|
| |
Issue no. 29 - June 1987
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 29 - June 1987
|
DDOnline Dialogue
on Diarrhoea Online Issue 29 June 1987  Page 1 2
Page 1 2
Training the trainers
While communities mostly possess good sense and will co-operate in behaviour change
when they are shown that this is to their advantage, it may be more difficult to persuade
some health professionals that they will receive any personal advantage from the promotion
of oral rehydration therapy. Yet their attitudes are crucial if the idea of drinking as
the appropriate response to diarrhoea is to become successfully imbedded in the minds of
all ordinary people. Health professionals must themselves be convinced that oral
rehydration works satisfactorily enough to be considered the correct scientific response. Need for new attitudes
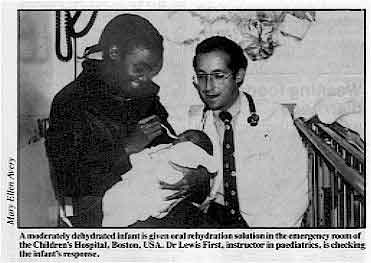 |
A moderately dehydrated infant is given oral
rehydration solution in the emergency room of the Children's Hospital, Boston, USA. Dr
Lewis First, instructor in paediatrics, is checking the infant's response.
Medical education has tended to emphasise the responsibility of doctors to intervene,
to apply their special knowledge in a way that adds, often dramatically, to their status.
As the possibilities of dramatic intervention have increased, thanks to the growth in
scientific knowledge over the last 50 years, so has the seductiveness of advanced medical
technologies.
|
To set up an intravenous drip or to prescribe a new 'miracle' drug has more appeal than
recommending the giving of a simple drink.
Doctors have spent years learning the mysteries of medicine, but now in diarrhoea, they
are being asked to co-operate in demystification of medical technology. They are being
asked to recommend a remedy which any family can learn to carry out at home, given simple
instructions and simple ingredients. In the case of oral rehydration programmes for
treatment of acute diarrhoea, whatever the causative agent, the attitude of influential
medical leaders, especially the paediatricians, is crucial. They are the ones who teach
the medical students and order the treatment procedures in hospitals and health centres.
Only when they are convinced will ORT be fully accepted at all levels as the treatment of
choice. Learning by doing
To achieve this goal, the scientific basis of ORT needs to be continually stressed.
Theory, however, is of little use without practice, and 'learning by doing' is an
important part of the detraining and retraining process. Oral rehydration, properly
carried out, is dramatic in its effects; anyone who has personal experience of orally
rehydrating a severely dehydrated child cannot fail to be convinced of its value. Nothing
in the way of information can replace that actual experience. In thinking about training
at all levels, it is useful to remember the adage:
What I hear, I forget
What I see, I remember - but
What I do, I know.
This issue of DD highlights some recent initiatives that have been taken to
improve medical training in management of diarrhoeal diseases, and also includes practical
guidelines for evaluating the effectiveness of training programmes. KME and WAMC
|
In this issue . . .
- Improving medical training
- Children as educators
- Evaluating training
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 29 June 1987  1 Page 2 3 1 Page 2 3
India: ORT survey To find out more about current practices and beliefs concerning diarrhoeal disease and
its treatment, a questionnaire was sent to 200,000 doctors throughout India. The following
is a summary of findings based on the 15,000 replies received (7.5 per cent). The majority
were returned by modern allopathic practitioners, although about one-quarter were returned
by doctors from indigenous and other systems of medical care. All respondents had received
the WHO/UNICEF Joint Statement on ORT. Two-thirds claimed to use ORS in their practice. A
similar percentage believed that mothers can manage most diarrhoeal cases at home and 76
per cent claimed that mothers already give fluid to their children during diarrhoea.
