|
| |
Issue no. 38 - September 1989
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 38 -
September 1989
|
DDOnline Dialogue
on Diarrhoea Online Issue 38 September
1989  Page 1 2
Page 1 2
Tell, show and do
 |
Everyone, especially mothers, needs to know about ORT - clear
demonstrations and practical experience are the best ways to learn. |
There is now more than ten years of world experience in promoting oral rehydration
therapy (ORT). Although more children every year now receive ORT, over four million of
them still die each year from acute diarrhoea. These four million deaths could mostly be
prevented by the universal use of ORT. It seems, therefore, that just telling people about
the simplicity of ORT, and the beneficial impact this cheap, effective solution can have
on child survival, is really not enough. Making ORS widely available is also not enough. Packets must be actually used and used
correctly. We now know that short term intensive ORT campaigns can only produce lasting
effects on diarrhoea treatment when they are part of a wider move towards sustained social
change. Also, we know that ORT training programmes for health workers must include genuine
hands-on practice in diarrhoea case management - and also in effective teaching methods -
if they are to promote positive changes in behaviour. It seems that belief in the value of ORT, and confidence in being able to manage
diarrhoea at family and community levels using ORS packets, or home based solutions, can
only come through effective, appropriate education and communication at all levels of any
society. The following pages offer practical advice about various aspects of training and
teaching. It is clear that the best way to convince anyone about ORT, from highly trained
physicians to underprivileged mothers, is both to tell and show them how ORT works, and
for them to do it themselves! KME and WAMC
|
In this issue:
- A Diarrhoea Training Unit
- Practical advice: How to teach
- Breastfeeding promotion
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 38 September
1989  1 Page 2 3 1 Page 2 3
A training idea
Dehydration
Ignorance of causes
Associated infections and malnutrition
Religious taboos and misbeliefs
Recognition of how infection spreads
Hygiene
Oral fluids as early as possible
Environmental sanitation
Always give food regularly
This formula was sent to us by Dr (Mrs.) Radha Y Aras of Bombay, India, who uses it
when training community health workers to help them remember key aspects of the causes and
control of diarrhoeal disease. We would like to hear from other readers about other ideas
they have used. ORS in the UK In March 1989, a detailed description of oral rehydration therapy was included for the
first time in the British National Formulary. The entry describes the benefits of ORT and
lists the WHO formula for ORS and seven proprietary preparations available in the UK. To readers in India
Readers of DD (English edition) in India who would like to be included on the
mailing list should send requests to the Christian Medical Association of India (CMAI),
Plot 2, A-3 Local Shopping Centre, Janakpuri, New Delhi 110058, India. CMAI is now
printing and distributing DD in India on a quarterly basis. Light on ORT...
| This matchbox
is produced by the Ministry of Women's affairs in Cameroon. Thanks to Dr A Froment,
ORSTOM, Yaounde, Cameroon for letting us know about this method of information support for
the national CDD campaign. |
 |
Viewpoint - local laboratory skills
Diarrhoeal diseases caused by different organisms can have similar signs and symptoms.
With most diarrhoeas, it is not necessary to know the cause, and oral rehydration therapy
should be given for prevention and immediate treatment of dehydration caused by diarrhoea.
However, it can sometimes be useful to discover the cause of the diarrhoea - especially if
the spread of the disease is to be prevented. The quickest way to find out about the type
of germs causing diarrhoea is to use simple, low technology laboratory techniques. But
this is only possible if trained staff are available as part of a local primary health
care team. Laboratory workers examining stool samples from patients with diarrhoea need
considerable skills and knowledge. In Zimbabwe, a scheme has been developed to ensure that
trained laboratory workers spend two years working in rural health programmes. In The
Sudan, a different approach has been used: training local microscopists to carry out one
or two simple laboratory techniques using basic equipment. These two approaches have
proved very successful and could be models for other places where there is a shortage of
skilled personnel. In Zimbabwe, to attract skilled laboratory workers to rural health centres and local
hospitals where the need for highly skilled laboratory diagnosis and interpretation is
often greatest, the Ministry of Health asks qualified technologists to work in rural areas
for two years as 'payment' for their training. By means of this bond commitment, resources
used in training are paid back to the community and more remote areas benefit from the
services of the technologist. In the Gezira region of Sudan, with assistance from the University of Gezira, a
training programme has been set up for microscopists whose sole task is to examine blood
film for malaria parasites and urine and faeces for Schistosome eggs. No other laboratory
work is undertaken. This means that the equipment is kept very simple and an academic
background is not needed. Every village in the scheme has a trained microscopist who works at home - often in
very basic conditions. All that is required is a table for the microscope, staining
solutions and jars. The work is mainly done out of doors, using daylight for illumination.
