|
| |
Issue no. 53 - June-August 1993
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 53 -
June-August 1993
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 53 June-August
1993  Page 1 2
Page 1 2
Eat your way to health
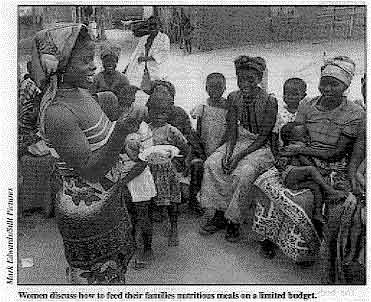 |
Women discuss how to feed their families nutritious meals on a
limited budget. Food is a key to health. A good and varied diet
gives us energy, helps us to grow, and enables us to fight off infections such as
diarrhoea. This issue of DD looks at the nutrients needed by our bodies and
explains how we can get them in everyday, inexpensive food.
|
We stress the importance of continuing to feed children who have diarrhoea. It used to
be wrongly thought that it was best to 'rest the bowel' during diarrhoea by stopping
eating. We now know that this is dangerous. Food is essential to repair damage to the bowel, speed recovery and build up children's
strength to fight off future episodes of diarrhoea. Unless a child with diarrhoea eats
well, he or she can easily become malnourished. Diarrhoea and malnutrition become a
vicious circle: malnourished children are more likely than well-fed children to die as a
result of diarrhoea. Special attention to diet is required in cases of persistent
diarrhoea. DD offers practical advice on feeding during diarrhoea. Breastfeeding is the best way to ensure that infants get off to a good start. In this
issue, DD provides answers to a common reason mothers give for stopping
exclusive breastfeeding - the worry that they cannot produce enough milk. We explain how
health workers can find out if a baby is getting enough milk, and if not, how to help the
mother solve the problem. Reassuring the mother that she can produce enough milk for her
baby is crucial. This issue also carries news about an important ingredient in our diet - vitamin A. It
has been shown to reduce the severity of, and danger from, diarrhoea. We report on studies
where deaths from diarrhoea of children in communities where vitamin A deficiency is a
problem decreased significantly after supplementation with vitamin A.
A big question facing health planners is: how can we get vitamin A to children during
their critical years of development. Fortunately, in most parts of the world, food rich in
vitamin A is readily available. DD describes good food sources. Some agencies would like to save children's lives as quickly as possible through
vitamin A supplementation programmes. Others recognise that the slower and more difficult
task of changing people's eating habits is likely to be more effective and sustainable. In
some countries, the two approaches can be tried: supplementation to save lives in the
immediate future, together with longer term nutrition education to improve people's diets.
Ultimately a community must eat its way to good health, and not rely on the distribution
of 'magic' capsules. William Cutting and Katherine Elliott
|
In this issue:
- How to plan a good mixed meal Page 3
- Vitamin A and child survival Pages
6-7
- New cholera strain in Asia Page 8
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 53 June-August
1993  1 Page 2 3 1 Page 2 3
An introduction to nutrition Felicity Savage and Ann Burgessdescribe the nutrients our bodies need to stay healthy, and which foods we can get
them from. Nutrients are the part of food that the body
uses to:
- build and repair tissues
- produce energy to 'fuel' growth and movement, and to keep warm
- protect itself from infections.
Almost all foods contain a mixture of nutrients. The following is a summary of the main
nutrients. Carbohydrates
The body uses carbohydrates mainly as 'fuel' for energy. Carbohydrates are either
sugars or starches.
 |
There are two
main types of sugars. Simple sugars (e. g. glucose and fructose found in
ripe fruit and honey) can be easily used by the body's cells. Complex sugars (e. g.lactose and sucrose found in milk and refined or cane sugar) need to be broken down
during digestion into simple sugars for the body to use. |
Starch is broken down into glucose during digestion. Starch is present in
cereals (such as rice, maize, and wheat); starchy roots (such as cassava, yams and
potatoes): and starchy fruit (such as plantain). Fat Fat is the most concentrated source of energy. It is an important energy store in the
body - if we eat more food than we need, the body changes it into storage fat.
