|
| |
Issue no. 25 - June 1986
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 25 - June
1986
|
DDOnline
Dialogue
on Diarrhoea Online Issue 25 June 1986  Page 1 2
Page 1 2
Drugs and bloody diarrhoea
Oral rehydration therapy (ORT) is the simplest and most important advance in the
treatment of dehydration due to diarrhoea. Dehydration probably accounts for at least 60
per cent of deaths from acute watery diarrhoea. Unfortunately there are other diarrhoeal
causes of death which are not so simple to treat. In this issue we focus on dysentery -
and the role of drugs, in addition to ORT, in the treatment of diarrhoeal disease. Dysentery: a major problem
Dysentery is diarrhoea with blood and pus in the stools. There are two main types; that
due to bacteria, bacillary dysentery, and that due to parasites, amoebic dysentery. In
recent years several major epidemics of bacillary dysentery caused by shigella organisms
have occurred, associated with high death rates (see="#page4">page 4).
Although dehydration was present in many of those who died, it was probably not the main
cause of death. Antibiotic drugs can be valuable in treating dysentery and this is
discussed on="#page5">page five of this issue. Amoebic dysentery is more
difficult to diagnose. Many people who live in conditions where environmental hygiene is
poor may have this parasite in their bowels, but relatively few show obvious clinical
signs of dysentery. It is now known that only certain types of amoeba cause illness in
man. Simple diagnosis
Can dysentery be diagnosed without access to a microbiological laboratory? In fresh
stools, blood can be seen by the naked eye in over 50 per cent of cases of shigella
dysentery and in about 40 per cent of cases of amoebic dysentery. (See="dd11.htm#page4">DD 11, page 4.) Blood is visible in less than 10 per
cent of the stools of patients with diarrhoea caused by other common organisms. (Stoll et
al. 1983. BMJ 286. 2037-40.) With a simple microscope it is often possible to
distinguish bacillary from amoebic dysentery. More than 50 white blood cells seen per high
power field is typical of a shigella infection. In amoebic dysentery, the amoebae
containing red blood corpuscles can often be seen moving about under the microscope. Drugs? Only when necessary
|
Rehydration: still the life-saving treatment in the majority
of cases of acute diarrhoea.
Man is a medicine taking animal and irrationally tends to believe that there must be
"a pill for every ill"; it is often difficult to convince people that the best
treatment for most diarrhoeas is a simple drink and not a drug. The major problems
associated with drugs for diarrhoea include:
- Inflated ideas about the efficacy of medicines. Doctors as well as patients often
wrongly believe that drug treatment is essential. Drugs are needed in only a few
conditions and some of these are discussed on="#page5">page 5.
|
 |
- Incorrect use of antibiotics. The commonest organisms which cause diarrhoeal disease are
either not susceptible to antibiotics, for example, rotavirus, or the antibiotics do more
harm than good, as in salmonella food poisoning. Indisciplined prescribing and
insufficient dosage worsen the problem of bacterial resistance to antibiotics.
- Inappropriate promotion and advertising of anti-diarrhoeal medicines perpetuates the
belief, in the minds of both the public and the health professionals, that a medicine is
the answer to the problem of diarrhoea.
- Insufficient supplies of drugs for the people who actually need them.
The use of drugs in diarrhoeal disease distracts both parents and health professionals
from the life-saving treatment for the majority of cases of acute diarrhoea - rehydration.
WAMC and KME
|
In this issue . . .
- Drug therapy
- Dysentery
- Care of medicines
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 25 June 1986  1 Page 2 3 1 Page 2 3
International Health Congress
The International Health Congress of the World Federation of Public Health Associations
will hold its fifth conference in Mexico City, on 22-27 March 1987. The theme of the
Congress is 'International Health in an Era of Economic Constraint: The Challenge'.