Villagers are tested for parasites on a routine basis, quality control being provided by
the organisers, to maintain high standards. Microscopists are paid with millet, cooking
oil, salt and other food. Training takes three weeks with periodic refresher courses
lasting one to two days. Extension of this idea would not be too difficult as long as the
field of activity is kept fairly specific, Advantages include ease of training and little
chance of the microscopist being attracted to work elsewhere. For differential diagnosis of diarrhoea, either of these approaches could accomplish a
great deal towards improving health in rural areas. Peter J Humphries, Principal Scientific Officer, Division of Pathology, Royal Free
Hospital, Pond Street, London NW3 2QG, UK. Laboratory investigation of diarrhoeal diseases Readers whose work involves laboratory diagnosis are invited to write in for a 12 page Health
Basics booklet: Laboratory investigation of diarrhoeal diseases in primary health
care, written by Monica Cheesbrough and produced by DD. The booklet describes
the equipment, training and techniques needed to identify causes of diarrhoea at PHC
level, including the investigation of chronic diarrhoea in AIDS. Containing illustrations,
and a resource list giving sources of information and equipment, the booklet is available,
free of charge, from AHRTAG, 1 London Bridge Street, London SE1 9SG, UK.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 38 September
1989  2 Page 3 4 2 Page 3 4
Training methods
These studies from India and Bangladesh are about training mothers to mix and give
oral rehydration solution. The results of the first study show that, as a teaching method,
demonstration is more effective than description. In the second study, it was found that
mothers can be taught to use ORT as successfully in small groups as on a one-to-one basis. 1. Telling or showing?
Measuring the correct amount of fluid to mix up oral rehydration solution can be
difficult. Many studies have found a wide variation in the composition of OR solutions.
Three methods of teaching rural, non-literate women to mix ORS were tried in the Punjab,
India. The success of each method was measured by analysing the solutions the women had
made after training. Group I was told simply, in the local language, how to mix a packet of ORS by a
community health worker. A doctor was also present to answer questions. Group II was given
the same verbal instructions as Group I, but was also shown how to mix ORS. Group III was
given OR salts in a larger bag with a line printed on it, marking the level to which it
should be filled with water. The community health worker also explained and demonstrated
this method of making ORS to the group. All the women - about 20 in each group - left the training session with either a sachet
or a bag of oral rehydration salts, as had been discussed or used in their group. A few
hours later, every woman was visited at home by the health worker and doctor, who watched
her make up the ORS as she had learnt. A sample of each solution was taken, to be analysed
for sugar and salts. There was no significant difference in the age, income or education of the women
between the three groups. The solutions made by women in Groups I and III contained
concentrations which differed significantly from the ideal ORS concentrations. This
difference was far less marked in Group Il. The conclusion of the study is that the women
in Group II made oral rehydration solution most accurately. Measuring problems In Group I, given only verbal instruction, five of the women did not use the whole
packet of salts. This was because they thought making oral rehydration solution was like
making a cup of tea: they added two or three spoonfuls of ORS to a cup of water in the
same way that they would add this amount of sugar to a cup of tea. Mothers also found it
hard to measure a quantity of water exactly (half a litre in this case). Those using milk
measures were more successful than those using tumblers or cups; those using jugs or other
larger vessels were least successful. It was expected that the plastic bags used by Group III would reduce measuring problems
because they are designed to hold exactly the right amount of water. However, the
concentration of the solutions made by Group III was less accurate than that of those made
by Group Il. This is possibly because of the poor design of the plastic bags: they are
intended to be held from above in one particular position, which is difficult even with
the help of another person to pour in the water. When 20 doctors were asked to measure
half a litre (500ml) of water using the same bags, after verbal instructions and a