| Fat is also needed for
other processes such as building cells and helping the body to absorb vitamin A. Good
sources: fats and oils (such as maize oil, palm oil, coconut oil, margarine, butter,
ghee, cooking fat): fatty animal foods (such as meat, fatty fish. milk and cheese); and
fatty vegetable foods (such as groundnuts and soya beans). |
 |
Proteins Protein is the most important nutrient for building body cells. It is especially
important for growing children and pregnant and breastfeeding women.
 |
The body cannot
store extra protein. When a person does not eat enough, the tissue from their muscles
breaks down to provide protein for important purposes such as fighting infections or
producing breastmilk. Good sources: meat, fish. eggs, milk (including
breastmilk), groundnuts and
beans. Cereals such as rice, wheat and millet contain less protein, but if eaten with
pulses (also known as legumes) such as lentils or beans they can be a good source of
protein.
|
Carbohydrates, fats and. to a lesser extent, protein all provide energy. We need more
energy when we are physically active. Energy needs also increase when we have infections
or are recovering from illness, or during pregnancy and lactation. Micronutrients These are vitamins and minerals which the body needs in very small amounts to function
well.
|
The most
important vitamins are: VITAMIN A - to reduce the severity of infections, keep the eyes healthy, and to
help children grow properly. (For good sources see="#page7">page 7.)
THE B VITAMINS - Thiamine, riboflavin and niacin help the body to 'burn'
nutrients to release energy. Good sources: meat, poultry, fish,
liver, wholegrain cereals, peas, beans, nuts, oil seeds, milk and eggs.
|
 |
- Folate helps the body to grow and make healthy red blood cells. Women need
more folate than men because they lose blood during menstruation. Pregnant women, mothers
who have recently given birth, and people with sickle cell disease also require increased
folate. Almost all foods contain some folate. Good sources: liver
and kidney, fresh vegetables (particularly dark green leaves), fish, beans and groundnuts.
Folate is destroyed when foods are stored or cooked for a long time. VITAMIN C - helps the body to use calcium and other nutrients to build bones and
blood vessels. It also increases the body's ability to absorb iron from non-meat or fish
sources, and to fight infections. Good sources: fresh or lightly cooked vegetables,
fresh fruit such as oranges, mangoes and pawpaw (papaya), apples, fresh milk and
breastmilk.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 53 June-August
1993  2 Page 3 4 2 Page 3 4
VITAMIN D - helps the body to absorb and use calcium and phosphorous to
build healthy bones and teeth. When the sun shines on the skin, a chemical reaction makes
vitamin D. The best way to get enough is to go outside with your face and arms uncovered
for at least 10 minutes most days. Even if it is cloudy, there is enough light for
production of vitamin D. The following minerals are important: IRON - to make haemoglobin for red blood cells. Good sources: meat,
fish and breastmilk. Liver, kidney, spleen and heart are especially rich in iron. There is
a useful amount of iron in beans, peas, nuts and cereals, but it is more difficult to
absorb in this form. IODINE - is used by the thyroid gland to produce hormones that regulate the way
the body uses energy and keeps warm. The hormones are also important to the functioning of
the brain and nervous system. Good sources: fish. seafood and iodised salt. Iodine
is also transferred to vegetables grown in iodine-rich soil. Iodine deficiency is common
in mountainous areas far from the sea and places where there are frequent floods, because
iodine is washed from the soil. CALCIUM - needed to build and maintain bones and teeth. Pregnant and
breastfeeding women, growing children, and older women need extra calcium. Good
sources: milk (including breastmilk), small fish with edible bones, beans and peas,
finger millet and dark green leaves. ZINC - helps the body to fight infections and enables it to grow and develop
normally. Good sources: meat, chicken, fish, wholegrain cereals and pulses (nuts,
beans, peas and lentils) and breastmilk. Water Adults need 2-3 litres of water a day. Extra water is needed to replace fluid lost
during diarrhoea or during sweating or fever. Breastmilk contains plenty of water, so
babies less than six months old who are exclusively breastfed do not need to drink water
or other fluids. Source: Savage King, F and Burgess, A, 1993. Nutrition for Developing Countries.
