|
| |
Issue no. 45 - June 1991
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
updated: 23 April, 2014
Pages 1-8 Dialogue on Diarrhoea Online Issue 45 - June
1991
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 45 June 1991
 Page 1 2
Page 1 2
Diarrhoea and dire circumstances
Epidemics of diarrhoea are a still a major problem. People living in refugee camps, who
have been recently displaced by war or natural disasters, are especially at risk, because
they do not initially have access to clean water supplies and good sanitation. Diarrhoeal
diseases, such as cholera, can spread rapidly among adults and children in refugee camps.
Those who live in over-crowded shanty towns, where environmental conditions are poor, are
also vulnerable. As the Dialogue goes to press, reports highlight the risk of diarrhoeal
diseases in Iraq, in areas where sanitation infrastructure has been destroyed. This year,
for the first time this century, cholera has broken out in Latin America. The epidemic is
spreading rapidly, affecting several countries and large numbers of people. Cholera need not kill Correct use of oral rehydration therapy (ORT) and appropriate drugs will save most
lives. Fewer than one per cent of over 200,000 reported cholera cases in Peru have died,
because prompt action has been taken (1). After the first case was identified,
health authorities made sure that medical staff throughout the country knew how to treat
cholera, and hospitals were issued with special supplies of ORS, intravenous fluids and
antibiotics. Public health education is ensuring that people know how to recognise cholera
and help prevent its spread.
|
Epidemics of diarrhoeal diseases, such as cholera, can spread
rapidly where environmental conditions are poor, especially in shanty towns or refugee
camps.
This issue of the Dialogue describes public health measures to control cholera,
and reports on how cholera deaths were dramatically reduced in a rural area of Bangladesh
and a refugee camp in Malawi. A special supplement features
practical guidelines on preventing diarrhoea epidemics in newly established refugee camps.
|
 |
Finally, most people know that diarrhoea germs can be passed from one person to
another, or through contaminated water. Fewer know that it is possible to catch an
infection that causes diarrhoea from animals. Find out more on="#page4">page 4.
1. Lores H, and Burbano J, 1991. Cholera situation in the Americas. Epidemiological
Bulletin, PAHO. Vol 12, no.1.
|
In this issue:
- Cholera - prevention and control
- Refugees and displaced communities
- Drugs - when and what to prescribe
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue no. 45 June 1991
 1 Page 2 3 1 Page 2 3
Epidemic control
DD describes public health measures which help to prevent the spread of
cholera. The current cholera epidemic is caused by the El Tor vibrio organism, which was first
seen in 1961 in Asia. The pandemic spread to the Middle East and reached Africa in 1970.
Nearly 100 countries have been affected. Traders and travellers can carry the infection
without knowing, and large gatherings of people increase the chance for infection to
spread. Cholera epidemics have also occurred in many refugee camps in recent years
(Ethiopia in 1984-85, Sudan in 1985, Somalia in 1985 and Malawi in 1986-88). The cholera epidemic that began early this year in Peru is now very serious. It has
reached the capital, Lima, where more than half the city's population of seven million
live in shanty towns. The epidemic has already spread to other Latin American countries.
In Africa, Zambian authorities had, by March, reported 6,000 cases, in an epidemic that
also threatens neighbouring Tanzania. Being prepared During an epidemic, most cholera episodes are mild and many people can carry the
organism but show no symptoms. Severe cholera is characterised by frequent watery stools
and vomiting. Fluid losses are high, and dehydration can develop rapidly, resulting in
death within three to four hours of the symptoms first appearing. Patients may also be
weakened by having to travel long distances to health facilities, and these facilities are
often unable to cope with the sudden increase in numbers of people needing care. In an
unprepared community, severe cholera can be associated with death rates of 50 per cent or
more. However, cholera is treatable. In most cases ORT and an appropriate antibiotic are
sufficient. Even in severe cases, correct treatment can reduce death rates to less than
one per cent of those infected. Cholera can also be prevented, but this requires
improvements in water supply, sanitation and hygiene.
|
Temporary treatment centres reduce pressure on health
facilities during an epidemic.