demonstration, the actual volumes measured by them varied from 300ml to 700ml, with a mean
of 420ml. The authors conclude that demonstrating measuring and mixing ORS is more effective than
verbal instruction alone. Finding a method for measuring ORS accurately is important,
because too little salt means that the solution may be ineffective, and too much may be
dangerous. This study is reported in full by Nagarajan, L, et al., 1989: A comparative study of
different methods of teaching rural subjects for reconstitution of oral rehydration
solutions. Indian Pediatrics 26 (April): 323-329. Reprints are available from Professor B
N S Walia, Department of Paediatrics, PGIMER, Chandigarh 160012, India. 2. Teaching in groups or one to one? The Bangladesh Rural Advancement Committee (BRAC) is a large non-government
organisation with much experience of promoting ORT in communities. Health workers have
taught mothers, using a one-to-one approach, to make home sugar-salt solution (SSS). The
cost of the programme was recently found to be 72 US cents per household visited. If this
amount could be reduced, more money would be available to meet other needs. BRAC carried
out a study to see if costs could be reduced, without affecting the programme quality, by
teaching mothers in groups rather than individually. The study compared the costs and
resulting OR solutions when mothers were taught one at a time and in small groups. In one area, mothers from different households were taught in groups of five by a
health worker. They were taught 'seven points to remember' about making and giving ORT,
the standardised technique used by BRAC. After the teaching session, each mother was asked
to demonstrate making the SSS, to make sure that she had understood. The same training was
given individually to other mothers in a similar area. One year later, an interviewer from
BRAC returned to see how much the mothers had remembered, and to find out if they used
SSS. A random five per cent of the 2,500 households interviewed were asked to prepare SSS,
and samples were taken for analysis. There was no significant difference in either the
composition of the solutions, the levels of knowledge or the use of SSS between the
mothers who had been taught alone, and those taught in a group. The cost of teaching mothers in groups of five was found to be approximately half as
much per mother as teaching individually. This study showed that by working with groups of
mothers, the same results could be obtained for half the cost. Further details of this study are published by Chowdhury, A M R et al., 1988:
Teaching ORT to women: individually or in groups? J. Trop. Hygiene 91: 283-287.
Correspondence to: A Mushtaque R Chowdhury, BRAC, 66 Mohakhali Commercial Area,
Dhaka-1212, Bangladesh.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 38 September
1989  3 Page 4 5 3 Page 4 5
Diarrhoea Training Unit
A Diarrhoea Training Unit (DTU) is a unit in a hospital which routinely treats many
cases of acute childhood diarrhoea and conducts training in correct diarrhoea case
management. In a large hospital, the DTU may be permanent; in other hospitals, it may be
set up or expanded as the need occurs, particularly when diarrhoea is seasonal. What does a DTU do?
A DTU develops the skill and confidence of doctors and other health workers so they can
give proper treatment for diarrhoea. They learn skills in diarrhoea management, especially
use of ORT, through hands-on experience, and in teaching others. A DTU can be established
where staff are interested in training others; where many patients are treated for acute
diarrhoea and dehydration, so that participants are trained by actually treating patients.
Five essential elements of a DTU are listed below. 1. Proper therapy for diarrhoea is practised on a routine
basis.
- Mothers stay with their children to give ORT and continue breastfeeding
- Mothers are taught how to give ORT, continue ORT at home, feed during and after
diarrhoea, and recognise the signs indicating that a child should be brought back to a
health worker. They are given other relevant health education messages on prevention of
diarrhoea
- ORT is used appropriately; intravenous therapy is not used when ORT would be effective
- Antibiotics are used only as needed; anti-diarrhoeal drugs are never used
2. Doctors, nurses and other staff members should use the same
diarrhoea treatment methods.
3. Space is arranged so that there are three areas for management of
diarrhoea cases.
- In the reception area, new cases are assessed, and classified for treatment.
Also, mothers are taught about diarrhoea prevention and home management.