Abstracts must be submitted by 15 October 1986, in English or Spanish. For further
information please contact: WFPHA Secretariat, c/o American Public Health Association,
1015 15th Street, NW, Washington DC 20005, USA. Diagnostic needs: questionnaire
The Programme for Appropriate Technology in Health (PATH), is currently undertaking a
survey to identify the priority diagnostic procedures needed for patient care in
developing countries. The results will help to formulate research priorities, and to
define the most important characteristics for diagnostic tests. If you are interested in
taking part in the survey, please write for a questionnaire to: Vivien Davis Tsu,
Editor, Directions, PATH, Canal Place, 130 Nickerson Street, Seattle, WA 98109, USA.All survey participants will receive a report summarising the main results. Child Survival Action News
Child Survival Action News is a new quarterly newsletter aimed at promoting child
survival programmes in the developing world. The newsletter will focus on immunisation,
growth monitoring, birth spacing, maternal health, the promotion of breastfeeding, and
improved nutrition practices. For further information and sample copies, write to: Child
Survival, National Council for International Health, 1101 Connecticut Avenue, NW, Suite
605, Washington D.C. 20036, USA. ORT in practice
|
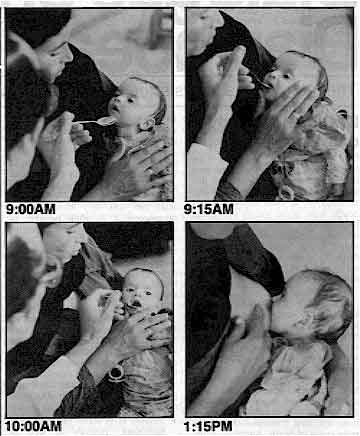
An Egyptian
infant - dehydrated from the effects of diarrhoea - is treated with life-saving oral
rehydration therapy (ORT). At 9:00am, the child's sunken fontanelle is a clear sign of
dehydration. Within hours, the child is out of danger; and is able to resume breastfeeding
by 1:15pm. National Control of Diarrhoeal Diseases Project (NCDDP), 20a Gamal el Din Abul
Mahassen St, Garden City, Cairo, Egypt.
|
 |
|
ORT literature The PRITECH Project (Technologies for Primary Health Care) produces a monthly
bibliographical listing, ORT Technical Literature Update. Each listing contains up to
eight annotated articles from the current literature on oral rehydration therapy and
related health issues. The focus is primarily technical, but future issues plan to include
operational and programme related literature. The articles are selected by the editors, Dr
Jon Rohde and Dr Robert Northrup, on the basis of possible interest to readers rather than
purely on scientific merit. For more information contact: Elizabeth Jennings,
Director, PRITECH Information Center, Suite 700, 1655 North Fort Myer Drive, Arlington,
Virginia 22209, USA.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 25 June 1986  2 Page 3 4 2 Page 3 4
|
DD subscriptions Due to rising costs and rapid expansion of the English mailing list, we are no longer
able to distribute DD everywhere free of charge. We are therefore asking all our
readers in North America and Western Europe, who can afford to do so, to make a small
contribution in the form of a subscription fee. $10.00 / £5.00 would cover the cost of
producing and distributing your copies of DD for one year. This obviously does not
apply to those who have already subscribed, or who are exempt for any reason - for
example, if you contribute to DD, or work for an agency which funds the newsletter
or distributes DD to health workers in developing countries. Cheques, bank drafts, or international money orders should be made payable to 'Dialogue
on Diarrhoea' (AHRTAG). Please make payments in £ sterling or US $ and write your
subscription number, if you have one, on the back of the cheque.
