|
| |
Issue no. 12 - February 1983
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Diarrhoea Dialogue Online Issue 12 -
February 1983
|
DDOnline
Diarrhoea Dialogue Online Issue 12 February
1983  Page 1 2
Page 1 2
Cholera tamed by ORT
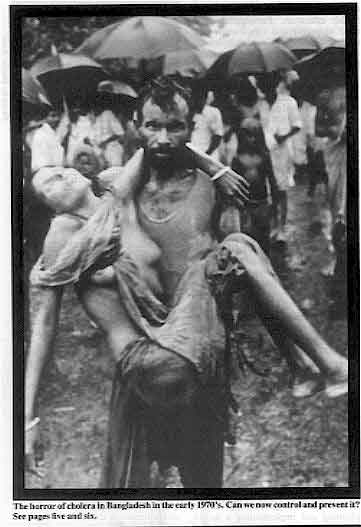 |
The
horror of cholera in Bangladesh in the early 1970's. Can we now control and prevent it?
See pages="#page5">five and six. This issue marks the 100th anniversary of the identification by Robert Koch of the
organism responsible for the death of millions. A crucial part of the cholera story is the
triumph of oral rehydration therapy (ORT) which began in Calcutta and Bangladesh just over
12 years ago. "They came in, carried or supported by their relatives and lay down . . . they
voided their bowels where they lay . . . the cramps spread upwards from the calves to
tighten the thin thighs and to knot the flaccid bellies . . . they gulped thirstily and, a
minute later, would vomit up what they had drunk. They shrank as the substance was drawn
from every part of the body and pushed out in those convulsions. Noses became pointed . .
. skin wrinkled and had no resilience. When those signs came, they had neither fear of
death nor will to live." Such was cholera in 1856 as described in a novel about Bengal by John Masters.
|
No one has to die from dehydration caused by any diarrhoeal disease provided someone
knows how to give enough oral rehydration correctly. Prevention of cholera can be summed up quite simply with the saying 'You can drink
cholera and you can eat cholera, but you cannot catch it'. Food and water must be kept
safe from contamination with faeces or vomit and hands kept clean at all times. Health
education can help to eliminate the causes of diarrhoeal diseases like cholera. Meanwhile
ORT can prevent unnecessary suffering and deaths. K. M. E.
|
In this issue...
- Cholera: history, research and control
- The role of intestinal parasites in the chronic diarrhoea/malnutrition syndrome
- News and reviews
|
|
DDOnline
Diarrhoea Dialogue Online Issue 12 February
1983  1 Page 2 3 1 Page 2 3
| The children's revolution The recent announcement by James Grant,
Executive Director of UNICEF, that the organization intends to put its resources even more
firmly behind the promotion of oral rehydration therapy (ORT) and breastfeeding is welcome
news. Collaboration between UNICEF and the diarrhoeal disease control programme of WHO is,
of course, not new. The two organizations have promoted the use of ORT for several years,
with WHO focusing more on training and management and UNICEF concentrating on production
and supply of oral rehydration salts (ORS). Nevertheless, this new initiative,
particularly in the whole area of communications and diarrhoeal disease control, will
undoubtedly help to stimulate far more widespread use of ORT with far-reaching
implications for child health in developing countries. |
Cooperating on communications
A crucial aspect of communications and diarrhoeal disease control is that different
people working on programmes have the opportunity to meet and discuss the best ways of
confronting the problem together. We report below on two meetings that have taken
place recently to encourage this kind of cooperation: Dominica: health education in schools Two seminars were held recently in the Dominican Republic to look at ways of preventing
typhoid and other diarrhoeal diseases - especially in schools. The seminars were sponsored
by UNICEF, in collaboration with the Ministry of Health, and attended by principals of
schools and health educators. Typhoid is endemic in Dominica and research has shown that the disease is transmitted
mainly by food. A health education drive stressing personal hygiene, therefore, could do
much to reduce the high incidence of the disease. Participants at the seminar discussed the best way of promoting personal hygiene both
at home and in schools. Constraints such as shortage of water and the best ways of
overcoming these problems were also considered. The importance of preventing diarrhoea in children was stressed by health educators.
Participants practised preparing oral rehydration fluid using both UNICEF oral rehydration
salts (ORS) and locally available ingredients.
A final technical session looked at the importance of breast-feeding and diet in the
treatment and prevention of diarrhoea. School principals and health educators had not
discussed these issues together and all the participants found the meeting very useful.