National diarrhoeal disease control programmes, if properly organised and managed, can
reduce the spread of infection by ensuring that the health system is well prepared to
quickly detect and control an epidemic. This includes monitoring patterns of illness, and
training health workers to cope with an increased caseload and to manage cases correctly.
|
 |
Increased publicity about the value of correct case management, including ORT, during a
cholera epidemic could, in the long term, improve acceptance of similar treatment for
those with diarrhoea due to other causes. Control measures
If an epidemic occurs, local authorities should emphasise the following preventive
measures:
- provide/maintain safe and adequate community facilities for excreta disposal;
- supply clean drinking water, if possible, if the existing supply is contaminated;
- prevent the use of contaminated drinking sources or washing/bathing areas;
- provide suitable chemicals for, and information about, household water purification;
- discourage the gathering of large crowds, for example, at feasts or funerals;
- ensure immediate and hygienic disposal of dead bodies.
They should also take measures to ensure effective treatment of cases:
- establish emergency treatment centres, assure a supply of essential materials for
treatment of patients, and retrain medical personnel if necessary;
- identify and treat patients early, isolate them from others as far as possible, and
promptly disinfect their surroundings (e. g. bedding, drinking vessels).
Public education Health workers need to inform the community about how to avoid infection. Families will
be worried and looking for help and advice: individual home visits, posters, public
meetings and radio and TV announcements may all be appropriate. Community and religious
leaders can also help to mobilise people to take part in epidemic control activities. These are the most important points to emphasise:
- With correct and prompt treatment, cholera is not fatal.
- Most cases can be treated with simple measures, especially ORT.
- Dispose of human excreta safely.
- Good personal hygiene habits help prevent transmission of cholera.
- Safe preparation of food and cleaning of utensils reduce risk of infections.
- Use clean water for drinking and bathing.
What not to do when cholera breaks out:
- Vaccination is not recommended. This is because the vaccine gives only modest
protection, which disappears after several months. Two injections are required, separated
by at least two weeks.
- Mass chemoprophylaxis (preventive dosing with antibiotics) is not helpful, since it is
usually impossible to treat everybody quickly enough to prevent the infection spreading.
Occasionally it is appropriate to dose close contacts of cholera cases (see="#page3">case study 1).
- Travel restrictions are not effective in preventing the spread of infection. This is
because many people are symptomless carriers of the cholera organism, but are still able
to infect others. It is not possible to control the movements of such apparently healthy
persons.
- Trade restrictions are not effective. There is no evidence that restricting exports from
areas where cholera is occurring will prevent it spreading to unaffected areas nearby.
Ref: WHO guidelines for the control of epidemics due to cholera (1991). WHO's
information kit on cholera provides more information on how to organise activities during
an outbreak, and how to identify and treat cholera patients. Available from the CDR
Programme, WHO, 1211 Geneva 27, Switzerland.
Common sources of cholera infection
- water contaminated at its source (e. g. by faeces leaking into an incompletely sealed
well) or during storage (e. g. by contact with faecally contaminated hands)
- contaminated foods which are eaten raw or undercooked, or stored at a temperature at
which bacteria can rapidly multiply to infectious levels
- raw vegetables that have been washed with contaminated water
|
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 45 June 1991
 2 Page 3 4 2 Page 3 4
Case study 1: Cholera control in a refugee camp
Factors that led to the rapid spread of cholera in a Mozambican refugee camp in Malawi
were identified by a research study. The study monitored cholera incidence, identified
high-risk groups, and led to precise recommendations that helped to bring the epidemic
under control. Through following these recommendations, the cholera incidence rate was
kept to below three cases per 1,000, despite the extremely poor general health of the
refugees. Between 15 March and 17 May 1988, 784 cases of cholera were registered at the cholera
treatment centre which had been set up in the camp. A case-control study of the fist 50
cases brought to the centre, showed that those with cholera were more likely to have used
water from one of the shallow wells in the camp than the healthy individuals in the
control group. Rains had destroyed half the camp's latrines two weeks before the epidemic broke out.
Most of these latrines were three to four metres deep and in contact with the water table
(the water level beneath the ground), which was at most only four metres below the
surface. This water was contaminated by latrine contents during the rains, and caused
surface well water to become unsafe. Nearly half of the shallow wells in the camp tested
for faecal coliform bacteria showed positive signs of faecal contamination, whereas none
of the deep borehole wells did. After the study, camp authorities advised the refugees to use only the boreholes as far
as possible. Families were also supplied with chemicals to chlorinate their drinking
water. Limiting transmission
The market was also temporarily closed, since the study found that those with cholera
were more likely to have eaten food recently bought there. The twice monthly food
distribution, normally held in one central area, took place instead at a number of
different parts of the camp, to discourage the gathering at one site of thousands of
refugees from both outside and within the camp. The cholera treatment centre kept records of where cholera patients lived in the camp,
so that areas of high risk could be identified. Health workers found new cases through
home visits, so that oral rehydration treatment could be given early in the illness.