|
Directory of periodicals A Directory of Development Education Periodicals, containing information about
publications by international and national NGOs and United Nations organisations, is now
available free of charge to Third World NGOs, at $10.00 for other NGOs, and at $15.00 for
other organisations and individuals. Readers should write to: NGLS, United Nations
Office at Geneva, Palais des Nations, CH 1211 Geneva 10, Switzerland. Getting the message across
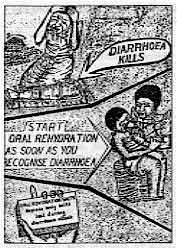 |
The
management of childhood diarrhoea is one of the major priorities in Uganda today, and ORT
is the main weapon being used. In order to help their efforts to educate rural mothers
about ORT, postgraduate students at the Institute of Public Health in Kampala designed
this poster during sessions on diarrhoeal disease management under the supervision of Dr G
Bukenya. The message is blunt and dramatic. It demonstrates that diarrhoea kills, but that the
child can be saved if ORT is started early. The poster will soon be field-tested in a
number of villages in Uganda. Dr Gilbert Bukenya, Department of Community Medicine, University of Papua New
Guinea, P. O. Box 5623, Boroko, Papua New Guinea.
|
Health care - a wider approach
In a future issue of DD the editors plan to focus on the implementation of
health care, particularly diarrhoeal disease control activities, through the work place
and community groups. Readers who would like to contribute to this feature are invited
to write to DD describing their experiences. The provision of health care for
plantation workers and their families is one example of this approach, to be discussed at
a one day meeting entitled 'Health and Health Services for Plantation Workers'. This
meeting will be held at the London School of Hygiene and Tropical Medicine on Thursday 4
September. For further information please contact Dr R Laing, Institute of Development
Studies, University of Sussex, Falmer, Brighton BN1 9RE, U.K. ORT in Saudi Arabia
|
A Saudi mother encouraging her child to drink oral rehydration
solution at the Quwazah Primary Health Care Centre in Jeddah.
Photo by Muneera Hamdan Al-Osemi
|
 |
In the next issue . . . .
DD 26 will focus on the effect of seasonality and social
factors on the incidence of diarrhoea. This issue will also contain an update of sources
of information and resource material for diarrhoeal disease. The Editors would like to thank all those readers who have filled in and returned their
DD questionnaires. Your comments and suggestions are much appreciated and will be
very helpful in planning content of future issues of DD. The results from the
analysis of the questionnaire will be published in DD later this year.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 25 June 1986  3 Page 4 5 3 Page 4 5
Still problems to resolve
Sudhir Pal reviews the global situation and findings
from the recent dysentery epidemic in West Bengal. Bacillary dysentery, characterised by frequent passage of blood and mucus in the
stools, and accompanied by excruciating abdominal pain, fever and intense weakness, has
long been recognised as the cause of many deaths during wars, famines and other disaster
situations. The disease occurs worldwide, but most frequently in countries where hygiene
and sanitation are poor. In these countries endemic shigellosis is a significant cause of
illness and death, particularly in young children. Cause and transmission
The infection is caused by bacteria of the genus Shigella; hence the name shigellosis
or bacillary dysentery. The shigella genus has four sub-groups: S dysenteriae, S.
flexneri, S. boydii, S. sonnei; and 39 serotypes. The most severe infections are
caused by the S. dysenteriae type 1 (also known as Shiga's bacillus),
which may occur in epidemics. Man is both the reservoir and natural host of Shigella. Infection is by the faecal-oral
route and is usually spread by person-to-person transmission. It takes only 10 to 100
shigella organisms to produce dysentery, a low infectious dose, whereas one million to ten
million organisms may need to be swallowed to cause cholera. During the late 1960s, Shiga's bacillus was responsible for a series of devastating
epidemics of dysentery in Latin America, Asia and Africa. In 1967 it was detected in the
Mexican-Guatemalan border area and spread into much of Central America. An estimated half
million cases, with 20,000 deaths, were reported in the region between 1967 and 1971. In
some villages the case fatality rate was as high as 15 per cent; delayed diagnosis and
incorrect treatment may have been responsible for this high death rate. One particularly
disturbing feature was the resistance of the bacteria to the most commonly used
antibacterial drugs: sulfonamides, tetracycline, chloramphenicol and streptomycin. Recent outbreaks
Serious epidemics due to the multiple-drug resistant S. shigae have