They produced the following recommendations:
- improvement of school facilities - especially water and sanitation
- wearing of official identification badges by all approved food handlers
- use of more printed materials on health issues in schools.
Report sent to Diarrhoea Dialogue by Marese O'Dwyer, Health Education
Unit, Primary Health Care Centre, Upper Lane, Roseau, Dominican Republic. Rio de Janeiro: communications workshop A workshop on communications and diarrhoeal disease control was held from 29 November
to 10 December 1982 in Rio de Janeiro. Organized by the Pan American Health Organization
(PAHO) and the Centro Latinoamericano de Tecnologia Educational para la Salud
(NUTES/CLATES) the workshop was attended by participants from ten South American
countries. Two people came from each country and they included paediatricians, public
health staff, nurses, health educators and artists. The aim of the workshop, the first of its kind, was to suggest an approach to planning
and implementing a health education programme for diarrhoeal disease control. Work
included discussions on adapting the 'social marketing' approach to health education
(looking at analysis of target audiences, message formulation, pre-testing of materials
and selection of media etc); production of some health education materials; and the
development of guidelines to encourage participants to prepare a national workplan for a
communications programme for diarrhoeal diseases.
|
Discussing
posters produced at the workshop
The workshop was organized so that participants worked in both small groups and plenary
sessions. Many people had already been involved in health education programmes and had
much useful experience to share. Great emphasis was laid on the pre-testing and evaluation
of materials - frequently left out of health education programmes.
|
 |
Participants at the workshop will now develop programmes in their own countries,
supported by PAHO. It is hoped that they will meet again at the end of 1983 to compare
progress achieved. During the year, the representatives from each country will also keep
in touch with their counterparts elsewhere to share experiences as they develop their
programmes. The communications workshop could well be of use in other parts of the world and the
diarrhoeal disease control programme of the World Health Organization is considering
whether this might happen. Two-way radio newsletter
Ned Wallace, of Development Technologies Ltd, has told us about a newsletter his
organization is starting this spring. The new publication will contain information about
use of two-way radio for rural health care in developing countries. There will be
information on equipment and the newsletter will also offer an inquiry service. If you
would like to be put on the mailing list write to: Marshall Cook, Editor, TWR Newsletter.
4337 Felton Place, Madison. WI 53705, USA.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 12 February
1983  2 Page 3 4 2 Page 3 4
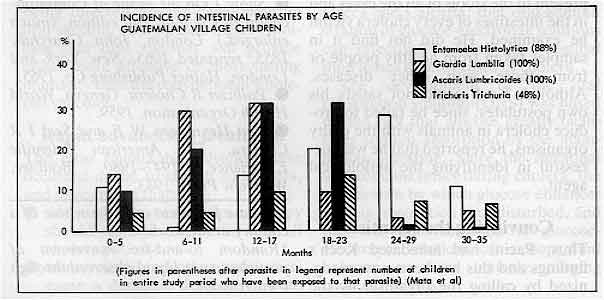
Causes or contributors?
Previous issues of Diarrhoea Dialogue have looked at the diagnosis and
treatment of some intestinal parasites. Andrew Tomkins now
considers their real significance in the chronic diarrhoea/malnutrition syndrome in
children. Many children in developing countries excrete parasites. Some are easily visible, for
example the adult worm of Roundworm (Ascaris lumbricoides) looks like an earthworm.
Others such as Giardia lamblia can only be seen by microscopic examination. Most
children in areas with inadequate sanitation experience an infection with Entamoeba,
Ascaris, Giardia or Trichuris during early childhood. Since many children also
have diarrhoea and are underweight it is tempting to blame the parasites. However, we
should ask whether they really cause disease.