Three-quarters of respondents stated that they teach mothers how to make ORS as part of
their advice. However, while over 70 per cent cited correct quantities of salt and sugar
for mixing home-made ORS, more than a quarter suggested formulas scientifically considered
to be unsafe, indicating an urgent need for further education and standardisation of
formulations. Feeding The overwhelming majority of doctors who replied (94 per cent) were aware that repeated
diarrhoeal episodes contribute to malnutrition, but 60 per cent recommended less food to
be given during diarrhoea, and the same number recommend a change from regular diet to
liquids and soft foods. Almost one-third recommend continuation of breastfeeding but
stoppage of all other foods. Clearly more information and teaching is needed about correct
nutritional support of children with diarrhoeal disease. Drug therapy Thirty-seven per cent of all doctors claimed anti-diarrhoeal preparations are
absolutely essential in all cases of diarrhoea, and another 55 per cent felt they were
sometimes essential. This use of anti-diarrhoeals by nearly all respondents demonstrates
the extent of the problem, for these drugs generally divert attention from oral
rehydration and are also too expensive for most families. Antibiotics are used regularly
by 40 per cent of doctors, although most claimed that they use them only in selected
cases. Intravenous (IV) fluids are used by 80 per cent of doctors in less than 15 per cent
of cases. WHO and Indian experts have, however, estimated that only 1 per cent of all
cases need IV fluids. While many Indian practitioners are clearly conversant with the ORT message and claim
to be using it in their practices, important efforts are needed to:
- promote use of standard and effective fluids in the home for early treatment of
diarrhoea;
- reduce dependence on, belief in and use of anti-diarrhoeals;
- influence more judicious and selective use of antibiotics; and
- improve nutritional management of the child with diarrhoea.
Rolf C. Carriere, Chief, Health and Nutrition, UNICEF, Regional Office for
South-Central Asia, 73 Lodi Estate, New Delhi 110 003, India. Editor's note: When, as in this survey. only a small percentage of questionnaires are returned and
analysed, further studies may need to be carried out to determine the actual practices of
mothers and physicians. WHO is currently developing protocols to measure practices and
effective case management in the home and in health facilities. Weaning foods and diarrhoea In many parts of Eastern and Southern Africa porridges are made by fermentation of a
cereal 'mash' with various species of lactobacilli. Milk or milk products are not used in
the process, and these porridges are often prepared by people who do not have access to,
or cannot afford, milk. (After a day or so the porridge becomes sour and the pH falls to
around three. No alcohol is formed.) Sour porridges are prepared by a wide range of
methods from sorghum, millet, maize or a mixture of these cereals. In some countries, for
example Lesotho and parts of Kenya, these porridges are popular weaning foods for young
children. In other countries sour porridges are popular among adults but are not given to
young children, although this may not have been the case in the past. There is considerable evidence which suggests that fermenting with lactobacilli and the
resulting low pH of sour porridges due to lactic acid formation significantly reduces the
chances of contamination with coliform bacteria likely to cause diarrhoea. (Such an effect
is of course widely recognised with sour milk products but the literature on the lactic
(as opposed to the alcoholic) fermentation of cereals is not very extensive.) Souring of
cereal porridges may therefore be an appropriate technology facilitating the frequent
feeding of young children. A large batch of porridge could be prepared in advance and
safely stored until needed for child feeding. This would be more practical than advocating
cooking fresh weaning porridge three times a day when constraints on women's time,
availability of fuel, washing facilities and utensils are considered. Some evidence suggests that lactic fermentation reduces the viscosity of the porridge
thus making easier the preparation of energy dense porridges. Fermentation also increases
the digestibility of sorghum protein and bio-availability of many vitamins and minerals.
Mothers have said that sick and anorexic children like the taste of the sour porridge and
that this encourages them to eat. People in many countries also believe that sour sorghum
or millet porridge stimulates the production of breastmilk. Given this long list of
apparent advantages it is perhaps surprising that health workers in the region have not
been more keen to promote the use of sour porridges in young child feeding. Some health
staff claim that they cause indigestion and heartburn (although mothers that I have talked
to do not agree) and that they are difficult to mix with other foods. Fashion, and the
increasing tendency towards western ways of doing things, and the fact that such
traditional foods are rarely discussed when health workers are trained may be more
important reasons which discourage use of such porridges. I am collecting information to help clarify the advantages and disadvantages of this
technology with respect to young child feeding, and would welcome comments from DD readers. David Alnwick, Regional Advisor, Household Food-Security and Nutrition,
UNICEF, Eastern and Southern Africa Regional Office, Nairobi, Kenya.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 29 June 1987  2 Page 3 4 2 Page 3 4
Improving medical education
Medical school training determines the future practice of doctors regarding
management of diarrhoea. Perla Santos Ocampo reports on
initiatives in the Philippines. The crucial role of the physician in supporting ORT cannot be too highly
emphasised.