occurred recently in Bangladesh, Somalia, South India, Burma, Sri Lanka, Nepal, Bhutan,
Rwanda and Zaire. Each epidemic showed similar features: the disease spread rapidly in
spite of all available public health measures, attacking over 10 per cent of the
population and killing between two and ten per cent even of the hospitalised cases. West Bengal in India has always been an endemic area for bacillary dysentery. In 1984,
greater numbers of dysentery cases started occurring and spread rapidly throughout the
state. Investigations revealed that attack rates were high, especially among young
children, and that all the shigellae isolated from stool specimens were resistant to the
commonly used drugs. In response to the outbreak, control measures were initiated, newspapers, radio and
television carried information about the epidemic to raise public awareness; and district
level health personnel were alerted. Reports came in of increasing numbers of dysentery
cases, between two and three thousand new cases, and up to 150 deaths, a day. People began
to panic and doctors were frustrated by the ineffectiveness of conventional treatment . Resistance to antibiotics
The epidemic spread to Calcutta, where stool samples from 382 patients showed Shiga's
bacillus in 35 per cent of cases, and different species of shigella organisms in 52 per
cent. These organisms were sensitive to nalidixic acid (96.7 per cent), gentamicin (83 per
cent), furazolidone (77.7 per cent), and; moderately sensitive to ampicillin (42.2 per
cent), kanamycin (37.4 per cent), neomycin (21.8 per cent) and cotrimoxazole (23.2 per
cent), but were resistant to other commonly available drugs and antibiotics. For most
doctors this was their first experience of coping with an epidemic of severe bacillary
dysentery and there was great confusion over the choie of antibacterial drugs and other
treatment. Nalidixic acid, although found to be most effective, was too expensive for
common use. Oral rehydration, the magic therapy for acute watery diarrhoea, was effective
in only about ten per cent of these cases, since in 90 per cent dehydration was not
serious. Preventive measures
A mass media campaign was begun which advocated boiling or chlorination of drinking
water, covering faeces with soil, protecting food from flies, avoiding eating exposed raw
vegetables and cut fruits, and washing hands with soap and water before eating and after
using the latrine. However, such measures are not easy to implement in some areas. In West
Bengal, for example, the total production of water-purifying tablets was only enough to
meet requirements for one or two days; scarcity of fuel limits its use for boiling
drinking water; and while there is convincing evidence that handwashing with soap and
water reduces transmission of shigella, people cannot be educated overnight to do this.
Consequently the epidemic took its own course and subsided only gradually. The reasons for the recent emergence of Shiga dysentery are not fully understood.
Resistance of the causative agent, Shiga's bacillus, to most commonly used and available
drugs is a major problem, and the case fatality rate is very high. Scientific knowledge
about the exact mode of transmission of the pathogen, the mechanisms of pathogenicity and
even about the actual cause of death due to the disease, is still inadequate. Such
knowledge might contribute to the development of better and more practicable public health
intervention measures, and an effective vaccine. Dr Sudhir Chandra Pal, Director National Institute of Cholera and Enteric
Diseases, Calcutta, India.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 25 June 1986  4 Page 5 6 4 Page 5 6
Drug treatment
Bradley Sack outlines current understanding of the use
of drugs for treating certain types of diarrhoea. The first objective of therapy for all diarrhoeal diseases is replacement of the fluids
and electrolytes lost in the liquid stools during the illness. In some dysenteric
illnesses, however, fluid losses are relatively minor and the main clinical symptoms of
fever, abdominal pain and toxicity are the result of invasion and destruction of the
epithelial cells lining the intestine, by pathogenic organisms or their toxins. In these
illnesses, antimicrobial therapy has a major role. Antimicrobial drugs
- In most diarrhoeal diseases, antimicrobial drugs have no proven value and should not be
given.
- In some severe diarrhoeal illnesses, antimicrobial therapy can be lifesaving. These
include dysentery caused by Shigella, especially S. dysenteriae 1 and some
cases of prolonged diarrhoea. Fortunately, these are relatively uncommon, except for the
present widespread outbreaks of S. dysenteriae I in some parts of the
world. In order to treat these illnesses most effectively, the laboratory is important
both to make the correct bacteriologic diagnosis and to indicate which antimicrobials will
be most effective.