Preventive doses (prophylaxis) of tetracycline (250mg tablets four times a day for three
days) were given to family contacts of cases. Supervised by health workers, the bodies of
those who had died were disinfected with chloride of lime, and put into sealed plastic
bags for burial. Moren, A, et al. 1991. Practical field epidemiology to investigate a cholera
outbreak in a Mozambican refugee camp in Malawi. J. Trop. Med. Hyg., 94:1-7.
|
How to recognise and treat cholera Health workers should look out for the first signs:
- an increase in the daily number of patients with diarrhoea and vomiting, especially
those with 'rice water stools';
- watery diarrhoea causing severe dehydration in any patient aged ten years or more.
Case management:
- give ORS solution to the patient by mouth. The amounts below show approximately
how much ORS solution to give during the first four hours of treatment:
under 4 months |
200ml to 400ml |
| 4-11 months |
400ml to 600ml |
| 1-4 years |
600ml to 1200ml |
| 5-14 years |
1200ml to 2200ml |
| over 14 years |
2200ml to 4000ml |
give Ringer's Lactate Solution intravenously if severely dehydrated;
feed the patient three or four hours after ORT has been started, and
when rehydration is completed, continue to encourage him or her to eat and drink - infants
should continue to breastfeed;
- treat severe cases with an appropriate oral antibiotic, such as tetracycline, when
vomiting has stopped (usually within a few hours of beginning ORT). Adult dosage: 500mg
tetracycline 4 times per day for 3 days or 300mg doxycycline in a single dose.
Where there is local resistance to tetracycline, give 100mg furazolidone 4 times per day
for 3 days, or 160mg TMP and 800mg SMX twice a day for 3 days. (See="#page7">page 7 for child dosages.)
|
Case study 2: An emergency treatment centre saves lives
Temporary treatment centres help to ease the pressure on health facilities during an
epidemic. One such centre was set up during a cholera outbreak in a rural village in
Bangladesh in 1986, because the nearest permanent health centre was three hours away by
boat. Local community leaders made a primary school shed available as a temporary centre,
which was kept open for three weeks, catering for over 200 patients. One doctor, with three assistants, provided medical care; relatives of patients and
unqualified local practitioners provided day-to-day care and food. Drugs and treatment
supplies included only ORS, intravenous saline bags and tetracycline capsules. A
government health inspector monitored the epidemic, by organising household surveys and
obtaining detailed histories from patients at the centre. After the centre was set up, the numbers of reported cases and of patients receiving
medical attention trebled. The proportion of deaths dropped substantially, from 14 per
cent to 0.4 per cent, with only one death out of the 263 reported cases. Most patients
were able to reach the centre before their condition became life-threatening, and prompt
and effective rehydration treatment saved many lives. Before the centre opened only one
case out of 94 had managed to get to the permanent health centre, and all 13 fatal cases
had died at home. The success of ORT in saving lives at this centre should help to
persuade local health workers and the community of the value of ORT in diarrhoea
management. Siddique, A K, et al. 1990. Makeshift treatment centre during a cholera epidemic in
Bangladesh. Tropical Doctor, 20: 83-85. Correspondence to Epidemic Control Preparedness
Programme (ECPP), ICDDR, B, P O Box 128, Dhaka 1000. Bangladesh.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 45 June 1991
 3 Page 4 5 3 Page 4 5
A danger to human health?
Most health workers are aware of person-to-person transmission of diarrhoeal
disease. The fact that animals can transmit diarrhoea germs to people is less well known. DD
reviews the evidence. Micro-organisms that cause diarrhoea are found in many domestic animals and birds,
which live with people as food sources or pets. These include cattle, goats, pigs, dogs,
cats and chickens. Wild animals, such as rats, that live in the same environment as
people, also act as hosts for these organisms. There are two ways in which these micro-organisms can be transmitted to people. Animal
products, such as chicken meat, eggs or milk, can be contaminated with bacteria. People
consuming these products risk diarrhoeal infections. This article focuses on the second
route of transmission of infection, which takes place via animal faeces. Many species of bacteria, viruses and protozoa have been found in the intestines of
healthy animals. These include common causes of diarrhoea such as Campylobacter, E.
