (23 per cent of 26 samples) when, according to the child's mother, these
were supposed to be clean. In contrast, the mother's hands were less frequently
contaminated (14 per cent in 78 samples) and the nipples of the mother's breasts very
rarely (three per cent of 64 samples). Difficult to clean
This high level of contamination of bottle nipples and feeding bottles is most likely
due to the difficulty in cleaning them in unhygienic environments, where water is scarce
and expensive and usually contaminated, as is the case in this Peruvian community. Foods,
such as animal milk, are contaminated by the bottles which also allow the bacteria to
grow, especially if left at room temperature for more than one hour, as was documented in
this study. Recommendations
The main conclusion is that the promotion of exclusive breastfeeding during the first
four to six months of life will eliminate the feeding bottle as a source of faecal
contamination during this period. But, because breastmilk is not sufficient by itself to
satisfy the nutritional requirements of infants after this age, other foods must be
introduced while continuing breastfeeding. These foods should be given using cups or
dishes that are easier to clean and less likely than bottles to be contaminated. There is
no need to use a baby bottle. The use of baby bottles should be completely eliminated. This will not only reduce the
frequency of consumption of contaminated weaning foods, but will also help to maintain
breastfeeding, resulting in a better infant diet. Reference
1. Black, R E et al. Incidence and etiology of infantile diarrhoea and major routes
of transmission in Huascar, Peru. Am. J. Epidemiol. In press. Dr Claudio Lanata, Director General, Institute de Investigacion
Nutricional,
Apartado 55, Miraflores, Lima, Peru
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 37 June 1989  3
Page 4 5 3
Page 4 5
Appropriate dietary management
Dr Roy and Dr Haider describe
the relationship between persistent diarrhoea and malnutrition, and the types of food to
give a child who has persistent diarrhoea. Persistent diarrhoea is a syndrome in which an acute episode of diarrhoea continues for
more than 14 days. The causes of persistent diarrhoea are complicated, and relate to
previous history of illness, diet, nutritional status and immune status. Management of
cases of persistent diarrhoea may be difficult due to lack of diagnostic facilities, and
absence of well defined guidelines for treatment. Many of these children have associated
malnutrition, resulting from reduced food intake and/ or loss of nutrients through
diarrhoea. Nutrient loss may also be due to damage to the digestive system resulting from
diarrhoeal infection, or malnutrition. In a recently completed study in Bangladesh, severe
loss of nutrients was recorded in patients with persistent diarrhoea. Persistent diarrhoea and malnutrition
Since diarrhoea not only causes but also worsens malnutrition, a prolonged diarrhoeal
episode has a more damaging effect on the nutritional status of the child. Severe
deficiency of energy, protein and micronutrients often leads to kwashiorkor or marasmus in
a child who is already undernourished.
 |
Management of persistent diarrhoea includes correction of
dehydration with ORT. It is known that malnourished children have more problems of digestion and absorption,
which may become worse during diarrhoea. Persistent diarrhoea is therefore a major cause
of malnutrition and subsequent death.
|
Prompt and effective intervention with an appropriate diet is a key factor in
management of persistent diarrhoea (1). Experience with persistent diarrhoea patients at
the International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR, B) treatment
centre has helped us to develop some case management procedures that may be helpful for
other countries. General management includes:
- correction of dehydration, and maintenance of hydration, with oral or intravenous
rehydration solution;
- treatment of other infections, like acute respiratory infections, urinary tract
infection, otitis media and other systemic infections which are present in many cases (2);
- observation of the volume, consistency, and frequency of stool, preferably in a
treatment centre.
A simple bedside test can be used for diagnosing carbohydrate malabsorption. If the
stool pH is less than 5.5, and stool reducing substances are more than 0.5 per cent,
carbohydrate malabsorption may be diagnosed. Choice of diet
Breastfeeding should be continued and encouraged in persistent diarrhoea patients.