The physician is seen by other health workers as the leader in health care delivery. His
practices, based on medical school training, are imitated. Unfortunately, the need to
impress patients and the desire to apply what has been learned in medical school may mean
that he will ignore a simple intervention, such as ORT, even though this is known to be
sound, scientifically based and effective. Instead, drug and IV therapy may be used for
acute diarrhoeas, and this is reinforced by public demand. Need for curricula changes Changes in curricula are thus needed to emphasise the role of ORT in the management of
acute diarrhoea. In the Philippines, the Task Force on Paediatric Education (under the
Association of Philippine Medical Colleges), decided it was necessary to focus on low-cost
highly effective health technologies such as oral rehydration in diarrhoea, and
immunisation, in the competency-based paediatrics curriculum. Medical school commitment The first step was to ensure the involvement of both the Dean and Chairman of the
Department of Paediatrics of all 26 medical schools in the Philippines in a two day
workshop. The commitment of the deans 'to offer curricular programmes emphasising these
effective health technologies and to give the necessary assistance and support to promote
the teaching of these effective health technologies to undergraduate medical students,
including the provision of community-based outreach programmes and 'hands-on' (practical
and personal) experience was obtained. The Task Force then formulated learning objectives
for teaching about diarrhoeal diseases in medical schools. Learning objectives and training methods The learning objectives are orientated towards practical skills and relate to the
community. As far as possible, teaching is to be conducted in different locations: in the
community, ambulatory care areas, wards or ORT corners. Adopting learning objectives is
not enough. Most important are the teaching methods used to communicate to students the
superiority and usefulness of ORT, and the knowledge and skills needed for its correct
use. Other teaching methods than lectures, such as role-play, group discussions,
demonstrations, direct patient interaction, pretests, post-tests, working tests, and case
presentations are encouraged.
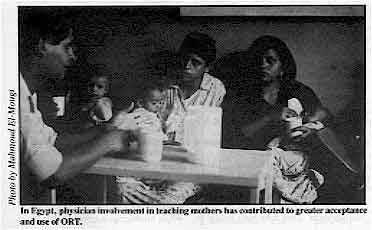 |
In Egypt, physician involvement in teaching mothers has
contributed to greater acceptance and use of ORT. The whole clinical team, including physicians, residents, interns, nurses, dietitians
and pharmacists, is to be involved in teaching. Teaching about diarrhoeal diseases will be
integrated with other disciplines, including community and family medicine. Modules are
now being developed by the various medical schools to emphasise ORT and other strategies
in the control of diarrhoeal diseases.
|
'Hands-on' experience Opportunity for hands-on experience is crucial: students must do and see for themselves
the improvement brought about in just a few hours using ORT. In a preliminary survey,
medical students exposed to an ORT corner in the University of the Philippines were
impressed with the efficacy, safety, simplicity, and cost-effectiveness of oral
rehydration. There is no substitute for hands-on experience in converting non-believers to
ardent exponents of ORT. It is most important that medical students learn about the value
of ORT and other proper diarrhoeal disease control measures in order to produce physicians
whose diarrhoea management practices are safe, effective and appropriate and which place
due emphasis on ORT. Physicians as trendsetters Medical opposition has been recognised as a significant obstacle to use of ORT in
diarrhoea management. If highly respected physicians, in their capacity as opinion leaders
or trendsetters in the community, use ORT in their practices, this can effectively add
prestige to ORT as the treatment of choice for acute diarrhoea. Perla D. Santos Ocampo, MD, Professor of Paediatrics, University of the Philippines,
Chairman, Task Force on Paediatric Education, Association of Philippine Medical Colleges,
Manila, Philippines. Professor Santos Ocampo is also President Elect of the International
Paediatrics Association.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 29 June 1987  3 Page 4 5 3 Page 4 5
Recent initiatives In August 1985, medical educators met in Geneva to seek areas where current
medical education about diarrhoea might be improved. Robert Northrup
and Roberto Unda report. Why do so many physicians resist using ORT, even new graduates from medical school?
This problem is a challenge for diarrhoeal disease control programmes in many countries
since physician behaviour strongly influences the behaviour of other health workers and
mothers. More is involved than just the choice between intravenous or oral rehydration:
- physicians often use unnecessary anti-diarrhoeal drugs and antibiotics to treat acute
watery diarrhoea;
- they often recommend 'resting the gut' during diarrhoea rather than continuing feeding;
- they often communicate poorly with mothers, so that mothers leave the clinic without a
clear understanding of how to prepare and administer oral rehydration solution, or how to
detect signs of dehydration; and
- they often direct and supervise health centre and community diarrhoea programmes, but do
so poorly.