coli, Salmonella, rotavirus, cryptosporidium, E. histolytica and
giardia. The species, age and health of animals determines the extent to which they act as
organism hosts. A study in Haryana state, India showed that on average only 10 per cent of
a mixed group of sick and healthy buffalo and cattle tested positive for Campylobacter
(1). Young animals, and those with diarrhoea, were more likely to have Campylobacter
in their stools than healthy adult animals. In contrast, 50 per cent of all the pigs
tested had Campylobacter in their stools, including the healthy ones. Ten per cent
of children tested in the same area also had the bacterium in their stools. In developing countries, diarrhoeal diseases mostly affect young children, and those
who live in rural areas usually have more infection from animals than urban dwellers. Contaminated environment
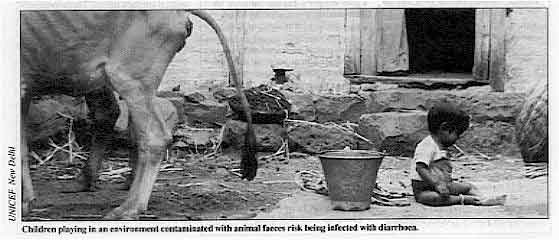 |
Children playing in an environment contaminated with animal faeces risk
being infected with diarrhoea. Transmission from domestic animals is probably an important source of
infection. It usually occurs through contamination of the household environment by animal
faeces. In addition, food and drink can transmit infection to humans when they have become
contaminated by animal faeces.
|
Diarrhoea-causing organisms are transmitted to humans from animals very easily through
the faecal-oral route. An infectious dose of Campylobacter, for example, can be as
low as one hundred organisms. Animal faeces can come into contact with and contaminate
children's playthings, cooking utensils, bedding, and garden soil or yard dirt. Children
playing in, and touching things in an environment contaminated with animal faeces will get
traces of faecal matter on their fingers and hands, which they often put into their
mouths. They are also likely to contaminate other objects with their hands. Any health education programme aiming to reduce diarrhoeal disease in a community
should consider the possibility that animals may be a source of infection. The following are suggestions for reducing the health risks of living with animals:
- maintain good animal health; isolate sick animals, treat them appropriately (see="#page5">article on page 5 on ORT for animals with diarrhoea) and keep children
away from them, if possible;
- keep animals away from drinking water sources used by people;
- keep stray animals out of the household area;
- sweep up and either bury animal droppings, or put them in a latrine, or place them on a
dung heap that is inaccessible to children;
- keep children's play areas separate from where animals are kept;
- keep smaller animals such as chickens off surfaces where food is prepared, and out of
kitchens and eating areas as far as possible;
- do not allow animals to eat off the same dishes as people;
- make sure that children wash their hands, preferably with soap, before eating or
touching food, especially if they have been playing with or near animals.
1. Kakkar et al, 1990. Prevalence of campylobacter infections in animals and
children in Haryana, India. J. Diar. Dis. Res. 8:34-36.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 45 June 1991
 4 Page 5 6 4 Page 5 6
Chickens and childhood diarrhoea
Diarrhoea is a major health problem for young children in Peru. Contact between
toddlers and domestic chickens may be a cause of infection. DD reports. A study in Lima's shanty towns looked at the factors which might explain the patterns
of transmission and infection with the bacterium Campylobacter jejuni. Earlier
research had shown that:
- chickens often carry C. jejuni in their gut;
- C. jejuni causes much of the dysentery seen in infants in Lima;
- C. jejuni can survive for up to 48 hours in chicken
faeces: 40
per cent of samples from infected chickens contained active C. jejuni after
24 hours in the sun, and after 48 hours 18 per cent were still positive;
- children in families where household chickens were infected with C. jejuni were
12 times more likely to have diarrhoea than those in homes without chickens.
Children's habits Field workers visited ten homes with children under five years of age (a total of 21
children). They observed the behaviour of these children and of chickens for 12 hours in
each home and saw that:
- each child touched chicken faeces with his or her hands about three times;
- each child put fingers contaminated with faeces in his or her mouth about four times;
- contaminated hands were rarely washed before the child sucked his or her fingers;
- the likelihood that a child's fingers would be contaminated increased with the number of
chicken stools deposited in the home during the day.
Mothers knew the risks, but ...