Oxford University Press. (Adapted by permission of Oxford University Press.) The new second edition is available to readers in developing countries for £3.95.
Write to: Oxford University Press, Saxon Way West, Corby, NN18 9ES, UK. Refer to the ELBS
(Educational Low-Priced Books Scheme). Planning good mixed meals Families do not need to have a lot of
money to eat well. It is much better to plan nutritious meals than to buy unnecessary
vitamin tablets.
|
Most
meals are based on cereal staples (such as rice, maize or millet porridge, or bread), or
starchy vegetable staples (such as boiled cassava or yams). These staples are usually not
expensive, and provide most of the energy in a meal. Cereal staples also contain
fibre,
vitamins, and some protein (but not complete protein). Starchy staples such as cassava do
not provide protein. Neither cereal nor vegetable staples provide the complete range of
vitamins and minerals needed by the body. It is important to eat other foods with the staple to provide these extra nutrients. If
served with the staple (for example in a sauce) other foods can provide missing nutrients
and make the meal tastier. Some additional foods such as fruit can be eaten immediately
after the main meal.
|
 |
The picture above shows some key foods which can be added. The most important thing is
to try to include a mixture of foods from the kinds of nutritious food described in the
introduction.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 53 June-August
1993  3 Page 4 5 3 Page 4 5
Feeding during diarrhoea How to break the cycle of diarrhoea and malnutrition. Deaths from diarrhoea are often
associated with malnutrition. The two conditions form a vicious circle, each making the
other worse. Diarrhoea is a major cause of malnutrition.
This is because the body needs more nutrients than normal to cope with infections such as
diarrhoea, yet children with diarrhoea usually eat less. Also, the ability of the body to
absorb nutrients is reduced during diarrhoea. Nutrient intake may decline by as much as a third during the first days of diarrhoea.
There are several reasons for this: loss of appetite; vomiting, which may discourage
mothers from giving food; or mothers feeding children less or giving diluted food based on
traditional beliefs or on incorrect recommendations to 'rest the bowel'. In addition, absorption of nutrients may also be reduced by as much as a third during
acute diarrhoea. However, even though some nutrients are lost, most nutrients continue to
be absorbed, so it is important to continue feeding children who have diarrhoea. Malnutrition can make diarrhoea worse.
Malnourished children tend to have longer and more severe episodes of acute diarrhoea than
well-nourished children. The cycle of malnutrition and diarrhoea can be broken by good
nutrition. Health workers should stress to parents the importance of feeding children well
and provide practical advice on healthy food. If children do get diarrhoea, good nutrition must be maintained both during and
after the illness.
This can be done by continuing to give generous amounts of nutritious food. If dehydration
develops, feeding (other than breastfeeding) should be stopped for a few hours while oral
rehydration therapy is given. Feeding should be resumed as soon as rehydration is
completed (usually within 4-6 hours). In general, the same foods should be given during
diarrhoea as those a child eats when he or she is well. If children are severely malnourished they should be given food as soon as possible
during the rehydration period. Such children also should be
rehydrated more slowly (over 12-24 hours) and given potassium-rich foods such as spinach,
avocado pears, bananas and coconut water. The recovery period is particularly important. Even when a child is given as much food
as possible during diarrhoea, growth will slow down, and this must be caught up. After an
illness children are often very hungry and may eat up to twice as much as usual. A useful
approach is to give the child as much as he or she can eat, and provide an extra meal
every day for two weeks. Milk for infants Breastfeeding should never be reduced or stopped during diarrhoea. Infants with
diarrhoea should be breastfed as often and for as long as they want. If infants are usually given animal or formula milk, this should be continued during
acute diarrhoea (diarrhoea that lasts less than 14 days). It used to be thought that it
was best to dilute animal or formula milk during the first two days of diarrhoea,
especially for young infants. However, recent studies in Guatemala and Brazil show that
this has no benefit and can be harmful because it results in less nutrient intake and
poorer growth (1). Older children If an infant is aged four months or older and is already taking soft or solid foods,
these should continue to be given during diarrhoea. Infants six months or older should be
started on soft foods if they are not already being given them. At least half the dietary
energy of children over six months old should come from foods other than milk. If dehydration develops, feeding should be stopped for 4-6 hours during rehydration,
and then resumed. Home fluids such as soup are important in preventing dehydration.