Many factors influence the behaviour of doctors. These range from drug promotion by
pharmaceutical companies to Ministry drug buying policies, from the greater profitability
of drugs over ORS packets to pressure from patients to use intravenous treatment. However,
all agree that the doctor's basic medical education about diarrhoea is a critical
influence on subsequent behaviour. Teaching deficiencies A number of aspects of medical teaching support or discourage ORT and appropriate CDD
behaviours in the graduate physician. These are presented as a kind of checklist for
medical schools about their diarrhoea teaching.
- Does the teaching hospital have a diarrhoea rehydration unit which emphasises oral
rehydration and continued feeding for diarrhoea patients? Is there an oral rehydration
'corner' in the paediatric outpatient or ambulatory clinic?
- What percentage of mild and moderately dehydrated patients are treated with ORS? With
intravenous fluids? With anti-diarrhoeal drugs? With antibiotics?
- What percentage of mothers of diarrhoea patients know when they leave the clinic how to
prepare and administer ORS correctly, how to feed their child during diarrhoea and
afterwards, and how to check for dehydration?
- How many diarrhoea patients has each medical student managed personally by graduation?
How many cases has he orally rehydrated with his own hands? How many children with
diarrhoea has he fed himself?
- How many individual mothers has each medical student taught about ORT and diarrhoea
prevention? How many groups of mothers? Does the school check the student's teaching by
interviewing the mothers to see if they have actually learned?
- Does the medical school curriculum include activities to produce skills in teaching
about ORT and feeding during diarrhoea, knowledge about the national diarrhoea control
programme, skills in designing and carrying out a community survey about effective use of
ORT by mothers, and skills in planning, implementing, and evaluating a project in
diarrhoea control for a community?
Changing the curriculum Where in the curriculum are good learning experiences about diarrhoea and ORT most
critical in affecting future behaviour? The final clinical rotations, where the student's
see their paediatric professors treating patients correctly or incorrectly, and where they
treat diarrhoea cases themselves, are doubtless much more important than the lectures or
laboratory sessions of earlier years, which are usually quickly forgotten. To make clinical teaching most effective, the group recommended the following:
- Every medical school should have a Diarrhoea Training Unit (DTU)
As described
by WHO (1), a DTU is primarily a set of clinical teaching activities rather than a
particular clinic room or ward. Thus, students learn from direct experience how to assess
dehydration. They rehydrate mildly or moderately dehydrated patients, giving oral fluid to
the child themselves, and learning effective methods to teach mothers ORT for home use.
In the emergency room, the ambulatory paediatric clinic, and the inpatient ward, the
DTU functions to establish treatment policies and monitor care given. Students passing
through each of these areas, as part of the diarrhoea curriculum, learn from direct
experience the skills of inserting IVs and nasogastric tubes for severely dehydrated
patients, of managing dysentery and chronic diarrhoea, and of linking feeding and
nutrition to diarrhoea management. In a well-run DTU the students' professors become role
models practising correct diarrhoea management with emphasis on ORT. Their example
motivates students to manage diarrhoea patients in the same way.
- Ten diarrhoea patients before graduation
Getting enough experience is
essential. One case is not enough to teach the necessary skills in diarrhoea management.
It was suggested that a minimum of ten cases of paediatric diarrhoea must be managed
properly by every medical student before he can graduate. The need for a supervisor's
signature in the student's logbook, and the use of an objective supervisor's checklist and
interviews with mothers will help to ensure that treatment and education of mothers are
carried out properly and effectively.
- Skills in management, supervision and community diarrhoea control
Physicians
are more than diarrhoea clinicians. Medical school education should also prepare students
for their wider future responsibilities. Even new graduates are often made responsible for
planning, implementing and evaluating community diarrhoea programmes. They become trainers
of other health workers and community groups. They supervise other health workers in
diarrhoea treatment, and community level diarrhoea prevention and control activities.
Adequate direct experience during training, often in the community and in health centres,
is necessary to give students the skills needed to carry out these activities. Focusing on
diarrhoea can make these experiences more measurable and meaningful to students.