As part of the study, 108 mothers were asked about their poultry rearing practices and
beliefs. Most (71 per cent) were aware that it cost less to buy a chicken in the market
than to raise one at home, but they continued to keep chickens for reasons of enjoyment.
|
In Peru's shanty towns, chickens roam freely despite the health risk.
Nearly half of the mothers who kept chickens knew that free-roaming poultry are a
health or hygiene risk. Nevertheless, in 83 percent of families, the chickens were allowed
to roam freely and had access to the house. This was possibly because of the commonly held
belief that chickens grow better if allowed to wander freely.
|
 |
These findings show that even when people know about the health risks of certain
practices, other factors may decide their behaviour. Behavioural and cultural studies like
this can help us to understand better how diarrhoeal diseases are transmitted. Health
education workers need to know what is happening in the home, otherwise their efforts to
improve hygiene may be inappropriate and ineffective. Marquis, G S et al, 1990. Faecal contamination of shanty town toddlers in
households with non-corralled poultry, Lima, Peru. Am. J. Public Health 80:146-149. This study was supported by the Applied Diarrhoeal Disease Research Project of
Harvard Institute for International Development, 1 Eliot Street, Cambridge, MA 02138, USA.
ORT for animals
Diarrhoea often affects young domestic animals, such as calves and piglets. But
ORT can be given to animals as well as to people. The idea of ORT for animals is not as strange as it first sounds. Diarrhoea in animals
is caused by bacteria and viruses similar to those that affect humans. Animals with
diarrhoea suffer the effects of dehydration and loss of salts in much the same way as
people. Dehydration from diarrhoea is the main cause of death in young animals, with death
rates of 20 to 30 per cent or more. A loss of six to ten per cent of body weight produces
clinical signs like those seen in humans. The loss of livestock through diarrhoeal disease can be a great economic problem for
farmers. It can be prevented by keeping young animals in clean, uncrowded surroundings,
feeding them with colostrum, weaning them gradually, and avoiding stressing them during
transportation. Before ORT was discovered, the only treatments available were intravenous rehydration
and antibiotics. Studies during the past twenty years show that ORT can reduce mortality
in animals to two per cent or less, and that antibiotics are ineffective. Pig
co-operatives in Haiti are now using ORT, which is important because the North American
breeds introduced in the 1980s are particularly susceptible to diarrhoea. Animals will
drink ORS eagerly from an open container, or from feeding bottles. Very weak animals need
a stomach tube. The composition of fluids used is similar to the WHO formula. Animal immunisation programmes have helped to improve community acceptance of vaccines
for young children. This suggests that ORT promotion for animal use might encourage people
to give ORT to their children. It would be useful, however, to have more first-hand
accounts about ORT for animals. Perhaps health workers could try to give ORS to animals
with diarrhoea - if you have already done this, please share your experience with other
readers! Dr Norbert Hirschhorn, c/o The Ford Foundation, PO Box 2030, Jakarta 1001,
Indonesia. Ref: Gastrointestinal diseases in the young pig and calf. 1983, Ann. Vet. Res.
(whole issue) 14: no 4.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 45 June 1991
 5 Page 6 7 5 Page 6 7
What changes behaviour?
Richard Laing reviews the effectiveness of different
methods used to change prescribing practice. Over-prescription of drugs is a major problem in patients with diarrhoea. Various
strategies have been used to try to improve prescribing practices. The results have often
been disappointing. This article looks at the methods used, and which seem to work best. Methods available Approaches to changing practice can be grouped into four categories.
- Educational -This is the most common approach, but can be the least effective. It
usually takes place during basic undergraduate training or through in-service activities.
The most successful educational methods are 'face-to-face', such as small group teaching,
one-to-one training, or advice giving at the time of dispensing. Printed educational
materials are most effective when combined with other interventions. General media, for
example national or local newspapers, radio or television, are useful for quickly
spreading new information.
- Regulatory -These are related to government policy or laws. These include banning
particular drugs; limiting the number of drugs available to lower level health facilities;
preventing repeat prescriptions; or limiting the number of drugs which a doctor can
prescribe. Unfortunately, these actions can have unexpected, negative results. For
example, if an ineffective but harmless anti-diarrhoeal drug is banned, doctors may
prescribe another more dangerous drug in its place, rather than giving only ORS.