- In the ORT area, ORS is made up, and staff supervise while
relatives give ORS to patients with diarrhoea.
- In the diarrhoea ward, patients with severe dehydration or complications are
treated separately, and may initially receive fluids through a drip or a nasogastric tube.
4. At night, continued care is provided for in-patients and new
emergency cases.
5. Appropriate supplies are available in adequate quantities
(see="#Supplies">box below) Training objectives
At the Diarrhoea Training Unit, case management skills should be developed with
supervision, so that the procedures outlined below are followed. In the reception area 1. Diarrhoea cases are assessed to:
- determine the extent of dehydration
- identify other problems (e. g. dysentery, fever, severe malnutrition), complications
(e.g. paralytic ileus), or associated diseases (e. g. measles)
- identify other diseases (e. g. meningitis) that may require treatment elsewhere.
2. Decide which cases need to be sent to the ORT area or
diarrhoea ward.
3. Teach each mother management of diarrhoea at home (fluids, food and
signs that indicate a child should be brought to a health worker), and educate her about
prevention of diarrhoea.
Note: If it is the policy to give ORS packets to mothers, trainees should
demonstrate and teach mothers how to mix and give ORS.
4. Prescribe other medicines if needed.
In the ORT area 1. Assess and treat cases:
- take the history, examine the patient and determine the amount of fluid to be given over
a four to six hour period
- discuss findings and recommendations for treatment with staff
- begin administering ORS and teach the mother to give the ORS
- assess the patient's progress periodically and record findings (every hour until the
patient is rehydrated; every two hours thereafter)
- decide on the amount of ORS to be given for maintenance and advise the mother
- treat other problems (e. g. reduce fever, give an antibiotic for dysentery)
2. Mix oral rehydration solution in bulk volumes.
3. Deal with difficulties in giving ORS (such as vomiting).
4. Supervise mothers and nurses giving ORS.
5. Encourage the mother to continue feeding the child giving a
diet appropriate for the child's age and prior feeding status.
6. Before a mother leaves, teach her how to continue caring for
her child at home and the signs that indicate she should bring her child back. Also,
explain what she can do to prevent diarrhoea, as well as how she can treat it. In the diarrhoea ward 1. Assess patients with severe dehydration:
- take history, read any hospital chart or notes, and examine the patient
- determine amount of fluid required
- if there will be a delay in putting in the IV, and if the patient can drink, begin ORS
while waiting for IV to be started
- discuss findings and recommendations for treatment with staff
2. Treat as appropriate:
- give intravenous therapy, if possible, otherwise insert nasogastric tube and administer
oral solution
- care for other problems, complications and associated diseases
3. Assess the patient's progress periodically and record
findings (every one to two hours until the patient is rehydrated; every six hours
thereafter). Start giving some ORS as soon as the patient can drink; discontinue the IV
when the initial deficit is corrected and signs of severe dehydration are gone. 4. Before the child is discharged from the diarrhoea ward, be
sure that the mother is taught how to continue caring for her child at home and the signs
that indicate she should bring her child back. Tell the mother that if her child starts
passing many watery stools, has frequent vomiting, becomes very thirsty, does not eat and
drink normally, develops blood in the stools, or seems not to be getting better, she
should bring him or her back. Also explain what she can do to prevent and treat diarrhoea. This article is based on material from Diarrhoea Training Unit: Director's Guide
1988, produced by the CDD Programme, World Health Organization, 1211 Geneva 27,
Switzerland.