Parasites can react with the intestine in several ways: Damage to the intestinal mucosa Giardia lamblia, Strongyloides stercoralis, Capillaria philippinensis and Cryptosporidium
destroy cells of the intestinal mucosa so that nutrient malabsorption occurs leading
to deficiencies of protein, energy, Vitamin A and folic acid. Mucosal damage causes
secondary lactase deficiency which makes diarrhoea worse if milk feeds, other than
breastfeeding, are continued. It seems that intestinal damage is most severe during the
first infection; the intestinal effect in subsequent infections is milder, suggesting the
development of some immunity. When immunity becomes weak, as in children with marasmus or
kwashiorkor, the parasites multiply. This is especially dangerous with Strongyloides which
actively invades the intestine. Decreased digestion Increased faecal losses of nitrogen and energy occur in children with heavy Ascaris infections
(though light infections have little effect). Giardia interferes with the process
which makes dietary fats soluble. A further problem is that bacteria colonise the upper
intestine during some intestinal infections. They may also decrease digestion of
nutrients. Loss of body fluids Many types of diarrhoea cause loss of body salts and minerals but certain parasites, Entamoeba
in particular, also cause loss of blood and proteins from the damaged intestinal
mucosa. Loss of appetite Food intake may be reduced by over 30 per cent during the prolonged diarrhoea caused by
some parasites. In severe giardiasis there is abdominal distension and discomfort due to
the malabsorption. In heavy infection with Ascaris there may be abdominal colic. Strongyloides
can cause abdominal pain and irritant skin rashes. Trichuris may cause painful
rectal prolapse. All these factors make a child miserable and unless he can be persuaded
to eat he will lose weight. Effect of treatment There are several factors to be considered: First, the nutritional status and diet. If the child is moderately well nourished and
fed, it is unlikely that treatment will be followed by weight gain. However, if he is
clinically malnourished and on an inadequate diet, the same degree of parasitic infection
is more serious and treatment can improve nutritional status. Second, the dose of infection. It is difficult to measure this accurately but, in Ascaris
infection, it is only children with heavy infection who show significant improvement
in growth after infection has been treated. Similarly, children with severe diarrhoea and
many trophozoites of Giardia show a more striking improvement in growth after
treatment than those children who are merely cyst carriers. Who should be treated?
However desirable it is to treat all infected children, mass treatment is unlikely to
be cost-effective. It is probably best to target treatment towards specific groups of
children. These would include those with clinical malnutrition or those with severe growth
faltering, those with obvious clinical symptoms of giardiasis (prolonged diarrhoea) or
amoebiasis (dysentery), any child with Strongyloides and those with especially
heavy infection with Ascaris. Unanswered questions
The introduction of oral rehydration therapy has drastically reduced mortality from
acute diarrhoea but many children are still dying from the protracted
diarrhoea/malnutrition syndrome. There are many unanswered questions about the role of
intestinal parasites in this syndrome. Perhaps you have some answers. Diarrhoea
Dialogue would be pleased to hear from you. Dr Andrew Tomkins, Senior Lecturer, Department of Human Nutrition, London School of
Hygiene and Tropical Medicine, U.K. Formerly at M.R.C. Laboratories, Fajara, The Gambia,
W. Africa. Mata L Jet al 1977 Effect of infection on food intake and the nutritional state:
perspectives as viewed from the village. American Journal of Clinical Nutrition 30:
1215-1227.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 12 February
1983  3 Page 4 5 3 Page 4 5
| Confronting a killer: 100 years of research on cholera |
The devastating disease
Abram Benenson reviews the history of cholera and those
who discovered its cause. Cholera was first reported in the Indian subcontinent in the 17th century and, as far
as we know, remained mostly in the Bengal area until 1817 when it began to spread to other
parts of the world in 'pandemics'. * The first pandemic began in 1817 and spread throughout Asia. The second began in 1829
and cholera spread into the West, entering Russia in 1830, England in 1831, and crossing
the ocean to Canada and the United States in 1832. Cholera was a new disease, causing
consternation and havoc as it spread. In some communities, as many as 15 per cent of the
population died in cholera epidemics. Many considered the disease to be a divine
infliction, correctable by appropriate devotions and proper living. Hunting the organism More scientific thought, however. was given to the problem when a second wave of
disease hit Europe. In 1849. John Snow published the famous pamphlet in which he argued
that the disease was transmitted by faecal wastes in water. During the third pandemic,
which hit England in 1853- 54, Snow was able to prove the association between drinking
faecally contaminated water and the development of cholera. He claimed the disease was
caused by 'morbid matter' which entered the body through the mouth and multiplied during
the incubation period. In 1849, Budd claimed that a distinct species of fungus, when
swallowed, would cause the disease. Pacini reported from Italy in 1854 the presence of
curved organisms in the intestinal contents of cholera victims. These organisms had a
darting motility far surpassing that of Brownian movement.** He called the organisms Vibrio
cholerae, but his publication of these findings rested quietly in the Italian
literature. Subsequently other workers observed and described such organisms but the
scientific world remained unconvinced. The fourth pandemic
The fourth pandemic started in 1863 and killed half a million people in Europe over the
next ten years. The cause of this devastating disease needed to be clearly defined.