Proper choice of diet requires understanding the digestive capacity during persistent
diarrhoea. Foods chosen should be easy to digest and absorb (to avoid osmotic effect),
contain adequate nutrients, and be non-allergenic, energy-rich, and acceptable to the
child. In selecting a diet: (i) complementary protein sources should be used;
(ii) complex carbohydrates (starches) should be used to avoid hyperosmolality and
reduce the problem of lactose maldigestion - e. g. milk-cereal mixtures are preferable to
milk given alone; and
(iii) fats that are most readily digestible should be preferred, especially as a means
of increasing energy intake.
|
Continued feeding prevents the malnutrition which can
result from persistent diarrhoea. Foods used should also be available, not too expensive, and culturally acceptable.
Children with persistent diarrhoea are very often anorexic and dietary management of these
children may be difficult at the beginning. This can be overcome in most cases by giving
frequent small feeds during the first few days.
|
 |
In the developed countries, a wide range of commercially available prepared diets is
available, but there are only a few in developing countries (and these are usually
expensive). The reduction of usual lactose content in milk formula for children whose sole
source of protein is milk may some-times help to resolve diarrhoea. If reduction of the
lactose content in cow's milk (by providing mixtures containing milk and staple food
products, or by decreasing the lactose in animal milk - for example by traditional
fermentation) does not bring any improvement, the next step in management would be to give
a milk-free diet using soya based formula, or a cereal based diet. Recently at the
ICDDR,
B a cereal based liquid formula made with inexpensive, locally available ingredients (rice
powder, soya oil, glucose and egg protein) has been used successfully. Eighty one per cent
of patients over three months of age improved within five days. Another milk-free diet
prepared with rice-dahl (lentils) mixture has also been used successfully in India.(3)
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 37 June 1989  4
Page 5 6 4
Page 5 6
Severe cases Most children respond to this dietary regime. However a small proportion of children
with severe persistent diarrhoea (high stool volume and marked weight loss) may require
specialised treatment in hospital and further modified diets, like a comminuted (finely
chopped) chicken diet. Though it is efficient for management of severe cases, this diet is
too expensive and difficult to prepare at home for most people in developing countries. Patients who fail to respond to the reduction of the lactose content of the diet, and
cereal based or comminuted chicken diets can be given a commercially available casein
hydrolysate formula, 'Pregestimil' (Mead Johnson and Co). If there is no improvement in
diarrhoea a week after the introduction of these diets, other underlying causes of
diarrhoea should be investigated. These include small bowel bacterial overgrowth, severe
enteropathy, monosaccharide intolerance and organic disorders. Most children will respond
to specific dietary and/or antimicrobial therapy. However, some with very severe food
intolerance, will be unable to take food orally and will have to receive intravenous
alimentation for several days or weeks, before progressive amounts of readily absorbable
nutrients can be administered orally. If the diarrhoea stops with any of the above mentioned diets, continue with the same
diet for a minimum of two weeks. Subsequent follow-up at weekly intervals is necessary to
monitor growth and the gradual transition to normal foods. Vitamin A, folic acid and zinc should be given routinely as these patients are usually
deficient in these essential micronutrients. Although persistent diarrhoea is a challenging problem, when treatment is based on
appropriate nutritional therapy, the results can be very encouraging. References I. Roy, S K et al., 1989. Persistent diarrhoea: a preliminary report on clinical
features and dietary therapy in Bangladesh. J. Paediatr. 35.
2. Roy, S K et al., 1988. Persistent diarrhoea syndrome (PDS) among Bangladeshi
children. Abstracts of the XII th International Congress for Tropical Medicine and
Malaria, 1988: 212.
3. Bham, S A et al., 1983. Protracted diarrhoea and its management. Indian
Paediatr.