- Managerial -These are related to health system administration. These include
limiting drug availability by changing the national drug list; restricting the prescribing
of certain drugs to doctors with special training; altering prescribing and dispensing
patterns by encouraging the use of standard prescription forms, and diagnostic and
treatment guidelines; printing clear instructions on drug container labels; and regularly
monitoring prescribing practices.
- Financial - These are related, for example, to reducing the profit margin on
non-effective drugs, or making essential drugs less expensive.
Which methods work best?
Apart from one study in Yemen (1), there has been very little evaluation of efforts to
improve prescribing practices in developing countries, and therefore not much is known
about what does and does not work. In the Yemen study two different areas were compared,
one with a functioning essential drugs programme, and one without. Compared with the
non-programme area, the number of essential drugs available was greater in the programme
area, and the number of non-essential drugs was reduced.
 |
Small group teaching is one of the educational methods that has
successfully changed prescribing practice. Prescribers attended workshops about rational drug use in the programme area and
learned how to use standard treatment schedules. They also went to follow-up training
sessions.
|
Although knowledge of rational drug use showed only slight improvement, those who had
been trained referred to the new treatment schedules on a regular basis. Overall the
programme was successful: fewer antibiotics, fewer injections and fewer drugs were
prescribed. Studies of various methods in developed countries have shown that the most effective
are also the most expensive and time consuming. These include:
- face-to-face education that focuses on specific problems;
- using structured drug order forms (particularly in institutions);
- regular checking of prescriptions, with feedback to the prescribers.
Methods having some success include:
- involving health professionals themselves in developing appropriate drug lists; and
- holding training sessions on the use of standard treatment schedules.
The least effective methods are often those that are carried out first and include:
- using printed educational materials alone;
- establishing essential drug lists or standard treatment schedules with no educational
back-up;
- setting arbitrary limits on prescribing;
- providing unfocused education (such as general lectures on pharmacology).
Prescribing patterns
Knowing what doctors are prescribing helps to decide which intervention methods to use.
Finding this out is not difficult, but requires careful planning. Many surveys try to
collect too much information from too few sites. An adequate sample could be as few as 30
randomly selected prescriptions, from each of at least 20 sites, giving a total of 600.
The indicators used to assess prescribing practices can also be very simple. The ones
proposed by INRUD (International Network for the Rational Use of Drugs) include:
- the average number of drugs per prescription;
- the average number of injections per prescription;
- the average number of antibiotics per prescription;
- the percentage of children under five with diarrhoea receiving ORS; and
- the percentage of children under five with diarrhoea receiving anti-diarrhoeal
preparations.
Patient care can be assessed by measuring: average consultation time; average
dispensing time; and presence of a minimum physical examination (pulse, temperature and
skin pinch). Choose the methods for the intervention strategy on the basis of what has been learned
about prescribing patterns. What works best will vary from one country to another and will
probably be a combination of the methods listed above. Richard Laing, INRUD, c/o Management Sciences for Health, 165 Allandale Rd, Boston,
MA 02130, USA. 1, Hogerzeil, H V, et al. 1989. Impact of an essential drugs programme on
availability and rational use of drugs. Lancet, January 21 pp 141-3. For more information please contact INRUD at the above address.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 45 June 1991
 6 Page 7 8 6 Page 7 8
Antibiotics and diarrhoea
DD explains how drugs can be used appropriately for treating cholera and
acute dysentery. There are two kinds of diarrhoea for which antibiotics should be given. Dysentery (acute diarrhoea with blood in the stool) can have a variety of
causes. The most frequent and most important is Shigella. A patient with acute
dysentery should be treated immediately with an effective antibiotic. If the illness is
caused by Shigella, this will result in a marked improvement within two days: less
fever, fewer stools, less blood in the stools, and improved appetite. If there is no
improvement, it usually means Shigella are resistant to the antibiotic
given. Another antibiotic should be given instead. Suspected cholera requires an antibiotic effective against Vibrio cholerae, especially
if there is severe dehydration. (This is in addition to treatment to replace lost water
and electrolytes.) Antibiotic treatment reduces the amount of diarrhoeal stool passed, and
usually stops the illness within 48 hours. Cholera should be suspected in any patient who
develops acute watery diarrhoea, usually with vomiting, in an area where there is an
outbreak of cholera; or when a patient aged over ten years of age develops severe
dehydration from acute watery diarrhoea.