- Skills and problem-solving
While knowledge is certainly needed as a basis for
most of these skills, knowledge-oriented activities like lectures are often
over-emphasised in medical school curricula. First priority should be given to activities
and practical skills. Faced with a clinical or community problem to solve, medical
students will be motivated to seek the necessary knowledge themselves.
- Clinical learning modules
As a follow up to this meeting, PRITECH (under
contract to WHO/CDD, and with additional support from USAID), is producing clinical
learning modules for use in medical schools. The initial ones will be related to clinical
teaching in the DTU. Modules for community teaching will be developed subsequently. Each
will include detailed educational objectives; an instructor's guide for carrying out the
activities in the module; special attachments and readings for the instructor; and student
handouts and readings. A bank of examination questions will provide pre-tests, post-tests
and working tests for each module as well as final examinations. Special supervisory
checklists have been prepared to improve clinical supervision and ensure that skills have
been acquired by the student. A general instructor's manual will give sample schedules for
the activities, provide general instruction on how to run the different types of learning
activities, and describe how to use the exam bank. The types of learning activities used
include readings; simulated cases; group discussion; debates; role-playing; demonstration;
clinical rounds; direct patient care.
Modules being prepared for the clinical component are:
- effective doctor-mother interaction;
- clinical management of diarrhoea cases with no or some dehydration;
- clinical management of dysentery, chronic diarrhoea, and diarrhoea accompanying other
diseases;
- nutrition and feeding in diarrhoea;
- assessment and monitoring of clinical care.
1. Diarrhoea Training Unit Director's Guide, WHO, CDD/SER/ 86.1, 1986.
Dr Robert S. Northrup and Roberto F. Unda, PRITECH, Medical Education in Diarrhoea
Control (MEDIAC) Project, Management Sciences for Health, 1655 N Fort Meyer Drive,
Arlington, VA 22209, U.S.A.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 29 June 1987  4 Page 5 6 4 Page 5 6
An American perspective Mary Ellen Avery and John Snyder
report on acceptance and use of oral rehydration therapy in the United States. Where it has been implemented in developing countries, oral rehydration therapy (ORT)
has been shown to be safe, effective and inexpensive. In the past in the United States,
mild diarrhoea was treated with avoidance of solid foods and substitution of 'clear
liquids'. We now know that these 'clear liquids': tea, carbonated beverages, broths and
fruit juices can be appropriate fluids to prevent dehydration and maintain hydration, but
are not appropriate for treatment of clinical dehydration. At least seven commercially manufactured oral glucose-electrolyte solutions are
available which approximate the WHO formulation. Most have slightly less sodium, about 50
to 70 mEq, but have proved to be effective maintenance and rehydration solutions in
controlled trials in infants and young children. These ready-made solutions are available
at most supermarkets and are sold without prescription. Packets of salts and glucose to
mix with water are also available without prescription, but are less widely used than the
more convenient (but also more expensive) ready-to-use solutions. The frequency, volume,
and effectiveness of packet use has not been reported in population-based studies, but is
felt to be growing. However, expense may limit use of commercial rehydration drinks among
the poorer socio-economic population groups who could most benefit from them. 'Hands on' experience of ORT At the Children's Hospital, Boston, where mostly mild to moderate dehydration is seen,
treatment in the out-patient department is started with oral rehydration, following the
WHO/UNICEF guidelines. A programme of instruction and 'hands-on' experience with ORT has
been established. Major reasons for preferring oral rehydration are that it is safer than
intravenous therapy, it often avoids hospital admissions, and it provides the opportunity
to educate parents about its early use at home. Furthermore, we are anxious that our
students and housestaff gain first-hand experience with ORT so that they will see its
effectiveness and at least will be prepared to challenge the old belief that intravenous
rehydration is somehow preferable. Without 'hands-on' experience it is often difficult to
convince those who have used intravenous rehydration successfully for years that a therapy
so simple and so inexpensive is indeed better. IV used only rarely Intravenous solutions are given only in unusual cases, such as very young infants with
diarrhoea in whom we suspect sepsis and want to start intravenous antibiotics pending
results of blood, urine, and cerebrospinal fluid cultures, or children with severe
dehydration, shock or coma. Even then, as soon as the child can drink, maintenance oral
hydration by mouth is given, and more calories are gradually introduced by eight to 24
hours in patients under the age of six months, and earlier in older children. ORT for burns Oral rehydration can also be a life-saving measure in other situations. Immediately