|
Supplies for a Diarrhoea Training
Unit Reception area
- Health education materials including pamphlets, and posters on preparation of OR
solution, home fluids, diarrhoea prevention, and management including feeding during and
after diarrhoea
- Forms for record keeping
- ORS packets of the standard size in the area (for demonstrating to mothers)
- Jars and flasks (commonly available sizes and one marked with volume measurements)
- Glasses, cups and spoons
ORT area
- ORS packets for making up large quantities of solution, and of a standard size in the
area (for demonstrating to mothers)
- Jars and flasks (as above)
- Antibiotics (tetracycline capsules) if cholera is likely in the area, and a suitable
antibiotic for dysentery
- Health education materials (as above)
- Baby scales accurate to 20 grams
- Thermometers
- Glasses, cups and spoons
- Cotton, gauze, towels and other linens
- Forms for record keeping
- Droppers
- Soap, wash basin and towel rack
- Nappies
Diarrhoea ward
- Beds or tables with wires above for hanging bottles of IV fluid
- Lactated Ringer's Solution with giving sets
- Scalp vein (butterfly) needles
- Antibiotics (as above)
- Glucose for injection (20%)
- Baby scales (accurate to 20 grams)
- Nasogastric tubes
- Thermometer
- Droppers
- Feeding bottles, milk powder
- Soap, towels and other linens
- Forms for record keeping
- Seating for nurses and relatives
- Health education materials for families
- Syringes and needles
- Alcohol, cotton, gauze
- Glasses, cups and spoons
- One litre and half litre flasks
- Nappies
- Tray or trolley for supplies
- Waste basket or bucket
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 38 September
1989  4 Page 5 6 4 Page 5 6
Step-by-step planning How can training be effective in preparing health workers to carry out key CDD tasks?
The effectiveness of training depends upon how well it is planned, the training methods
used, and whether or not there is refresher training, as well as follow up visits to
personnel in the field. It takes time to plan good training, and planning should be done
one step at a time. The steps described here can be used in planning any type of health
personnel training. Step 1: Define CDD tasks The success of training will be measured by how well health workers carry out CDD tasks
when they return to their posts. Define carefully the tasks expected of them based on an
understanding of existing practices and behaviour, so that they are taught about which
practices need to be changed, reinforced, or introduced. An example of a task would be to
educate mothers about home management of diarrhoea. Step 2: Identify knowledge, attitudes and skills needed
This step is often missed out, and the content of health training programmes is limited
to technical knowledge of the particular health topic. To teach mothers about diarrhoea,
knowing the clinical signs of diarrhoea and dehydration is necessary, but certain
attitudes and skills are also needed. For example, the health worker must be able to: find
out what mothers usually do at home to treat diarrhoea; know how to mix and give ORS; and
know how to ask questions in the right way. Step 3: Choose priority topics
You will now have a list of tasks, and of what is needed to carry them out. There will
never be enough time to teach everything, so decide on priorities. To do this, it can be
helpful to categorise the skills which are 'essential', 'useful', or 'interesting'.
'Essential' items can then be grouped in topics, for example: advising on home treatment;
mixing and giving ORS. Step 4: Define objectives Once priority topics are identified, define the specific objectives for each training
session. Trainers and trainees need to know what is to be learned, and it is important to
limit the content of the training session. Define objectives in terms of what trainees
should be able to do by the end of the training session. Step 5: Prepare a draft training plan and schedule
Using topics (Step 3) and the objectives for each topic (Step 4), prepare a draft training plan and schedule. Order the topics
and estimate the time necessary for each one. It is important to do this before planning
sessions in detail. Step 6: Choose appropriate learning activities
Trainees learn more through active participation than just watching or listening. Make
sure that learning activities are as similar as possible to the tasks which will be
expected of the trainees in their own work environment. For example, practice in mixing
ORS will be more effective than talking about it. Think about which learning activities
would be best for achieving different objectives. A knowledge objective could be dealt
with using a lecture, a text, a film plus discussion, or several of these activities
combined. Activities where trainees are personally involved - group discussions, role
plays and practical experience - would be more effective in getting participants to think
about their present attitudes and to consider adopting new ones. For skill objectives,
practical experience: for example, preparing and giving ORS to a dehydrated child;
conducting a group CDD education session with mothers, would be most effective. Step 7: Develop a detailed plan
A 'planning worksheet' can be useful in deciding how each learning activity in each
session will be carried out, what material and human resources will be needed, who will be
responsible for what, and the time for each activity. Step 8: Finalise the training plan Finally, review and, if necessary, adjust the training plan and schedule based on what
is decided in Steps 6 and 7. Judi Aubel, Consultant in Health Education and Training, B P 3746, Dakar, Senegal;
and Dr Mohamad Mansour, CDD Project Director, 8 Rue Immam Sahnoun, Tunis, Tunisia.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 38 September
1989  5 Page 6 7 5 Page 6 7
The right start
Encouraging breastfeeding instead of bottle-feeding can help to prevent diarrhoea.