Distinguished scientists, such as Pettenkofer, maintained that cholera was caused by
airborne emanations from suitable soils. Macnamara, a British ophthalmologist who was
convinced that a specific aetiological agent was causing cholera, was refused permission
to go to India for further studies. However, Robert Koch headed a German Commission and
Roux a French Commission which went to seek the aetiological organism in Egypt, which had
been invaded during the fifth pandemic in 1881. The French group tried to isolate the
organism by animal inoculation. Koch used the bacteriological techniques which he had
developed and succeeded in isolating a suspect organism. When the disease disappeared from Egypt, Koch went to India and demonstrated that the
suspect organism was present in the stools of all the cases and in the intestines of every
cholera victim he examined. He did not find it in samples taken from healthy people or
from those with other diseases. Although Koch could not satisfy his own postulates, since
he failed to produce cholera in animals with the guilty organisms, he reported that he was
successful in identifying the aetiological agent. Convincing the scientists
Thus, Pacini had antedated Koch's findings and this has been now recognized by calling
the organism by the name he gave it (Vibrio cholerae). Snow had identified the
faecal-oral transmission of the disease, and the important part played by
faecally-contaminated water. But Koch was the one who succeeded in convincing the
scientific world of these truths, and put to rest the conflicting and false concepts
supported by very influential scientists. It is 100 years since the issue has been settled. Since then there have been two
pandemics. The sixth lasted from 1899 to 1923, largely in Eastern Europe. The seventh, and
current, pandemic started in 1958 in Sulawesi and spread to reach Europe by 1965. It has
provided the impetus for the initiation of exciting studies by many scientists on the
pathogenesis, immunology, treatment and prevention of cholera. Out of these studies have
come the techniques for successful management of the disease, especially oral rehydration
therapy, described in previous issues of Diarrhoea Dialogue, the effectiveness of
appropriate antibiotics in eliminating infectivity, and the role which can be played by
available vaccines. These studies, largely centred in the Pakistan - SEATO Cholera
Research Laboratory (now the International Centre for Diarrhoeal Disease Research,
Bangladesh), have converted a terrible disease with a case fatality rate among
hospitalized cases of 20 per cent and higher to an easily managed illness with death
occurring in less than one per cent. Professor Abram Benenson, Head, Division of Epidemiology and Biostatistics, Graduate
School of Public Health, San Diego University, USA. Further reading:
- Snow J On the Mode of Communication of Cholera. 2nd edition, (much enlarged.) London,
John Churchill, 1855; reprinted 1965, New York and London, Hafner Publishing Co, 1965.
- Pollitzer R Cholera. Geneva, World Health Organization, 1959.
- Van Heyningen W E and Seal J R Cholera, The American Scientific Experience,
1947-1980. Boulder, Westview Press, 1983.
*Disease prevalent over the whole of a country or the world **Random to-and-fro movement of particles in any liquid observed through a
microscope.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 12 February
1983  4 Page 5 6 4 Page 5 6
| Confronting a killer: 100 years of research on cholera |
Recent developments
The treatment of cholera has progressed considerably since the first pandemic
spread out of India in 1817. Charles Carpenter highlights the
key advances. The central key to our current understanding of cholera was the 1959 demonstration, by
S. N. De in Calcutta, that the massive intestinal fluid losses in cholera are directly
related to the action of an enterotoxin, caused by cholera vibrios, on the intestinal cell
wall. Subsequent studies have:
- demonstrated that the same enterotoxin is produced by all pathogenic strains of V.
cholerae
- defined the chemical structure of the enterotoxin
- identified the molecular pathways by which the enterotoxin causes fluid secretion by the
intestine.
There is no other bacterial infection in which pathogenetic events have been so
precisely defined. Vaccine research
However, despite this, no effective vaccine has yet been developed. Carefully
controlled field trials, carried out in Bangladesh and the Philippines in 1963, clearly
demonstrated that conventional whole-cell vaccines, consisting of killed micro-organisms,
provide only limited (40 per cent to 70 per cent) protection for a relatively short period
of time (6 to 18 months). More recent studies have demonstrated that a toxoid prepared
from the cholera enterotoxin likewise provides only limited protection for a short time.