after an extensive burn, a child may still be responsive enough to take oral fluids, which
will help to lessen the net loss of fluids caused through blisters and loss of skin. At the Boston Children's Hospital, giving fluids by mouth is endorsed as the best means
of preventing dehydration, and oral rehydration as the best therapy in the face of fluid
losses. We expect continued acceptance of these measures and a reduction of dependence on
intravenous therapy in the future. Mary Ellen Avery, Thomas Morgan Rotch Professor of Paediatrics and John Snyder,
Assistant Professor of Paediatrics, Harvard Medical School, Boston, MA 02115, USA.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 29 June 1987  5 Page 6 7 5 Page 6 7
Evaluation of training Birger Forsberg describes several methods for evaluating
the impact of training on the practices of health workers. Training in programmes for the control of diarrhoeal diseases (CDD) is very much
oriented towards changing health workers' performance in supervisory activities and their
behaviour in the treatment of diarrhoea. It is becoming increasingly important to evaluate
this aspect as countries accelerate their programme activities. Some countries have
started to develop methods for evaluating the impact of training on the practices of
health workers. Follow-up In the United Republic of Tanzania, for example, a series of clinical management
workshops was held in 1986. Supervisory visits are now being made to participants, six to
12 months after the training, to assess how they are applying the skills taught at the
workshops. As one of the objectives of the training was to teach participants how to
organise diarrhoea training sessions, this area is given special attention during the
follow-up visits. The trainees are given the opportunity to explain their problems and the
assistance they need to successfully promote proper diarrhoea management in their
hospitals. This type of follow-up is appropriate when a training programme is focused on a
small group of persons who have a major responsibility in the CDD programme. It is not
feasible for the evaluation of large-scale training activities. Nepal provides an example of how extensive programmes can be evaluated. The country is
training health workers in a new regionally phased programme. During a CDD programme
review in 1986, the practices and skills in the treatment of diarrhoea of a random
selection of health workers were assessed (Table 1). Records showed that children treated
at health posts in districts where the staff had been trained were significantly more
likely to receive ORS than those in 'untrained' districts. There was little difference in
the use of antibiotics between the two groups. Written guidelines for diarrhoea treatment
were available more than twice as often in facilities with trained personnel.
|
Table 1.
Availability of written guidelines
and frequency of treatment of diarrhoea with ORS and antibiotics at health posts, Nepal |
| |
With trained staff |
With untrained staff |
| No. |
Per cent |
No. |
Per cent |
| Health posts surveyed |
13 |
- |
13 |
- |
| Posts with treatment guidelines |
7 |
54 |
3 |
23 |
| Diarrhoea cases in under-fives |
219 |
- |
103 |
- |
| Cases treated with ORS |
156 |
71 |
48 |
47 |
| Cases treated with antibiotics |
178 |
81 |
96 |
93 |
Comparing trained and untrained health workers Interestingly, interviews with health workers did not reveal any differences between
trained and untrained health post workers in knowledge of how to assess and treat
diarrhoea, primarily because the untrained health workers were fairly familiar with these
skills already. This suggests that the training has been partially successful in changing
the practices of the health workers with regard to the use of ORS. Further efforts must
now be made during training to discourage the use of antibiotics. Checking records Another example can be taken from Sudan. A rural health training programme was
evaluated by a review of daily attendance records at different health stations. This
involved counting total numbers of visits, diarrhoea and dysentery cases, and cases given
antibiotics, ORS, or both. Records were checked before training in ORT, and at intervals
of one, six and 18 months after training. The results are shown in Table 2.
|
Table 2.
Diarrhoea and treatment
with ORS and sulphonamides, Sudan |
| |
No. of cases |
ORS |
Sulphonamides |
| |
% |
% |
| Before introduction of ORT |
1140 |
8 |
76 |
| 1 month after training workshops |
698 |
64 |
45 |
| 6 months after training workshops |
1981 |
59 |
38 |
| 18 months after training workshops |
4060 |
72 |
22 |
The training appears to have had a definite impact on the behaviour of
the health workers; ORS was prescribed much more often and antibiotics less often than
before the workshops. Evaluation is an important part of training programmes. These examples illustrate some
ways of evaluating the impact of training on the actual performance of health personnel:
- follow-up visits including discussions with trainees;
- interviews, observation and comparison of trained and untrained health workers; and
- checking and comparison of hospital records before and after training.