20 (3): 173-8. R Haider (Research Physician) and S K Roy (Associate Scientist),
International Centre for Diarrhoeal Disease Research, Bangladesh, GPO Box 128, Dhaka 1000,
Bangladesh
|
Composition of
diets used in persistent diarrhoea ( / Iitre )
|
| Half strength rice suji |
Half strength comminuted chicken |
| Rice powder |
30g |
Chicken, minced |
90g |
| Egg albumin |
15g |
|
|
| Oil (soya) |
20ml |
Oil (coconut, soya) |
20ml |
| Glucose |
25g |
Glucose |
30g |
| Potassium chloride |
1g |
Potassium chloride |
1g |
| Sodium chloride |
1g |
Sodium chloride |
1g |
| Magnesium chloride |
0.5g |
Magnesium chloride |
0.5g |
| Calcium chloride |
1g |
Calcium chloride |
1g |
| Water up to |
11 |
Water up to |
11 |
| |
|
|
|
| Energy |
400 kcal |
Energy |
380 kcal |
| Osmolality |
280 mosmol/ kg |
Osmolality |
218 mosmol/ kg |
|
DDOnline
Dialogue on Diarrhoea Online Issue 37 June
1989  5 Page 6 7 5 Page 6 7
Lactose intolerance
I work in a teaching hospital in Orissa, south east India, where treatment of diarrhoea
and its complications demands a large share of my time. I am concerned by the increasing
incidence of lactose intolerance, particularly in malnourished children. It is essential
to give milk to these babies to break the vicious circle of diarrhoea and malnutrition,
and using soya milk is very costly. It is very distressing that we are sometimes forced to
stop even breastmilk temporarily due to the severity of the diarrhoea. I would very much
like to know if it is possible to obtain lactase, which seems to be the ultimate solution
to this problem. Dr P Suvarna Devi, Assistant Professor, Dept of
Paediatrics, M K C G Medical
College, Berhampur 760 004, Orissa, India
Acute gastroenteritis sometimes leaves young infants with secondary
complications such as malabsorption and malnutrition. It is necessary to stress good
dietary advice so that the child does not develop malnutrition. Breastfeeding is most
important in this situation.
 |
For infants with acute diarrhoea with temporary lactose
intolerance, breastfeeding should be continued. Some infants develop varying degrees of lactose malabsorption. Very few have a total
lack of lactase in the gut warranting elimination of lactose until such time as the gut
mucosa returns to normal. Some develop a moderate degree of lactase insufficiency that
requires short periods of withdrawal and gradual reintroduction of breastfeeds.
|
The majority of children will have a mild degree of insufficiency. They do well with
alternating breastfeeding with a lactose free cereal diet. The danger of permanent
discontinuation of breastfeeding should be prevented by proper education. The value of
lactose free cereal diets made of locally available grains needs no emphasis. The role of drugs in inducing lactose deficiency should be remembered before
prescribing them. There needs to be a balanced approach to dietary management during
diarrhoea. One cannot be so particular about breastfeeding in the presence of severe
lactose malabsorption. On the other hand, prescribing lactose free formulas, even for
trivial intolerance, is not warranted. It is better to use cereals and pulses as the best
supplementary foods in diarrhoea with lactose intolerance . Dr P Natarajan, Aswini Hospital, Villupuram 605 602, India
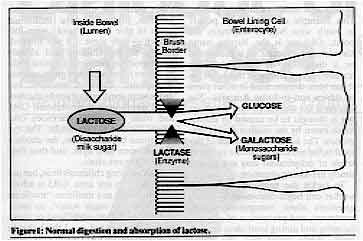
DD replies Lactose, or milk sugar, is a disaccharide carbohydrate and an important
constituent of both human and other milks. In the small bowel this is split by the enzyme lactase,
on the surface of the enterocytes, the cells lining the small bowel, into the
monosaccharide sugars, glucose and galactose (see="#Figure 1">Figure 1).
Malnutrition, bowel infections and certain drugs can damage the lining cells so that the
amount of lactase is reduced. This condition in children is called acquired or temporary
lactase deficiency. When someone with lactase deficiency has a lot of lactose sugar in
the diet, the bacteria in the bowel act on the sugar breaking it down into short chain
acids. These both irritate the bowel and limit absorption so that stools become acid and
watery (see="#Figure 2">Figure 2). This may be associated with abdominal
discomfort and extra flatus (wind). Many individuals, including most adults, and some
racial groups in particular, are lactase deficient. It almost amounts to physiological
lactase deficiency of adults. Most of them can and do tolerate some lactose as milk in the
diet.