Although considerable research is now being directed toward developing an oral vaccine, no
solid data exist to indicate that oral vaccines will provide either more effective or more
lasting immunity than the conventional whole-cell vaccines. Rapid advances in treatment
The most remarkable advances have occurred in the treatment of cholera, and have shown
that:
- adequate intravenous fluid therapy should result in the survival of all cholera
patients.
- tetracycline (and other antibiotics) cause a dramatic decrease in both the duration and
volume of intestinal fluid loss and therefore in the volume of fluids required for
treatment.
- oral administration of properly prepared glucose- (or sucrose-) electrolyte solutions
will alone provide adequate treatment for the great majority of cholera patients in all
age groups.
Studies in Bangkok in the late 1950s established two important facts which were
essential to the rapid advances during the 1960s:
- the clear demonstration that the structure of the intestinal mucosal wall is not damaged
during cholera.
- the precise description of the nature of intestinal fluid losses in cholera.
Over the next few years, studies in India and Bangladesh clearly demonstrated that
virtually all patients would survive if they received adequate quantities of the proper
intravenous fluids throughout the two to five day course of cholera. Oral rehydration therapy
Only four years after the demonstration of the effectiveness of antibiotics, another
far more important and radical advance in therapy occurred, which has made it possible to
treat cholera effectively anywhere, with inexpensive, locally available ingredients. This
development was the demonstration, in Dacca and Calcutta, that oral administration of
glucose-electrolyte solutions can effectively restore the intestinal fluid losses in most
cases of cholera. The development of the oral rehydration solution (ORS) was based on the fact that
glucose greatly facilitates sodium absorption by the mammalian intestine. Since the
intestinal wall remains intact during cholera, the mechanism by which glucose enhances
sodium absorption is undisturbed, and the oral administration of glucose-electrolyte
solutions can restore fluid balance even in actively purging cholera patients. WHO: ORS solution A number of glucose-electrolyte solutions have proved to be effective, but the one
which is currently most strongly recommended is the WHO oral rehydration salts solution
(ORS), which consists simply of 3.5 grams of NaCl (table salt), 2.5 grams of NaHC03
(baking soda), 1.5 grams of potassium chloride and 20 grams of glucose (or 40 grams of the
more readily available sucrose or table sugar) per litre of water. This single solution,
when given orally in quantities equal to 1½ times the volume of intestinal fluid losses,
has proved to be effective in both the initial and maintenance treatment of virtually all
cholera patients. Occasionally patients who are already in hypovolemic shock* may still
require an initial intravenous infusion of fluids when first seen by a health worker.
However, most patients can be treated adequately with ORS throughout the course of
cholera. Subsequent studies have demonstrated that ORS is also effective in the treatment of
other acute infectious diarrhoeal illnesses, caused both by other bacterial (e. g.
enterotoxigenic E. coli) and by viruses (e. g. rotavirus). Universal treatment
Now that an effective treatment of acute diarrhoeal disease has been developed, every
effort must be directed towards:
- Ensuring that village health workers everywhere are familiar with the preparation of
ORS, or alternatives using locally available ingredients and measuring techniques.
- Educating the community, especially mothers, in developing countries about the
necessity for beginning oral rehydration as soon as diarrhoea begins and maintaining the
administration of ORS throughout the episode of diarrhoea.
Professor C. C. J. Carpenter, Chairman, Department of Medicine, University Hospitals
of Cleveland, Ohio, USA. * Hypovolemic shock - circulatory failure due to rapid fall in blood volume through
dehydration. Further reading: Pierce N F, Hirschhorn N 1977 Oral fluid - a single weapon against dehydration in
diarrhoea. WHO Chronicle, Vol 31, 87.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 12 February
1983  5 Page 6 7 5 Page 6 7
Control strategies
Although many questions remain about the epidemiology of cholera, there is little
doubt about the most effective control measures. Dhiman Barua
reviews the key strategies. Cholera control can best be achieved through a national CDD programme that ensures
adequate training, proper treatment, community involvement, uninterrupted supplies of ORS,
laboratory and other back-up facilities, regular surveillance, and measures to improve
water supply, excreta disposal, personal hygiene and food safety. The important strategies
for cholera control are described below:
- Early detection of epidemics through continuous surveillance.
- Active case-finding with the help of community elders, religious leaders and
teachers, and through home visits by local health workers reinforced by mobile teams, if
necessary.
- Provision of early and proper treatment of cases. This includes the establishment
of temporary treatment centres if the permanent facilities are not within easy reach, so
infected people travel as little as possible.