However home fluids are not a substitute for food. They do not provide enough calories or
nutrients on their own. During and after diarrhoea, children should be given small meals frequently (e. g. six
or more times per day) and actively encouraged to eat. The following are useful
guidelines:
- Use well-cooked local staple foods that can be easily digested, such as rice, corn,
sorghum, potatoes or noodles.
- Give the staple food in a soft, mashed form. For infants, use a thick porridge or
semi-liquid pulp.
- Increase the energy content of the staple food by adding 1-2 teaspoonfuls of vegetable
oil per serving. Red palm oil is especially good because it is also a rich source of
vitamin A (see="#page7">page 7).
- Mix the staple food with well-cooked pulses (beans, peas, nuts or lentils) and
vegetables. If possible, include eggs, meat or fish.
- Give foods rich in potassium (see="#potassium">above) to replace potassium
lost during diarrhoea.
- Avoid drinks with a high concentration of sugar (e. g. sweetened commercial fruit
drinks, fizzy drinks). These can make diarrhoea worse and increase the risk of
dehydration.
Source: WHO. 1992. Readings on Diarrhoea: Student manual. (Available from CDD/WHO,
CH-1211 Geneva 27. Switzerland. Price for readers in developing countries: Sw. fr 14.) 1. Chew, F; et al., 1993. Is dilution of cows' milk
formula necessary for dietary management of acute diarrhoea in infants aged less than 6
months? Lancet 341: 194-7.
|
Persistent diarrhoea
Good nutrition is especially important in cases of persistent diarrhoea (diarrhoea that
lasts 14 days or more). Persistent diarrhoea may cause dramatic weight loss and a
deficiency of key micronutrients. The guidelines (see="#page4">above) for
feeding during acute diarrhoea should be followed, with these additions or exceptions:
- Special hospital care
Children who are under six months old or are dehydrated should be rehydrated and referred
to hospital. They may need treatment to maintain hydration and to be given special diets.
- Children over six months old
If children are normally fed with animal milk, mothers should be advised to give only half
the usual amount, or to replace it with a fermented milk product such as yoghurt. In many
cases this will cause the diarrhoea to reduce rapidly. Once the diarrhoea has stopped, the
reduced amount of animal milk, or the fermented milk, should be given for another week,
then the usual milk should gradually be reintroduced over several days.
- Micronutrient supplements
Supplementary vitamins and minerals should be given for at least four weeks. The most
important micronutrients for children with persistent diarrhoea are: folate, vitamin B12,
vitamin A, zinc and iron. Supplements can be given in the form of multivitamin tablets or
syrup.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 53 June-August
1993  4 Page 5 6 4 Page 5 6
'I do not have enough milk.'