CDD programmes can promote breastfeeding by training health professionals and improving
hospital practices. Medical education about diarrhoea management should stress the role of breastfeeding,
both in preventing diarrhoea, and as a component in ORT and feeding during and after
diarrhoea. A recent Guatemalan survey found that more than 50 per cent of doctors did not
know that breastmilk helps protect infants against diarrhoea, or that it can be an
important food source after the first six months of life. Teaching health workers about the advantages of breastfeeding, and how to help mothers
breastfeed, has been productive in Indonesia, Thailand, Panama, the USA, and elsewhere.
Although many programmes have emphasised the benefits of breastfeeding, they have not been
aware of the need to include techniques to help mothers to breastfeed - an equally, if not
more, important part of training. It is important: to encourage proper positioning of the
infant at the breast; to help the mother in cases where the infant does not want to suck
or sucks with difficulty; to advise on how to prevent engorgement, infection, and other
breastfeeding problems. Changing hospital practices
Changing the ways hospitals manage childbirth can also encourage mothers to breastfeed.
Appropriate practices include keeping the mother and baby together, and suckling soon
after delivery. Mothers who have immediate contact with their infants after birth are more
likely to continue breastfeeding. This also ensures that the baby receives the first milk
- colostrum - which gives important protection against infection. Analgesics (painkillers) and anaesthesia should be used as little as possible during
delivery, as these drugs are passed on to the baby making it too sleepy to suck after the
birth. No water, glucose water, or other supplements to the infant's diet should be
introduced in hospital. Infants who are given bottles often show subsequent 'nipple
confusion', because sucking at the breast requires different movements from sucking at a
bottle nipple, and can be more difficult. Demand feeding promotes increased milk
production, because infants fed on demand will usually suckle about every two hours during
their first few weeks, and regular sucking helps increase milk production.
Rooming-in
|
To encourage early and continued breastfeeding, it is
important for a mother and baby to be together often. It is important to allow the mother and baby to stay together continuously while in
hospital. Known as 'rooming-in', this provides the conditions needed for successful
breastfeeding, encouraging demand feeding, no bottles, and no replacement of breastmilk by
water or other supplements. Health professionals can promote breastfeeding by encouraging
mothers to feed infants frequently, by not allowing bottles on the wards, by restricting
the distribution of milk samples or bottles in the hospital, and by changing the ward
arrangements to make rooming-in a standard practice.
|
 |
Routines in ORT units CDD workers often have to deal with cases of diarrhoea associated with lack of
breastfeeding, but then it is often too late to re-establish breastfeeding. By promoting
exclusive breastfeeding during the first months of life, health workers can help to
discourage early supplementation and use of bottles. In ORT units, bottles should not be used, and spoon feeding of ORS should be the
approved method of the hospital, so that mothers will not think that bottles are endorsed
by the medical community. Health workers can also use this opportunity to encourage
mothers to continue breastfeeding at home, and to use spoons rather than bottles for
giving ORS. Hospital ORT units and in-patient intravenous units should be arranged to
ensure that breastfeeding mothers are not separated from their infants. It is essential that CDD workers see breastfeeding as an important aspect of diarrhoea
prevention and try to influence policy and practice at all levels in their day-to-day
work. Many hospitals have ORT units and in-patient wards where diarrhoea is a major cause
of admission. These units are often a highly respected part of the paediatric service and
doctors managing diarrhoea are often also responsible for conducting paediatric rounds.
They have access to the administrators who make policy, and work alongside obstetricians,
who may need to be convinced about rooming-in. In all these situations, paediatricians can
influence hospital policies for the better, and can encourage practices which promote
breastfeeding. Sandy Huffman, President, Center to Prevent Childhood Malnutrition, Suite 104, 720O
Wisconsin Avenue, Bethesda, MD 20814, USA A five page bibliography, including references for the studies mentioned in this
article, is available free of charge, on request, from DD.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 38 September
1989  6 Page 7 8 6 Page 7 8
How to teach
Health workers may need to train others in primary health care, including
diarrhoeal disease control. But, often, they themselves have no training in how to teach. DD
presents practical guidelines for those involved in training. If you are training others, it is not enough to know how to do something - you need to
know how to pass on that knowledge. Whether you are helping a community to build latrines
or leading a training course, it is always important to ask a few key questions:
- Do you know enough about the needs of the trainees, and how will you find out about
these needs?