- Extremely thorough disinfection of the clothing, utensils, excreta, vomit, and
environs of cholera cases (by boiling, or with disinfectants like lysol, cresol or lime,
as appropriate). The dead bodies of cholera victims should be disposed of with the minimum
of transportation and rites, which can spread the disease.
- Health education, properly carried out, can achieve a great deal, even in the
most desperate situations. All health workers should provide health education while
providing services. All appropriate media should be used and special attention given to
densely populated areas. Simple explanations of factors helping the local spread of
disease and the ways in which the population can help interrupt transmission will secure
community involvement and minimise panic.
Emphasis on personal hygiene (especially hand-washing with soap and water) and on food
and water safety is essential. The necessity for eating only cooked food while still hot
and drinking only safe water (boiled, treated, or collected from a safe source and stored
properly) should be explained. The need to protect all water sources from contamination
must be emphasized; infection is acquired not only by drinking water, but also by bathing
or washing articles at contaminated sources. The population should also be informed about
the dangers of:
- community feasts and gatherings of any kind, particularly funerals, where safe food and
water and proper excreta and waste disposal cannot be assured;
- visiting sick relatives and eating/drinking in the homes of cases;
- contaminated foods e.g. fish and especially shellfish collected from suspect waters,
vegetables irrigated or freshened with sewage-contaminated water.
- Epidemiological investigations to determine how transmission is occurring should
be undertaken by health workers. In most instances, several factors are involved because
of the complex socio-cultural customs of intimate mixing and free exchange of foods/drinks
etc, but there are instances when a common source/vehicle (like a well, shellfish,
vegetables) has been detected by epidemiological investigations, in which case the
outbreak can be quickly controlled by specific interventions.
- Provision of safe water is very important, as the boiling of water is not
practical in many situations. Numerous simple and innovative methods are available for the
supply and treatment of water. Special attention should be paid to the proper protection,
storage and use of water in the home.
- Proper disposal of excreta is vital to protect water sources and the environment.
In the absence of any facilities, burial of all excreta, specially those of cholera cases,
is essential. Refuse disposal by burning, burial, or other methods should be ensured to
prevent fly breeding.
- Chemoprophylaxis i.e. the administration of antimicrobials to healthy persons who
are suspected of carrying V. cholerae and are likely to become sick or spread the
infection is theoretically a sound measure. Yet many countries have experienced that mass
chemoprophylaxis does not produce the desired results mainly because the infection spreads
faster than the time it takes to reach and treat all members of the community. Moreover,
by inducing drug resistance, it deprives the actual cases of an effective drug for their
treatment.
Therefore, chemoprophylaxis only of close contacts in the home of a
case was recommended. Recent experience has shown, however, that in many areas the custom
of intimate mixing of members of the community and of visiting and sharing foods with
extended families makes it difficult to identify close contacts; the recommendation thus
becomes unpractical. Chemoprophylaxis may still be effective in situations where everybody
in the affected community can be treated quickly and simultaneously e.g. a
refugee camp.
- Vaccination is no longer seen as an effective weapon for cholera control because
of its low efficiency in preventing disease and almost total ineffectiveness in preventing
the carrier state. Vaccination is still undertaken in some situations, mainly because it
is demanded by an uninitiated public. This should be countered by proper health education
explaining the limitations of the vaccine and the risks of mass vaccination (e.g.
hepatitis).
Dr Dhiman Barua, Programme for the Control of Diarrhoeal Disease (CDD), WHO, Geneva,
Switzerland. For further reading on this subject contact Dr Barua at the above address.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 12 February
1983  6 Page 7 8 6 Page 7 8
- Community-based health and family planning
Kols A J and Wawer M J Population Reports 1982 X.6 (Series L No 3) pp 79-109
- Oral rehydration therapy: an assessment of mortality effects in rural Egypt.
Tekce B Studies in Family Planning 1982 13:11 pp 315-327.