Health workers are more conscious about lactose intolerance because of the small
proportion of diarrhoea cases where this deficiency causes problems. Also some artificial
milks contain extra added lactose and this puts stress on the sugar splitting enzyme
system. Some baby food companies are promoting lactose-free or low-lactose milk
substitutes as the answer to the question "what nourishment should I give my child
who has diarrhoea?"
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 37 June 1989  6
Page 7 8 6
Page 7 8
|
Figure 1: Normal digestion and absorption of lactose. |
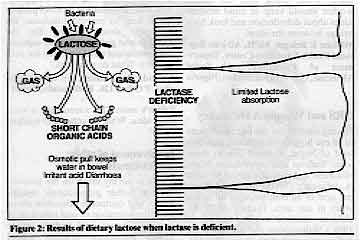 |
Figure 2: Results of dietary lactose when
lactase is deficient.
|
How do you know if a baby really has lactose intolerance?
- Test the stool with a blue litmus paper which turns pink at about , pH5.5-pH6. Dip
the paper in the liquid stool and look for the colour change. The most likely cause of an
acid stool is lactose intolerance. This is a screening test rather than definite proof of
diagnosis.
- Test for reducing sugars in the stool. Use a "Benedict-test" system.
"Clinitest" is the most widely available and convenient form. Five drops of a
freshly collected liquid stool are diluted with 10 drops of water in the little test tube.
A "Clinitest" tablet is added and the mixture will heat up and froth. Check the
colour of the fluid against the chart provided. An orange-brown colour indicates >0.5
per cent of reducing substances. This is very suggestive of carbohydrate
malabsorption.
- Milk withdrawal and challenge. The two tests described above check for the presence
of lactose intolerance, but do not reveal whether it is clinically important. Many infants
with acute infectious diarrhoea have temporary lactose intolerance that is nor clinically
important. They do not require any change in diet even when the above tests are positive.
The clinical importance of lactose intolerance can best be determined by checking whether
diarrhoea rapidly worsens when milk is given, and rapidly improves when milk is
temporarily replaced by a cooked cereal or other lactose-free food. Dietary changes to
reduce the amount of lactose are only needed when lactose intolerance is clinically
important.
Managing clinically important lactose intolerance in infants
Remember that in most cases in infants the intolerance is only partial and temporary.
Once the cause is remedied, the infection has settled or the malnutrition recovered, the
new cells will make lactase again. The steps described below should be taken in sequence. Try each for two or three days.
If diarrhoea has not improved, move to the next step.
- Dilute cows' milk or formula milk to half strength. Make up the milk in the usual
way and then add an equal volume of clean drinking water. This will dilute any lactose
along with other components of milk. Give extra cereal pulse mixtures to make up the
nourishment requirements. This is not appropriate in the first four months of life (see="#Acute">letter from Dr Natarajan). (Note - pulses are leguminous vegetables,
peas, beans, dhal, gram, etc.)
- Replace milk with milk products which are modified in traditional ways, e. g. as
curds or yoghurt, and therefore have a reduced lactose content.
- Withdraw milk completely for a few days. Breastmilk should only be withdrawn as a
last resort. Ask the mother to express her milk to keep up production as her baby will
need it again in a few days time. Give cereal pulse mixtures as suggested above, or use a
soy-based milk substitute for infants below four months of age.
Note Lactase-like enzymes can be recovered from a variety of vegetable
and animal materials, e. g. yeast. However, the pure forms, suitable for converting the
lactose of milk for food, are very expensive so this is not a realistic alternative to
soya milks. (See question in letter from Dr Suvarna Devi).