- Tetracycline
Tetracycline is the drug of choice for cholera. It rapidly kills Vibrio cholerae and
therefore reduces the duration of the disease and the amount of rehydration treatment
needed.
Pharmacology and how it works
Tetracycline is a broad spectrum antibiotic that kills or slows the multiplication of
bacteria. Doxycycline is a slowly excreted form of tetracycline that is effective as a
single dose (for adults only).
Adverse effects and precautions for use
Tetracycline is not recommended for children under 12 years, as it is deposited in
newly forming teeth and bones, causing discoloration. But, given the dangers of severe
cholera, a short course of tetracycline is justifiable. Avoid giving tetracycline if there
is significant damage to the kidneys or liver.
- Cotrimoxazole
Also called trimethoprim (TMP) - sulphamethoxazole (SMX), these two drugs are combined in
a ratio of 1:5 TMP-SMX, because they work together more effectively than alone. It is the
drug of first choice for bacterial dysentery in most parts of the world. It is also used
for cholera, in regions where the Vibrio is resistant to tetracycline, or in young
children.
Pharmacology and how they work
Antimicrobial resistance to sulphonamides is a growing problem. However, when given
together, the two drugs may slow down resistance development. The drugs are absorbed into
the bloodstream, reaching bacteria that have invaded the tissues.
Adverse effects and precautions for use
TMP and SMX share some side effects. They slow down the rate at which cells divide and
are therefore not recommended during pregnancy, nor for premature or jaundiced infants
under one month old. Excretion is through the kidneys, so poor kidney function is a
contra-indication for use. Sulphonamides can cause abdominal upsets, including a feeling
of sickness or vomiting. Serious effects include damage to the bone marrow and bad rashes,
like Stevens-Johnson syndrome.
- Ampicillin
Ampicillin is a broad spectrum penicillin, active against a wide range of bacteria. It is
recommended for dysentery, where Shigella are sensitive. However, in many areas most
Shigella have developed resistance.
Pharmacology and how it works
Like other penicillins, it acts by interfering with the construction of bacterial cell
walls.
Adverse effects and precautions for use
When given by mouth, only about half of ampicillin is absorbed. Absorption is further
decreased if it is taken with food. It should be given between or before meals.
Ampicillin often causes rashes, particularly when a patient has certain viral infections,
including HIV infection and glandular fever. It should not be given if the patient is
allergic to penicillin. Normal gut bacteria may be affected, causing bowel upsets.
- Nalidixic acid
This is one of the 4-quinolone group of antibiotics. Where Shigella organisms are
resistant to cotrimoxazole and ampicillin, this is usually the drug of choice for
dysentery.
Pharmacology and how it works
Nalidixic acid is easily absorbed from the bowel and blocks bacterial multiplication.
Another powerful antibiotic in this group is ciprofloxacin, but it is expensive and
recommended only for infections that are resistant to all other drugs.
Adverse effects and precautions for use
Nalidixic acid can cause bowel upsets and skin sensitivity to sunlight. It may produce
nervous system disturbances, headaches, giddiness and visual upsets. Avoid use in patients
who have a history of convulsions.
- Furazolidone
Furazolidone has both anti-bacterial and some anti-protozoal action. Although slower
acting than some antibiotics, relatively few bacteria have developed resistance to it. It
is useful when cholera is known or suspected to be resistant to tetracycline.
Pharmacology
and how it works
Furazolidone is poorly soluble when taken by mouth. It acts mostly on organisms within the
bowel, interfering with their enzyme systems.
Adverse effects and precautions for use
Side affects include bowel upsets, rashes, allergic reactions and sometimes giddiness,
drowsiness and headache. Avoid use with drugs that act on the autonomic nervous system
such as ephedrine.