Involvement of local people, readily available supplies and cultural acceptability are
all reasons why community-based distribution (CBD) of health resources should be
effective. If essential supplies can be obtained nearby there is less difficulty and cost
to poorer families. Communication is easy and items will be more readily accepted if they
are stocked by members of the community who understand how to use them and can explain how
they suit health needs and beliefs. A number of programmes are using CBD for
contraceptives, nutritional supplements, simple treatment for intestinal parasites,
malaria and oral rehydration for diarrhoea. However, operating CBD programmes is demanding. Local depot holders must be trained,
supervised and given regular supplies. Parents need motivation and education to use the
materials correctly. Repeated personal instruction and contact is necessary to remind
people about the availability of supplies and to refresh memories about the right way to
use the facilities. Treatment of acute diarrhoea with oral rehydration therapy (ORT), is an important
technique that can be taught and applied through CBD. However, ORT is time and labour
intensive. Instruction also has to overcome fears and doubts about the method. Some of
these are associated with traditional beliefs and remedies, while others are the result of
resistance and routine practices of doctors and health workers. Several studies of ORT in CBD in Egypt have shown that it can be effective in lowering
the death rate due to diarrhoea in communities. In one study the diarrhoea mortality was
decreased with Oralyte, sugar-salt packets or household fluid programmes.
Egyptian Project,
Strengthening Rural Health Delivery |
Deaths per 1,000 children 1 month to 5 years of
age
in two periods and with various services |
| |
1976-79 |
1980 |
| Oralyte, home distribution |
18.9 |
11.2 |
| Oralyte, commercial source |
19.9 |
16.9 |
| Home prepared sugar-salt |
17.7 |
10.3 |
| Prepackaged sugar-salt, home distribution |
23.4 |
9.3 |
| Control area 1 |
19.4 |
17.3 |
| Control area 2 |
21.5 |
18.8 |
Such improved death rates were not found universally, and in the
Menoufia programme there was no lowering of the diarrhoea death rates in a community in
which mothers were given two Oralyte packets and taught how to use these for their
children in cases of diarrhoea. Apparently in most instances ORT was used too little or
too late. Both these reports emphasize the need for repeated personal instruction and suitable
ongoing support for effective impact from oral rehydration programmes.
- Evaluating the role of health education strategies in the prevention of diarrhoea
and dehydration
Iseley R B Journal of Tropical Pediatrics October 1982 Vol. 28 pp 253-261
Health education can interrupt the lethal diarrhoea-dehydration cycle at three points:
prevention of diarrhoea; management of diarrhoea when it occurs; and the management of
dehydration. However, ways to evaluate the impact of health education strategies are badly
needed. Experienced field workers suspect that community organization is a key element in
bringing about behavioural change and this cannot be achieved through the mass media alone
without local involvement. Village-based health workers are the most effective carriers of
educational messages at household level but they need cooperation from both the mass media
and community leaders in setting up local programmes to deal with diarrhoeal disease
control. Such programmes should include not only environmental improvements but also the
provision of resources for effective oral rehydration therapy, together with the
encouragement of prolonged breastfeeding and better weaning practices. Measuring behavioural change is not easy. This article describes a 'health belief'
model which can be adapted to a traditional culture to provide a framework out of which
evaluation questions can be selected for use. Some form of relevant, local evaluation is
essential if health education services are to be effectively designed to maximize scarce
resources by combining the use of mass media with various types of local interventions to
prevent diarrhoea and dehydration.
|
Journal of Diarrhoeal Diseases Research The International Centre for Diarrhoeal Diseases Research, Bangladesh (ICDDR, B)
(originally known as the Cholera Research Laboratory) is soon launching a Journal of
Diarrhoeal Diseases Research with the encouragement and support of the Canadian
International Development Research Centre (IDRC). The Journal will be a quarterly
publication with an annual index. Contents will include original research articles, short
communications and letters dealing with all aspects of diarrhoeal diseases. There will be special emphasis on the Asian region and each issue will include an
annotated bibliography of current Asian literature on diarrhoeal diseases. The scientific
editors of Diarrhoea Dialogue are both members of the Editorial Advisory
Board and the first issue of the Journal will be fully reviewed in the appropriate issue
of this newsletter. Contributions to the new Journal will be welcomed by its Managing Editor, Mr Md. S. I.
Khan, Journal of Diarrhoeal Diseases Research, lCDDR, B DISC, GPO Box 128, Dhaka 2,
Bangladesh.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 12 February
1983  7 Page 8 7 Page 8
Saving lives
I am the coordinator for the National and Child Health Clinics in this region. We've recently had an extensive epidemic of diarrhoea and dysentery in Tanzania. In
your="dd11.htm">issue No 11, November 1982, I was pleased to read about oral
rehydration therapy (ORT), as we taught it repeatedly to the women who attend our clinic.