- In cholera antimicrobials may be useful when given in addition to ORT because they
shorten the duration of illness and reduce the volume of stool loss.
- Antibiotics may also have some value in milder forms of dysentery due to Shigella, and
possibly in serious diarrhoea due to enteropathogenic serotypes of E. coli, and the
clinical syndrome of travellers' diarrhoea. In diarrhoea due to Campylobacter jejuni, antimicrobial
therapy is only useful if it is begun in the early stages of the illness, which is not
usually possible because detection of the organism requires at least two days using
special laboratory facilities.
- Antimicrobials are contraindicated in diarrhoea caused by non-typhoid Salmonella, unless
the Salmonella caused systemic invasion, because they are of no clinical benefit
and they prolong the excretion of these organisms in the stool.
- Antiparasitic drugs are valuable in symptomatic cases where trophozoites of Entamoeba
histolytica or Giardia lamblia are detected by microscopic examination of fresh
stool specimens.
Antimotility drugs
These include synthetic opiates, such as loperamide and diphenoxylate, and morphine
derivatives such as paregoric. In infantile diarrhoea and non-dysenteric types of
travellers' diarrhoea, antimotility drugs slightly reduce the duration of illness, but do
not decrease the rate of stool output, as they are not significantly antisecretory in
action. These drugs may give some symptomatic relief in adults, but are contraindicated in
children under 5 years old because of possible harmful side-effects, such as depression of
respiration and altered consciousness. In cases of dysentery, antimotility drugs may
actually increase the severity of the illness because clearance of the invasive organisms
from the colon may be delayed. Antisecretory drugs
Two drugs, chlorpromazine and berberine, have demonstrated antisecretory effects, but
neither has yet proven practical for routine use.
- Chlorpromazine reduces stool output somewhat in severe cholera, but it has little effect
in patients whose illness is not severe. For this reason, and because it causes
sleepiness, its use is not recommended.
- Berberine is a traditional anti-diarrhoea medicine in Asia. In studies on animals, it
has been shown to reduce stool output caused by enterotoxins of V. cholerae and
E. coli. However, studies in humans have not shown consistent beneficial effects.
It is not recommended for the routine management of diarrhoea.
Other drugs
Bismuth subsalicylate is moderately effective in adults with travellers' diarrhoea, but
the dose required is very large. Its mechanism of action is unknown. Cholestyramine is a
non-absorbable basic anion exchange resin. It acts both by deconjugating bile salts and
binding bacterial toxins. Preliminary trials suggest it reduces the duration of diarrhoea
in infants and further studies are underway. In combination with certain oral antibiotics
(i.e. gentamicin and neomycin), it has been effective in treating persistent diarrhoea,
that is cases in which acute diarrhoea continues for more than 14 days. High dosage may
prolong acidosis and there is not yet enough evidence to recommend the drug for routine
use. There is no evidence of efficacy for kaolin and pectin or any of a large number of
other drugs, including traditional medicines and anti-inflammatory agents such as aspirin. Guidelines for use of drugs
Although recommendations regarding the role of drugs in diarrhoea therapy are
incomplete, and often require laboratory back-up, the following general guidelines may be
useful, particularly when adequate laboratory support is not available:
- In patients with watery (non-bloody) diarrhoea no antibiotics are indicated unless
cholera is strongly suspected, as for example during a cholera epidemic. In that case
tetracyclira or another antimicrobial effective for V. cholerae should be used.
- In patients with dysentery, especially children who are febrile (temperature greater
than 38.5 ºC) or who appear seriously ill, appropriate antimicrobials such as ampicillin
or trimethoprimsulphamethoxazole (co-trimoxazole) should be given. The choice of
antibiotic should be based on known antimicrobial sensitivity patterns of Shigella strains
in the geographic area.
- There is no rationale for using any "anti-diarrhoeal drug" for routine
management of acute diarrhoea, especially in children under 5 years old. Fluid and
electrolyte replacement (ORT) remains the primary treatment for all diarrhoeal diseases.