|
Antibiotic dosages for children by mg/kg body weight
- Cholera:
tetracycline 12.5 mg/kg 4 times a day for 3 days
or (if local resistance)
furazolidone 1.25 mg/kg 4 times a day for 3 days
or TMP 5 mg/kg and SMX 25 mg/kg twice a day for 3 days
- Shigella dysentery:
TMP 5 mg/kg and SMX 25 mg/kg twice a day for 5
days
or (if local resistance)
nalidixic acid 15 mg/kg 4 times a day for 5 days
or ampicillin 25 mg/kg 4 times a day for 5 days
|
Dr William Cutting, University of Edinburgh, UK. Correction: controlled trials have shown that furazolidone is not effective
in treating acute dysentery (as suggested in="su44.htm#page3">DD44 supplement
page 3). For references, contact DD.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 45 June 1991
 7 Page 8 7 Page 8
Diarrhoea management - Britain lags behind
A recent study in Britain to find out what pharmacists recommend for diarrhoea and how
much mothers know about correct management, showed that neither group was always sure
about the best treatment for childhood diarrhoea. Diarrhoea is one of the most common
illnesses in children for which advice is sought from a pharmacist. It is therefore
important that pharmacists give the right advice. Twenty randomly-chosen community pharmacists in a large city were asked to fill in
questionnaires about what treatment they would recommend for diarrhoea. Researchers posing
as parents visited half the sample, asking for advice about treating a child with
diarrhoea. All the pharmacists advised some form of purchased treatment, whether ORS or an
anti-diarrhoeal drug (both available without a doctor's prescription). But half the
pharmacists responding to the questionnaire, and 70 per cent of those visited, recommended
inappropriate treatment such as anti-diarrhoeal drugs (e. g. kaolin or
loperamide).
Although 50 per cent recognised the importance of ORS in their questionnaire answers, less
than one third actually recommended it to the researchers who posed as parents. Only 30
per cent of pharmacists in the group visited asked the child's age. None asked about
duration of illness or for further details, including about symptoms of dehydration. Mothers attending child health clinics in the city were also asked about diarrhoea
management. Only 15 per cent said they would use ORS (described using a well known brand
name) if their child had diarrhoea, although the majority had heard about it. A few (seven
per cent) said that they would give their child over-the-counter drugs, such as kaolin and
morphine, or loperamide. Nearly half the mothers said they would stop breastfeeding or
giving food to their child if he or she had diarrhoea. Although the numbers interviewed were small, the results suggest a high level of
ignorance among British pharmacists and mothers about the treatment of childhood
diarrhoea. Most of the pharmacists, however, felt that they should be giving advice on
diarrhoea treatment, and said that they wanted more training. In addition to recommending improvements in training courses for pharmacists, the study
suggests that guidelines issued to them should match those used by WHO. Information should
include advice on home preparation of ORS and warnings about the use of anti-diarrhoeal
drugs. Goodburn, E et al. 1991. Management of childhood diarrhoea by pharmacists and
parents: is Britain lagging behind the Third World? Brit. Med. J. Vol 302: 440-443. ORT is useful for treating adults I am a regular reader of DD and find it very informative. Although I support the
emphasis put on the usefulness of ORT in treating diarrhoea in children, I would like to
remind readers that ORT is also very useful in managing diarrhoea in adults. I have been running a hospital-based AIDS clinic for the past four years, and am also
involved in caring for HIV infected patients who are members of The AIDS Support
Organisation (TASO) in Uganda. Many of my patients suffer from both acute and chronic
diarrhoea as a result of their HIV infection and I rely on ORT as an essential part of
their treatment. It took me a long time to convince the patients and their relatives that ORT would be
effective in treating their diarrhoea. Sometimes doctors themselves are very reluctant to
use ORT. New patients often need to be encouraged to take ORS fluid. However, with
persuasion, they realise how helpful the treatment is, and start asking for it regularly.
I have heard the patients give these reasons for refusal:
- it is a treatment for children, and not appropriate for adults;
- it does not taste nice;
- it makes me vomit, or feel like vomiting, whenever I take it.
I try to help patients by explaining that:
- ORT replaces both water and minerals which are lost during the bouts of diarrhoea and/or
vomiting, and provides energy so that the patient will feel stronger;
- when the patient is vomiting or feeling nauseous, ORS should be taken in small amounts
but more frequently;
- ORS should be taken as soon as diarrhoea or vomiting begins, since this prevents the
development of dehydration, which can lead to further complications.
|
ORT benefits adults - including those with HIV related
diarrhoea.
We now routinely give ORS to all our patients with HIV associated diarrhoea. They often
improve without any treatment with antibiotics. We have also noted a big reduction in the
number of patients developing severe dehydration and requiring admission to hospital.
|
 |
Dr E Katabira, Department of Medicine, Mulago Hospital, P 0 Box 8933, Kampala,
Uganda.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Assistant editor Nel Druce
Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Nicole Guérin (France)
Dr Norbert Hirschhorn (USA)
Dr Sharon Huttly (UK)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 45 June 1991
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
updated: 23 April, 2014
|