Felicity Savage addresses a common concern of mothers
experiencing problems with breastfeeding. Giving a baby breastmilk only (called exclusive
breastfeeding) is the best way to feed a baby for the first 4-6 months. In many countries,
nearly all mothers successfully breastfeed. However, some mothers experience problems
which lead them to give supplementary foods or fluids before these are needed, or to stop
breastfeeding altogether. The belief that they cannot produce enough milk is one of the commonest reasons that
mothers give for starting supplements early. Yet almost all mothers, even those who are
moderately malnourished, can produce enough milk. IS THE BABY GETTING ENOUGH MILK? Health workers first need to find out whether the baby is taking enough
breastmilk. The wetness test - If a breastfed baby who is not given other fluids urinates at
least six times in 24 hours, then it is almost certainly taking enough
breastmilk. The weight check - In the first six months of life a healthy baby should gain at
least 125g each week, or 500g a month. If a breastfed baby gains much less than this, it
is either ill or is not getting enough milk. If you think a baby might be ill, diagnose
and treat the illness, or refer the baby to a more specialised health worker. If the baby is getting enough milk, you should reassure the mother that the baby is
growing well and encourage her to continue breastfeeding. IF THE BABY IS NOT GETTING ENOUGH MILK There are several possible reasons why a baby may not be getting enough
breastmilk.
Most of these can be detected and overcome if a health worker asks the right questions,
observes the mother when she breastfeeds, and gives the mother appropriate help.
- The baby is not suckling effectively
Sometimes a baby does not take enough of the breast into its mouth, sucking the nipple
only. This means the baby is not getting the milk out of the breast efficiently. The baby
may want to feed very often, or for a long time at each feed, or it may become frustrated
and refuse to feed. If the baby continues to breastfeed in this position, it may make its
mother's nipples sore and cracked.
ACTION: The baby should take a big mouthful of the breast tissue as well as the nipple.
Explain the importance of this to the mother and help her to make sure the baby takes
enough of the breast into its mouth.
- The mother does not breastfeed the baby often enough
Breastfeeding less than 5-6 times a day is also a common reason why a baby may not get
enough milk. Some mothers who are very busy find it difficult to respond to their babies'
demands for feeding. But the baby's suckling action stimulates the production of milk, so
if the number or length of breastfeeds is reduced, less milk is produced. Mothers should
allow babies to breastfeed as often and for as long as they want.
ACTION: Discuss with the mother how she can breastfeed more frequently.
If she breastfeeds more often for a few days, including during the night, her milk supply
will increase. A mother who works away from home needs special advice. Perhaps she can
take her baby to her workplace, or ask a helper to bring the baby to her to be breastfed.
If this is not possible, she could feed her baby more at night and express her milk to be
given to the baby while she is away. (See="dd41.htm">DD41.)
- The baby does not suckle for long enough
Sometimes mothers take their babies off their breasts after a short time, before their
babies are satisfied. Some babies are slow feeders and take 30 minutes or more before they
get enough milk. Other babies suckle for only a few seconds and then fall asleep. After a
short time they may wake up crying because they are hungry again.
ACTION: Advise the mother to let her baby continue breastfeeding until it stops
suckling. If the baby goes to sleep the mother should stroke its cheek gently to wake it
up.
(Make sure that the baby is not overwrapped. A baby that is too warm is more likely to
fall asleep.)
- Supplements are being given
Supplements (e. g. milk formula, cow's milk, cereal, juice, teas, and even water) fill the
baby's stomach causing it to suckle less at the breast, therefore decreasing the mother's
milk supply.
ACTION: Advise mothers against giving supplements until the baby is at least four months
old.
Source: Savage King, E 1992. Helping Mothers to Breastfeed. African Medical and
Research Foundation, Kenya. Correction to positioning in breastfeeding twins picture DD51 contained pictures of a mother breastfeeding twins.