Professor R. B. Sack, The Baltimore City Hospital, 4940 Eastern Avenue, Baltimore,
Maryland 21224, U.S.A.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 25 June 1986  5 Page 6 7 5 Page 6 7
Medicines with care
Drugs must be purchased, stored and distributed with professional skill. Patients
should use them carefully; this often depends on clear instructions. In this article Professor
D'Arcy and Dr Harron outline some practical
guidelines. Purchase
- All medicines must be purchased from reliable and well proven sources; if purchased in
bulk by Third World health authorities, then advantage should be taken of the WHO
certification scheme, through which the quality of medicines is assured.
- If medicines are purchased by the individual patient, then, where possible, professional
advice should be sought, preferably from a pharmacist. It can be dangerous to buy medical
supplies from nonofficial or non-professional sources.
Storage
- Medicines must be stored with care. The basic requirements are the same both for home
storage and bulk dispensary storage.
- Medicines:
- must be kept in a cool and dry place ;
- bulk containers should be stored off the ground so that they cannot be spoiled by rain
puddles;
- should never be allowed to stand in the sun;
- should be protected in sealed containers, from attack by insects and rats and containers
should be properly labelled;
- must not be used after their expiry date - often this is marked on the label - if not,
assume two years from purchase for all solid dosage forms and one year for liquid
preparations and creams and ointments. Discard any medicines that show discoloration,
fungal growth or any other signs of physical deterioration.
- Some medicines need storage in a refrigerator at a temperature below 5° C; this
requirement is usually shown on the container. Do not place any medicines in the freezing
compartment of the refrigerator (except for some vaccines which should be stored frozen.)
COSTLY MEDICINES WILL DETERIORATE IF THEY ARE NOT STORED CORRECTLY. Containers and labelling
- All bulk medicines must be stored in suitable closed containers which are labelled to
indicate the nature of the medicine, its source, quantity, dosage and, where applicable,
its expiry date.
- Smaller quantities of medicines prepared for individual patient
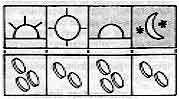
use must be dispensed in a suitable clean and closed container which is labelled with the
name of the medicine, the name of the patient, the date of supply, and the instructions
for use in a form that can be readily understood by the patient (if necessary pictograms
should be used to illustrate the required dosage schedule):
|
 |
Medicines must not be supplied to patients in a screw of paper or in an open and
unwashed container provided by the patient. Every distribution system of medicines should
consider the provision of cheap, closable, multipurpose containers as a priority. Distribution to the patient
- Distribution of medicines should always be in the care of a trained health care worker
(preferably supervised by a pharmacist and according to the prescription of a doctor) who
dispenses them in a suitable container.
- Labelling of medicines should be reinforced by verbal instructions to the patient or
relative. Check to make sure that the instructions have been understood before the
medicine is handed over.
COSTLY MEDICINES WILL BE WASTED IF THEY ARE NOT USED CORRECTLY.
|
Special precautions with medicines for diarrhoea
Oral rehydration salts (ORS) are available through the United Nations
Children's Fund (UNICEF) in water-proof foil packets. Both WHO and UNICEF are assisting
countries to produce WHO recommended formulations of ORS; for local production WHO
recommend: packaging of ORS in polythene where possible. The ORS formulation containing
trisodium citrate dihydrate (ORS-citrate) is more stable than the sodium bicarbonate
formulation (ORS-bicarbonate) especially in tropical countries where it has to be stored
in conditions of high humidity and temperature. Avoid the use of non-WHO recommended
formulations of ORS which may be less effective, less stable and more expensive. Although the use of germ-free water is preferable for mixing the rehydration solution,
ORS solution for oral rehydration can be prepared even when pure water is not available.