Health staff in charge of CDD programmes and Diarrhoea Treatment Units (DTUs) could
consider including such methods in their training programmes. Birger Forsberg, MD, Evaluation Officer, CDD Programme, WHO, 1211 Geneva 27,
Switzerland.
DD would like to hear from readers about their own experiences with evaluation of
training.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 29 June 1987  6 Page 7 8 6 Page 7 8
Children can be teachers Mark Swai describes how children, taught about ORT at
school, can help to reinforce learning by mothers. In the Moshi district of Tanzania, 79 children from the older classes of two randomly
selected primary schools were given questionnaires to answer, about diarrhoeal disease and
how to treat it. This was followed by two activity lessons about diarrhoea which included
making visual aids and participating in making oral rehydration solution with sugar, salt
and water. The children were also given 'homework' which involved showing their parents
the visual aids and discussing with them what they had learnt at school. What mothers already knew The children's mothers were asked questions before and after the children did their ORT
'homework'. There was a wide variation in what the mothers knew already about diarrhoeal
disease. Some thought it was 'not serious', while in one tribal group it was described as
'enemy number one'. Many realised that it could lead to death. Almost equal numbers said
that they would take a child with diarrhoea to hospital, as said they would take a child
to a traditional healer. About three quarters of the mothers said they would continue
breastfeeding during diarrhoea and an even larger number said they would continue giving
other foods. Twenty-one per cent of the mothers said they would restrict fluids during
diarrhoea, and almost all of these were from the tribe who described the condition as
'enemy number one'. Nearly all mothers had heard of oral rehydration therapy (ORT) for diarrhoeal disease.
Over 80 per cent had seen it used in MCH clinics and almost 80 per cent had actually used
it themselves. Despite this widespread general knowledge about ORT, very few knew about
ORT in any detail. Relatively few could prepare a solution correctly with sugar and salt,
and the majority made it too concentrated. When asked how they would give OR fluid, many
mothers said 'three teaspoonfuls three times a day', and 22 per cent said that ORT
'prevents diarrhoea', implying that they did not understand the basic principles of the
therapy. After their children had discussed the topics with them, many mothers were able to
point out the features of dehydration much more accurately. The number who recognised
reduction in urine and a dry mouth as important signs of dehydration doubled. The number
who knew a sunken fontanelle and sunken eyes to be signs of dehydration also increased,
from 71 and 81 per cent respectively, to virtually all mothers. Over 40 per cent of
mothers showed improved understanding of the role of ORT in treatment, and, most
important, the number who could make up a correct solution increased from 13 to 65 per
cent. (Unfortunately this still leaves 35 per cent who could not make up a safe and
satisfactory solution.) Schools for health education In many countries there are far more primary schools than there are health facilities.
For example, in the Kilimanjaro region of Tanzania, with a population of 1.2 million,
there are only 189 health facilities but 703 primary schools. In the Kisumu district of
Kenya the ratio is even more striking, with only 16 health facilities and 295 primary
schools. If health messages, for example about the effective use of ORT, are to reach
homes in such circumstances, schools and school children are an important resource. Dr Mark E. Swai, KCMC Hospital, P. 0. Box 3010, Moshi, Tanzania.
|
A diarrhoea game
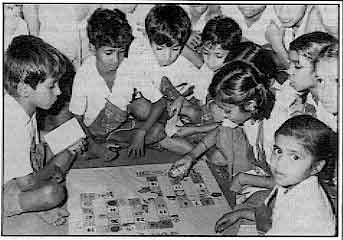 |
Learning
is more agreeable, interesting, effective and lasting for school children when it is done
through games. With this in mind, a health education game on diarrhoea has been developed
for school children in Bombay. The game is played on a board. Any number of children can
play. |
Each child throws the dice in turn. If they land on a good health habits square, they
can move again, for 'bad' practices, the player has to move back. The first person to
reach the final square 'healthy home' is the winner. The children enjoy the game very
much.
This game was designed to teach and encourage school children to concern themselves
with their health and that of their younger brothers and sisters. The children learn
simple preventive and promotive health measures appropriate for their communities.
They pass on what they learn to other children and to their families. In the game causes
of diarrhoea, symptoms, signs, treatment and advice are covered in simple
rhymes.