|
In one of the pictures, however, the positioning of the babies was not good
(see left). The babies' heads were turned away from their bodies, a position which makes
it difficult for a baby to get the breastmilk out of the breast. Poor positioning is also
a common cause of sore nipples. |
|
We asked our artist to redraw the picture (see left). Here, the babies look
comfortable, with their heads and bodies facing the mother. |
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 53 June-August
1993  5 Page 6 7 5 Page 6 7
Vitamin A and children's health
Children who eat enough vitamin A are more likely to survive an episode of
diarrhoea. However, planners are still debating the best ways of improving vitamin A
intake. Not enough vitamin A in their diet is a serious
health problem for millions of children worldwide. It has been known for years that
vitamin A deficiency damages the eye, but it has only recently been shown that it is also
linked with deaths from diarrhoea. In the last ten years, a number of studies have looked at the role of vitamin A in
increasing children's resistance to infection, and in helping them to recover from
illnesses such as diarrhoea, measles and acute respiratory-infections. These studies have
looked at the effect of providing vitamin A supplements to children in populations where
there is vitamin A deficiency. There is now clear evidence that vitamin A supplementation reduces mortality in
populations where vitamin A deficiency is a public health problem. A recent meta-analysis
(statistically combining the results of several studies) found that vitamin A
supplementation decreased mortality of children aged six months to five years by an
average of 23 per cent (1). Most of the studies involved giving high dosage capsules (200,000 international units
[IU]; with the majority reducing the dosage for infants under 12 months old to 100,000
IU)
at 3-6 monthly intervals. In one study, vitamin A was added to monosodium glutamate which
was eaten daily. In another, vitamin A capsules were given weekly. Weekly dosing and
adding vitamin A to commonly used food were found to be just as effective as giving high
dosage capsules. Most of the reduction in mortality came from a decrease in deaths due to diarrhoeal
diseases and measles. The effect of vitamin A supplementation on mortality from acute
respiratory infection was not clear. Vitamin A supplementation did not reduce the incidence or duration of diarrhoea or
respiratory infections. But it did appear to reduce the severity of diarrhoea and measles.
The author of the meta-analysis concludes that 'vitamin A status appears to affect the
child's ability to respond appropriately and adequately once infection has developed'.
 |
Vitamin A supplements can save lives,
but changing people's diets is more effective in the long term. |
Further research Because there are no clearly established safe limits for high dosages of vitamin A in
children under six months, the effect of high dosages on these younger infants is now
being investigated. The studies so far have taken place in populations where some children had signs of
vitamin A deficiency (e. g. eye problems associated with lack of vitamin A). There is a
need for studies in populations where there is biochemical vitamin A deficiency without
clinical signs. There are three main ways that vitamin A deficiency could be tackled.
- Improving people's diets
In many communities with vitamin A deficiency, vitamin A-rich foods are available (see
page 7), but because of cultural taboos some of these foods such as
eggs or mangoes may not be given to children who need them most. Also, some vitamin A-rich
foods such as mangoes are seasonal; however, with good preservation methods (solar drying
or preservation in sugar), mangoes can be eaten all year round. Small quantities of oil in
food can increase absorption of vitamin A.
With the right advice and encouragement most families can improve their children's vitamin
A intake without relying on outside interventions. Education and information campaigns,
involving community members, mothers, nutritionists, farmers, teachers and health workers,
are needed.
- Fortification
adding vitamin A to a commonly used food in the same way that iodine is added to salt
in many countries. This depends on a common food being produced centrally so it can be
fortified. It might be possible in some countries in Asia using monosodium glutamate, but
in many African countries no suitable product has been identified.
- Supplementation
giving vitamin A capsules to children in high risk population groups. There are
various ways this could be done:
- Treatment basis Capsules could be given to children who come to health centres or
hospitals with measles. There is also a strong case for giving supplements to children
with persistent diarrhoea, although this could involve a risk of too frequent dosing.
- Targeting children in greatest need This is more difficult. Needy children are
often the hardest to reach, e. g. they are in remote areas or are not in contact with the
health system. There would also be problems with choosing individuals to receive vitamin A
supplements while other children in the same community missed out. It would be better to
supplement all children in vulnerable communities.
- Mass distribution of capsules Studies are being carried out into giving vitamin A
supplements through immunisation programmes. However, the age group for immunisation,
usually infants under nine months, is not the time of greatest risk of vitamin A
deficiency or diarrhoea because these infants are usually being breastfed*.
Also, immunisation programmes do not always reach children who are most in need. An
alternative would be to give out capsules at 4-6 month intervals at health centres.