The cleanest safest local water should be used. However, where possible, boil and cool the
water before use. To minimise contamination, ORS solution should be made fresh every day,
covered and stored in a cool place. Ensure that the volume of water in which the ORS is
dissolved is correct. This is vital both in the pharmacy and the home. Check that the
patient's relatives understand about the correct volume, and possess a suitable container. Solutions for intravenous infusion have a role in the treatment of severe
dehydration in diarrhoeal diseases. Care is needed as some solutions do not contain
appropriate or adequate amounts of electrolytes required to correct the losses from
dehydration associated with acute diarrhoea. The needles, tubing, containers (bottles or
plastic bags), and fluids used for intravenous therapy must be sterile. Correct storage of
these components is therefore crucial and storage conditions must maintain sterility. It
is not necessary to store infusion fluids in a refrigerator. The containers should be
inspected at regular intervals for damage caused during transport or storage (e.g. leaks,
cracks, or splits in containers); all damaged containers should be discarded. When in use, it is helpful to mark intravenous fluid bottles at various levels with the
times at which the fluid should have fallen to those levels. This allows easy and rapid
monitoring of the rate of administration of the fluid.
|
Professor P F D'Arcy, Department of Pharmacy, and Dr D W G Harron,
Department of Therapeutics and Pharmacology, The Queen's University of Belfast, Lishum
Road, Belfast BT9 7BL, Northern Ireland.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 25 June 1986  6 Page 7 8 6 Page 7 8
| Development of oral rehydration |
Australia: Diarrhoea in Aboriginal children
The Aboriginal population in Central Australia live mainly in rural or remote areas
and, while they represent less than a third of the total population served by the Alice
Springs Hospital, their levels of mortality and morbidity from diarrhoeal disease are
disproportionately high. In the early 1960s, the infant mortality rate among the
Aboriginal population was almost 250 per thousand live births, one of the main causes of
death being acute diarrhoea - often in epidemic form and usually associated with protein
energy malnutrition. Oral rehydration
The rehydration fluid recommended at that time was dextrose in normal saline solution
(DNS) and many infants died of hypokalaemia (potassium deficiency) during outbreaks of
what was probably rotavirus diarrhoea. These infants were often severely dehydrated and
passed little or no urine, and it was considered dangerous to give potassium when there
was no evidence of kidney function. During one epidemic in 1966, sodium and potassium
concentrations in diarrhoeal stools were measured. The findings led to a modified oral
electrolyte mixture (MEM) containing potassium. Mortality rapidly decreased once MEM was
in common use. MEM powder was dispensed in small jars and had a relatively short shelf
life. Significantly however, the formula was similar to that of UNICEF oral rehydration
salts (ORS) in foil sachets, which became available a little later. ORS has now replaced
MEM and is used extensively throughout Central Australia. Teaching health workers about ORT
The use of ORS, recognition of danger signs of dehydration, and the supervision of
mothers during rehydration of their children are all basic skills taught to the Aboriginal
Health Workers and, despite occasional epidemics of diarrhoea, deaths from the disease are
far less frequent than they were. A card with a sliding insert, was designed to help
literate health workers and parents assess the levels of dehydration, carry out a standard
treatment for diarrhoea and monitor progress. (The technique of intraperitoneal infusion
was refined problems and introduced as a life-saving measure where oral rehydration
therapy had failed. A card describing this procedure was produced and distributed.)* Remaining problems
Although mortality levels from childhood diarrhoea among Central Australian Aboriginals
have fallen dramatically over the past 20 years, due largely to the introduction and
widespread use of an appropriate oral rehydration solution, the incidence of diarrhoea,
caused by organisms such as shigella, campylobacter or salmonella, continues to be
extremely high, and the admission rate to the base hospital at Alice Springs is of great
concern. Very few children avoid at least one hospital admission for diarrhoea during
their first year of life, and some are admitted many times. Diarrhoea makes an important
contribution to the under-nutrition seen in more than 20 per cent of Aboriginal children
under the age of five years. The continuing high attack rate of diarrhoea is almost
entirely related to of poor diet, living conditions, and lack of awareness of the
importance of community and personal hygiene. Dr Kerry Kirke, Regional Director, Alice Springs and Barkly Region, Department of
Health, P.O. Box 721, Alice Springs, N.T. 5750, Australia.