- What is the aim of this training - what should be learnt from it?
- Have you allowed enough time to cover everything you planned?
- Have you planned how to check that your training is effective?
Two-way communication
If you are teaching members of the community, rather than health workers you need to be
extra sure that your teaching is appropriate. Is this training needed and wanted? For
example, if you have been asked to teach mothers about ORT, you should learn to understand
their needs. To do this:
- Ask what they want to know, and why
- Find out what they think about diarrhoea and its causes, and learn about local words and
customs
- Find out how much they know already about prevention and treatment
- See how much time they can spare for learning
- Try to adapt your training to local knowledge and customs
- Decide how much you can cover in the time available (do not attempt too much)
Do not just tell mothers only what you think they should know. Listen to them, and let
them know that you are listening. Only when you do this, can you provide teaching that is
useful and likely to be acted upon. Teaching methods
It is always difficult to learn anything just by hearing about it. Traditional teaching
methods often rely too much on talking. When practical skills are being taught, it is
especially important to show something being done, and to let people learn by doing.
Trainees should be encouraged to take an active part in discussions, rather than sitting
back passively. New skills and information are always more memorable when they are
'discovered', rather than heard about. Below are some examples of techniques you could use
to get people more involved.
- Group discussions are valuable in finding out about existing knowledge and
attitudes, and useful to help everyone to get to know each other. They provide a chance
for participants to learn from each other as well as from the teacher, and to ask
questions relatively informally, without fear of losing face or being embarrassed.
- Practical work is essential if the people being trained are expected to learn
practical skills. Interviewing, taking histories, and good communication of all sorts are
all skills which require practice as much as skills like making oral rehydration solution,
using weighing scales, and sterilising equipment.
- Problem solving is a useful way of making training more interesting and easy to
remember. It is also more likely to be the way in which health workers will have to carry
out their work after training. For example, rather than listing a set of procedures for
dealing with breastfeeding problems, you could present different problems one at a time,
and ask people how they would try and solve them.
- Role playing can help trainees to see a situation from another person's point of
view. You could divide a group into pairs, with one person acting the part of a mother
with a sick child, and the other a health worker.
- Games can be useful learning aids, but you need to be sure that people do not
feel embarrassed about taking part, and that they are really learning and not only
thinking about the game itself. You could use the toss of a coin to determine imaginary
events, or use picture cards to make up families and events.
- Case studies are useful for introducing the complicated combinations of events
which occur in real life. Some training needs to be simplified so that treating diarrhoea,
for example, can be learnt one step at a time. But case studies can link an episode of
diarrhoea with other factors such as malnutrition, poor sanitation and lack of awareness
about hygiene.
- Field visits, for example to a health centre or practising diarrhoea management
unit, allow trainees to see more than you can demonstrate to them with fewer resources.
They can also be important when teaching about referral, and what referral centres can
offer. You could also arrange visits to mothers at home, women's groups, schools,
pharmacists and experts on different subjects related to the training.
- Visual aids are very important to convey key messages clearly, but they must
always be easy to understand and culturally appropriate, otherwise they can cause
confusion. Suitable posters, diagrams, graphs, and pictures should all be used as much as
possible.
Evaluation
An important part of training is checking what people are learning. If some things are
not being absorbed, you need to adjust your teaching speed or style, or possibly accept
that some things are outside the scope of what you can teach in the time available. You
can evaluate your training simply by testing trainees' knowledge of a subject you have
worked on together, or by observing them at work. Further reading Werner, D, and Bower. B, 1982. Helping health workers learn: a book of methods, aids
and ideas for instructors at the village level, Hesperian Foundation: USA. World Health Organisation, 1987 The Community health worker: working guide,
guidelines for training, guidelines for adaptation. WHO: Switzerland.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 38 September
1989  7 Page 8 7 Page 8
What is weaning?