However this would only reach children who attend health centres and it would demand very
good record keeping to ensure that children did not receive possibly harmful extra doses.
Other approaches which have been suggested but not tested include distributing vitamin A
capsules to mothers during immunisation programmes for them to give to older children, and
involving communities in 'vitamin A days' three times a year.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 53 June-August
1993  6 Page 7 8 6 Page 7 8
Sustainable solutions Supplementation has been described as a 'temptingly convenient way of tackling the
issue, but not sustainable' (2). Distributing vitamin capsules may show
an effect on mortality within a short period of time and could appeal to those who measure
success mainly on the basis of reaching numerical targets. However, dietary change is more
effective in the long term. It may take longer to achieve than supplementation, but will
be more sustainable and more cost-effective. It is also important to work on raising
people's incomes in order to improve their diets. In the short term, some countries may decide to use two approaches: supplementation to
save lives within a few months, while at the same time working on improving people's
diets. It is important that adequate resources are set aside for nutrition education, and
are not all used up in short term supplementation. 1. Beaton, G H, et al., 1992. Effectiveness of Vitamin A
Supplementation in the Control of Young Child Morbidity and Mortality in Developing
Countries. University of Toronto.
2. Tapang, H, 1992. Ghana Uses Vitamin A To Fight Child Deaths.
Panos / Namibia New Era, 14-20 January I992.
A full list of references for the studies is available from AHRTAG. *Breastmilk is one of the best sources of Vitamin A. Even a mother
whose Vitamin A status is not good can produce enough vitamin A in her breastmilk for her
child's needs. Further source of information IVACG (International Vitamin A Consultative Group), The
Nutrition Foundation. 1126 Sixteenth Street, NW, Washington, DC 20036. USA.
|
Good food sources of vitamin A There are two forms of vitamin A in food.
- RETINOL found in animal products is the best form of vitamin A. Good sources are
breastmilk, animal milk, liver, kidney, eggs, butter and ghee.
- CAROTENE found mainly in orange, yellow and green vegetables and fruits destroys
harmful chemicals (called free radicals) produced during infection. When we eat carotene,
most of it is changed to retinol. Six molecules of carotene make one molecule of
retinol.
Good sources are red palm oil; orange and yellow fruits and vegetables such as mangoes,
pawpaw, pumpkin, carrots, maize, yellow sweet potatoes and bananas; and dark green and
medium green leaves such as spinach, amaranthus, kale, the leaves of cassava, cowpeas,
sweet potatoes and beans.
 |
We store vitamin A in our livers. If we eat a lot of vitamin A at one time (e. g.
during the mango season) our livers can store enough vitamin A to last several months.
Vitamin A is said to be 'stable'. This means that not a lot of the vitamin is lost through
moderate cooking processes. However, some vitamin A is lost through deep frying, sustained
boiling until the vegetable or fruit disintegrates, and through sun drying. |
|
|
Action on improving diets Food rich in vitamin A can be grown on
farms, in urban backyards, tiny garden plots, and even on window ledges. In September 1991, the UN Food and Agriculture Organization started a programme in
Zambia's Luapula valley to tackle chronic vitamin A deficiency. Two main strategies were
identified: increasing the growing of vitamin A-rich vegetables, fruits, and nuts; and
educating local people on the link between nutrition and eye disease. Sixteen demonstration plots growing vegetables rich in vitamin A were established,
including some at primary schools. Tree nurseries were planted to produce fruit tree and
oil palm seedlings to supply farmers. There are now plans for a seed 'bank' to provide
vegetable seeds for community use. Nutrition information was introduced into the training of primary school teachers,
agricultural workers and community development workers. Training stressed improving
people's all-round nutrition, since people who are deficient in vitamin A usually lack
other nutrients as well. The information campaign emphasised improving the nutrition of
pregnant and lactating women and pre-school children. Women's organisations, schools and
the mass media were all involved in spreading information. A year after the project started, there was already much more Vitamin A-rich food being
grown in the valley and many more families were aware of the connection between diet and
blindness. Source: Madeley, J. 1992. Preventing blindness in Zambia. World Health, Nov-Dec
1992.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 53 June-August
1993  7 Page 8 7 Page 8
New strain of cholera reported Tens of thousands of cases of cholera caused by a previously unknown organism have
recently been reported in medical journals in India and Bangladesh. The new strain is an important
development in the history of the disease. Until now, Vibrio cholerae O1 was the
only organism causing cholera epidemics. The symptoms and treatment of cholera caused by the new strain (designated V.