Medicine for diarrhoea is almost nil here and ORT was the means to save the lives of many
of the children. I will be particularly interested to read issue No 12 as we are presently treating
cholera. Thankfully, the cases are under control and declining steadily. Sister Katherine Taepke, Makiungu Hospital, P. O. Box 56, Singida, Tanzania.
Local foods Dorothy Francis has written an excellent article on the necessity for continued feeding
during diarrhoea to avert the onset or increase of PEM. Locally available multi-mixes are
rightly commended (Diarrhoea Dialogue 10, page 66). Our Nepal-wide multi-mix (½ roast pulse, ¼ roast grain 'a', ¼ roast grain 'b') and
Kathmandu Valley multi-mix (½ roast soya bean, ¼ roast maize, ¼ roast wheat) - both
called 'Sarbottam Pito' or Super Flour, include soya or other legumes roasted and ground.
Contrary to Dorothy Francis's point of view, we do not find that legumes (roasted
and finely ground by the local traditional process) cause additional digestive
problems.(1) 'Sarbottam Pito' can be used very satisfactorily for young children of five months
upwards, or even three months if mother's milk is genuinely not available. The soya
and cereal mix provides a good combination of amino acids, necessary potassium and other
essential nutrients. I regret that many of the foods listed in Miss Francis's Table 'A' - chicken, rabbit,
beef, lamb (or indeed any meat), egg, arrowroot and often even oils are
scarce and expensive in this developing country. However, our multi-mix provides needed
calories too, and the recipe may be a useful basis for other similar areas to provide
appropriate local diets. Ruth Angove, Nutrition Adviser, UMN Health Services Board, United Mission to Nepal,
P. O. Box 126, Kathmandu, Nepal. (1) Bomgaars Mona R 1976 Undernutrition - Cultural Diagnosis and Treatment of
'Punche'. JAMA, Nov 29 1976, Vol 236, No 22, p. 2513.
Sarbottam Pito 2 parts by volume of one pulse (soya-bean is the best)
1 part each by volume of two cereal grains
- Clean and roast each of the ingredients separately and grind into flour.
- Mix the resulting fine (sifted) flours.
- Store in a closed clean container.
- To prepare the child's feed: boil sufficient water, add the powder, and stir while
boiling briefly. Cool, add a little salt if needed, and use as a weaning or supplementary
food.
|
ORT for adults
Thank you very much for your issues of Diarrhoea Dialogue. I would like to
continue receiving it. I have closely followed your discussions on oral rehydration therapy and enjoy reading
them very much. We in Fiji are recipients of the UNICEF salts packages, which have gone a
long way in controlling our diarrhoeal diseases. But one issue concerning these packages
really concerns me. I have often seen my fellow colleagues issuing these packages to adults suffering from
diarrhoeal diseases. I should be very grateful if in a future issue of Diarrhoea Dialogue you could
discuss the following:
- Should adults be prescribed these UNICEF packages?
- If no, are there any special adult preparations of salts packages?
- Will an early replacement therapy be of any use to adults?
Please accept my appreciation for the task you are undertaking on educating and keeping
us abreast (particularly those of us from developing countries) of developments in the
world of diarrhoea. Yours in health, Dr A W Khan, Medical Officer, Tavua Hospital, Tavua, Fiji Islands, South Pacific.
Editors' note:
 |
Spreading the ORT message to everyone. This letter demonstrates the need to spread the ORT message more widely and more
clearly. Anyone who has diarrhoea needs early oral rehydration therapy, regardless of age
or size. Because dangerous dehydration occurs so quickly in small children, they must be
the first to benefit from the special UNICEF packets. The formula also works for adults
but they can, as an alternative, be advised to drink large amounts of water to which
glucose or sugar and a little salt has been added.
|
If packets are not available, children may also be given similar
home made oral rehydration mixtures as described in earlier issues of Diarrhoea Dialogue.
Not more than a pinch of salt should be used to a cupful of water or a teaspoon to a
litre; too much salt is not good for children.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Executive editor Denise Ayres Editorial advisory group
Professor David Candy (UK)
Dr I Dogramaci (Turkey)
Professor Richard Feachem (UK)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr D Mahalanabis (India)
Professor Leonardo Mata (Costa Rica)
Dr Mujibur Rahaman (Bangladesh)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from WHO, UNDP, UNICEF GTZ and SIDA
|
Issue no. 12 February 1983
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
updated: 23 August, 2019
|