In="dd32.htm">issue 32 of Dialogue on Diarrhoea, the information on
weaning was welcome and informative. However, it may have caused some confusion regarding
the definition of 'weaning'. The article describes weaning as "giving of family foods
in addition to breastmilk" and "a gradual process by which the infant becomes
accustomed to the adult diet". According to Dorland's Medical Dictionary, weaning
means "taking off the breast", that is, not supplementation, but the replacement
of breastfeeding. Could you clarify this point and state exactly when the infant should be
taken off the breast? Dr M A Muttalib, President, Community Health Research Association, 22 Bijoynagar,
Dhaka, Bangladesh.
Dr Andrew Tomkins, London School of Hygiene and Tropical Medicine, replies There is often a lack of clarity about the use of the word 'weaning', even in most
dictionaries. I myself use 'weaning on' to mean the start of weaning - the introduction of
solid foods in addition to (i. e. supplementing) breastmilk, and 'weaning off' to mean
completion of weaning - stopping breastfeeding completely. Breastfeeding can be continued
for two years or more, but other food is needed as well as breastmilk when the baby
reaches four to six months of age.
Food hygiene and infection Following Dr Schweiger's article on food hygiene in DD36,
I would like to add some points of my own. These are some ways in which individuals can
reduce the risk of catching diarrhoea from dirty food:
- Refuse to buy any food which is ready cooked and cooled, or is to be eaten raw, that is
not wrapped or protected from flies
- Never carry unwrapped food in your hands, and never carry jugs of milk or other fluids
with your fingers or thumbs inside the jug
- Keep food preparation surroundings clean, and never leave dirty plates and pots or
scraps of food where they might attract flies to contaminate other food
- Report to the authorities any shop where food is handled in dirty and unhygienic
conditions.
Akinyemi A Taiwo, Secretariat, PMB 5005, Ibadan, Oyo State, Nigeria.
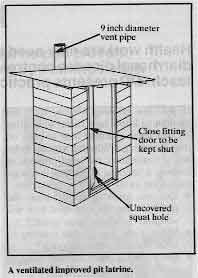
Latrine confusion In the March issue (number 36) of DD, the picture of a latrine in the="su36.htm">Practical Hygiene insert shows some confusion between
the ordinary type of pit latrine and the ventilated improved pit (VIP) latrine. The
picture shows a VIP latrine, but with the opening covered, and a large space over the
door. The opening of the ordinary type must be kept covered when not in use, and plenty of
light allowed in over the walls and through the open door.
|
A ventilated improved pit latrine.
But the VIP latrine needs to be kept relatively dark inside so that the ventilation
pipe (of nine inches diameter) is the main source of light, and so that this light is
brighter than that entering through the latrine hole. Any flies which may breed in the pit
are then attracted to the ventilation pipe, but die and fall back when they cannot get out
through the fly screen in the vent pipe. Also, with the VIP latrine door shut, warm air is
drawn up and out of the vent pipe, removing smells. VIP latrines are popular because they
are relatively free of flies and smells, compared with ordinary pit latrines. It is
therefore important to distinguish clearly between the two types.
|
 |
Dr C A Pearson, 2 Springfield Road, Bury St Edmunds, Suffolk, UK.
Improving latrines Our Community Health Unit has started a campaign to stop faecal borne diseases in our
area. As part of this campaign, every household built a pit latrine with a pit of six to
seven feet deep. However, many of the latrines smelt so bad that people were unwilling to
use them. After discussion with the villagers, it was decided to add ventilation pipes
made from bamboo (which is a cheap local material). So far, only a few families have made
this improvement, but they have found that smells have been considerably reduced. We hope
to take these ideas to other villages in the area. Mr Dawa Tshering, Health Assistant, Lingmethang BHU, BPO Kurizampa, Mongar, Eastern
Bhutan, Bhutan.
Editors' note: To obtain the full benefits of VIP latrines, other factors as
well as ventilation pipes require attention: see Dr Pearson's letter above.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 38 September 1989
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
|