cholerae O139) are largely the same as for 'normal' cholera. Severe, watery
diarrhoea causing rapid dehydration is the main sign. The first line of treatment is
rehydration, followed by administration of an antibiotic in patients with severe
dehydration. Tetracycline, the antibiotic of choice for most adults with cholera, has so
far been effective against V. cholerae O139. It appears that the routes of transmission of V. cholerae O139 are the
same as for the O1 vibrio. Contamination of water, food and hands are presumed to be the
main ways it is spread. Prevention measures should therefore be identical. Unlike other cholera epidemics in Asia, V. cholerae O139 affects
an unusually high proportion of adults. This is because while many adults in areas where
there have been V. cholerae O1 epidemics have developed some
immunity to this strain, they lack immunity to the new O139 vibrio. Health planners are concerned that the new strain, which has so far only appeared in
southern Asia, may spread to other areas just like Vibrio cholerae O1 has done -
starting in Asia in 1961, then spreading to the Middle East and Africa by 1970. Even though WHO advises that vaccination against 'normal' cholera is ineffective, some
countries still promote the vaccine. The existing vaccine will not protect at all against
the new organism, therefore vaccination will be totally ineffective as a means of
prevention. Health workers should redouble their efforts to prevent cholera, and should be on the
alert to provide quick and effective treatment. Sources: Ramamurthy, T: et al., 1993. Emergence of novel strain of Vibrio cholerae with
epidemic potential in southern and eastern India. Lancet 341:703-4.
Albert, M J, et al., 1993. Large outbreak of clinical cholera due to vibrio
cholerae non-O1 in Bangladesh. Lancet 341:704.
WHO, 1993. Epidemic diarrhoea due to Vibrio cholerae non-O1. Weekly Epidemiological
Record. 68 No. 20: 141-2. Write to AHRTAG for a copy of the cholera treatment chart in="dd52.htm">DD52. NGO nutrition strategies
The International Conference on Nutrition organised by WHO and the Food and Agriculture
Organization (FAO) in December 1992 set up a non-government organisation working group on
nutrition. Its purpose is to prepare guidelines on effective nutrition strategies. The working group is seeking information from NGOs about:
- nutrition problems which need to be addressed
- ideas for possible solutions
- nutrition activities being undertaken
- effective educational material.
If you have experience of working at NGO level on nutrition activities, the group would
like to find out your views. Write to: The convener of the NGO working group on nutrition, Mrs Joanna Koch, Alte
Landstrasse 89, 8802 Kilchberg, Switzerland. Breastfeeding resource list
 |
An
international resource list of organisations involved in promoting breastfeeding, with a
section on publications and audio-visual materials, will be available soon from AHRTAG. It
will be free to readers in developing countries.
Write to: AHRTAG, 1 London Bridge Street, London SE1 9SG, UK.
|
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Executive editor Kate O'Malley
Design & production Ingrid Emsden
Editorial advisory group
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Nicole Guérin (France)
Dr Norbert Hirschhorn (USA)
Dr Sharon Huttly (UK)
Dr Claudio Lanata (Peru)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Professor Dang Duc Trach (Vietnam)
Professor Andrew Tomkins (UK) With support from AID (USA), Charity Projects (UK),
Ministry of
Development Cooperation (Netherlands), ODA (UK),
SIDA (Sweden), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Turkish Medical Association (Turkey)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 53 June - August 1993
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
updated: 23 April, 2014
|