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 37 June 1989  7
Page 8 7
Page 8
Students as communicators
During a recent epidemic of diarrhoea in our state the Indian Medical Association
obtained a donation of two tons of glucose, plastic packing material and printed
instructions. We organised college, high school and technical school students throughout
the state to prepare more than 800,000 small packets of ORS using a simplified formula
with glucose and sodium chloride. The students then distributed the packets house to
house, providing the product and a message on how local fluids could also be used to
prevent the dangerous dehydrating effects of diarrhoea. The project grew and was
undertaken in all major cities and rural areas of Sadvichar Parivar, a state of more than
30 million. Lions, Rotary, Jaycees and women's groups joined in as well. Students were
highly effective communicators, often mixing the solution and drinking it in public to
create confidence. Widespread community acceptance was evident and we are proud that while
many other states clamoured for cholera vaccine, our communities were effectively educated
to the use and effectiveness of ORS in diarrhoea. Dr P Mehta, Honorary Secretary, IMA College of General Practitioners, Gujarat, India
Combining beliefs
Much health communication misses its mark because health workers unquestioningly
translate health messages from English, French or other languages directly into the local
language. While the words themselves may translate, the ideas behind them often get lost,
because local cultural disease perceptions do not always relate to modern scientific
ideas. The solution is not to revert totally to local explanations of the disease process,
but to find some common ground between different medical and cultural ideas. This process
can best be achieved during discussions between the health worker and small community
groups. This example of the Yoruba people in south west Nigeria illustrates the point. Oka
ori is the Yoruba name for sunken fontanelle. It is thought to be a disease in its own
right. The Yoruba are not unique in this belief, as it has been documented in other parts
of Africa and in Latin America. The disease is not associated with diarrhoea but is
thought to be caused by certain foods eaten by the mother during pregnancy. The health
implications of this local belief are that moderate to severe levels of dehydration may
not receive timely life-saving attention. To tackle the problem, the health worker can begin discussion by asking questions about
recognition, cause, treatment, and prevention of oka ori, listening and
noting local ideas on each issue. While doing this, the health worker should keep in mind
modern ideas about dehydration and look for a bridge between the ideas. William R Brieger, MPH, African Regional Health Education Centre, Department of
Preventive and Social Medicine, University of Ibadan, Nigeria
ORS and Vitamin A Deficiency Having worked for the last three years in an eye hospital in the south east flatland of
Nepal, I would like to share some findings and experiences. Night blindness and clinical
signs of Vitamin A deficiency (VAD) are found in six per cent of all children aged up to
ten years in our area. (Survey of 70,000 children checked at their homes in 1988.)
Malnutrition and diarrhoea are the main contributing causes of VAD. In the hospital, forms
are also filled out about the history of illnesses and food habits of VAD children. Ninety per cent of the children with corneal lesions had had diarrhoea recently, or
were still suffering from diarrhoea. Most of them were seen by a doctor before they came
to us, because of illness and diarrhoea. Most were given ORS but nutritious foods like
bananas, yoghurt, papaya (traditional foods to give in diarrhoea) were forbidden - only
some rice was allowed. Nearly all the children had already developed eye problems (at
least night blindness), but were not given vitamin A capsules, although antibiotic eye
drops were sometimes given by the doctor. Parents gave their children ORS and some rice
while diarrhoea continued for one to two weeks. The eye conditions became worse, the
children did not open their eyes, and then they came to the eye clinic. ORS is saving children's lives, but not their sight, in our area. ORS is advertised in
Nepal as a medicine: 'medicine water' or 'salt-sugar water', so many people think that
other food or treatment is not needed . . . I think that in countries where VAD is still a
big problem, brief information on ORS packets could help to prevent blindness, for
example, about looking for eye changes and giving vitamin A capsules and nutritional
advice specific for each country. What do you think? Cordula Ran, Lahan, c/o United Mission, P 0 Box 126, Kathmandu, Nepal
Editor's note: This sounds like a very good idea. What do other DD readers
think?
Involvement of other professionals
I wish to air my views on the involvement of other professionals besides nurses and
doctors in education about and administration of oral rehydration therapy. These could
include public health inspectors, primary school teachers and voluntary social
organisations. The rate at which knowledge of ORT is spreading within our community is not
encouraging, hence the need for programmes to give a role to non-health personnel. Oyebo Olunyong, Primary Health Care Centre,
Ikire-Ibadan, Oyo
State, Nigeria
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 37 June 1989
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
|