Dr Daksha D Pandit and Dr N P Pai, Preventive and Social Medicine Dept,
Topiwala National Medical College, Bombay 400 008, India.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue 29 June 1987  7 Page 8 7 Page 8
Oral rehydration and the medical profession Oral rehydration therapy (ORT) has gained wide acceptance in the Third World, thanks to
the massive promotional support given by the international agencies like WHO and UNICEF.
The paediatric professionals in developing countries are believed to have rallied round
the ORT bandwagon to promote its acceptance. Unfortunately, certain disturbing signs have
either not been perceived or are considered too trivial to warrant remedial measures. In India, medical students learn pharmacology and therapeutics at the beginning of
their clinical studies. What they learn will certainly influence their attitudes to
management of diseases. One of the most popular Indian text books 'Pharmacology and
Therapeutics' discusses scientific management of diarrhoea thus: 'symptomatic and
supportive therapy includes control of diarrhoea with anti-diarrhoeal agents and
correction of dehydration and electrolyte disturbances. The latter is the most important
aspect of treatment in severe diarrhoea'. However, the book next presents an
elaborate discussion of the drugs used in the symptomatic treatment of diarrhoea under
three headings. (1) Gastrointestinal protectives and adsorbants, (2) Drugs affecting
intestinal motility and (3) Miscellaneous agents. Nearly three pages are devoted to a fairly thorough discussion on the use of bismuth,
prepared chalk, light kaolin, pectin, activated wood charcoal, codeine,
diphenoxylate,
loperamide and lactobacillus acidophilus. There is not a word on oral rehydration in the
chapter on diarrhoea. One cannot help feeling that thousands of medical students in India
start with their 'basics' wrong in the management of diarrhoea. More shocking however is the professional practice of the paediatricians. I made a
critical evaluation of the management of diarrhoea in a leading teaching hospital of our
country, where over 2,000 children are admitted annually for diarrhoea. A survey of a
hundred randomly selected case records revealed the following practices. Most of the
children admitted had only mild or moderate dehydration. The majority of children with
mild or moderate dehydration received intravenous fluids on admission. Oral rehydration
solution was given as a supplement to IV fluids. Almost all children (92 per cent), with
acute or chronic diarrhoeas, received a combination of pectin and kaolin. No child with
vomiting ever escaped an antiemetic preparation like promethazine. Stool tests were
restricted at best to an occasional microscopic examination; stool cultures were seldom
sought. Case records abound with combinations like ampicillin, metronidazole,
gentamicin,
etc. Oral preparations of lactobacillus acidophilus were frequently administered to
children with all types of diarrhoea. What is most disturbing is that the institution is a leading centre of both
undergraduate and postgraduate training in paediatrics. The senior members of the faculty
have all been exposed many times to the modern trends of management of diarrhoeas and in
turn are vocal exponents of oral rehydration therapy and rational management of diarrhoea.
Somehow, at the moment of reckoning, old habits prevail over new concepts. I have no
reason to believe that the example is an isolated one, peculiar to India. It is not
unusual to overhear young trainee paediatricians saying that 'ORT' is good public
relations, while IV is excellent private management. Unless paediatric professionals in
the Third World change their practices, the whole concept of rational management of
diarrhoea and ORT may lose popular appeal. Third World mothers will place more faith in
what doctors practice, than in what they preach. Dr C R Soman; Professor of Nutrition, Medical College, Trivandrum, India.
|
News about DD
- Tamil edition . . .
The Rural Unit for Health and Social Affairs at
the Christian Medical College in India has produced a Tamil translation of="dd19.htm">issue 19 of Dialogue on Diarrhoea. Issue 19 focused
on ORT and readers who would like to obtain copies in the Tamil language should write to Dr
R Abel, RUHSA, Christian Medical College and Hospital, P.O. Box 632209, North Arcot
District, Tamil Nadu, India.
- Poster competition . . .
On="#page7">page 7 of this
issue we describe the important role which children can play in educating their parents
and brothers and sisters about better management of diarrhoeal diseases. Following this
theme, the Editors are pleased to announce a poster competition for children. Prizes will
be given for the best entries, and children can enter individually or as a school. We hope
that teachers will find this project a helpful way of getting children to think about
better health practices. For further details about the competition and how to enter,
please see the form enclosed in this issue.
- In the next issue . . .
In many countries women are responsible for
fetching, carrying and storing water for family use. Hygiene and sanitation practices are
also largely dependent on women. DD 30 returns o the
theme of water and sanitation, focusing in particular on the role of women.
|
Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 29 June 1987
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
|