Copies of the diarrhoea slide rule are available from the Assistant Director, N.T.
Health, at the above address. *Editors' note: With modern and efficient oral rehydration therapy there is
virtually no place for intraperitoneal infusion nowadays. If a child is shocked it needs
rapid expansion of blood volume by intravenous infusion. A child who is unconscious or
vomiting a lot can receive ORS solution by naso-gastric tube.
|
Pakistan: Early use of ORS
In 1970, when Professor Abdul Billoo took charge of the Paediatric Unit at the Civil
Hospital in Karachi, nearly half the cases admitted were suffering from diarrhoea and
dehydration. The treatment method used was I.V. therapy but the resources available, in
terms of time, manpower and I.V. fluids and equipment, were not sufficient to cope with
the number of patients - and many died. After some experimentation, in 1972 the Unit started giving by mouth a solution of half
strength saline (0.45 % Na C1) and 4.5 dextrose in water*. At that time this was found to
be fairly safe, effective and acceptable, and greatly reduced the need for use of I.V.
drips. Home-made solutions, using the correct proportions of salt, sugar and water, have
since been successfully promoted in six outreach rural diarrhoea education programmes.
Citrus fruits, particularly oranges, and also bananas, are freely available in Pakistan,
and are promoted as a good source of potassium. The first trial of an oral rehydration
solution was made by Professor Billoo on two six month old children of some friends of
his, both suffering from severe diarrhoea, and moderate dehydration. Both children
responded well, and were fully recovered in 72 hours. "Both of them are now happy and
healthy young boys of 14 years, and I was proud of them and grateful to their parents for
their contribution to the success story of ORT in Karachi, which has a population of 7
million and where now nearly 70 per cent of mothers are aware of the use of ORT in
diarrhoea." Professor A G Billoo, Professor of Paediatrics, Dow Medical College and Civil
Hospital, Karachi, Pakistan. *These proportions are not sufficient to make an adequate oral rehydration
solution. The WHO recommended formula with the correct proportion of ingredients should be
used.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 25 June 1986  7 Page 8 7 Page 8
Carry on feeding
Diarrhoea Dialogue is a regular part of our medical student teaching programme
in Social Paediatrics at Makerere University. While convinced that ORT will prevent dehydration by early home management of
diarrhoea, and effectively rehydrate the mild to moderately dehydrated children brought to
health centres, clinics and hospitals, ORT is not the complete management of the child
with diarrhoea and prolonged use of ORT without adequate attention to calorific and
nutritional requirements can be disastrous. Emphasis should be placed on meeting these
essential requirements by continuing and, if possible, augmenting feeding. Many health
workers and parents persist in restricting food including milk during ORT. As sole feeding ORT provides less than 5 per cent of calorific needs and no other
nutrients. With its wide circulation we urge that Diarrhoea Dialogue should
continue to stress feeding during ORT as in="dd15.htm">issue 15. (See DD issue 23.) D A HiIIman, Professor of Social Paediatrics, Child Health and Development Centre,
Makerere University, Kampala, Uganda.
Leaf nutrient for malnutrition
In your="dd23.htm">issue No. 23, December 1985, you had articles on feeding
the anorexic child and on leaf nutrient. Unfortunately the relationship between the two
was not made clear. Actually leaf nutrient is one of the best foods to provide for
children recovering from diarrhoea. The moist product is soft so it does not need chewing;
and it can easily be made either sweet or spicy. A 40 gram portion of 50 per cent moisture
content material will provide a child with 12 grams of protein, about 40 per cent of his
normal daily needs. It will also provide all the required vitamin A as beta carotene.
This, according to West and Sommer (Food Reviews International 1 (2) p. 355-418 (1985)
and The Lancet, May 24, 1986.) can be of vital importance in reducing mortality and
morbidity rates for children. In addition, leaf nutrient contains significant amounts of
many other vitamins as well as calcium, iron and several other essential minerals. Studies have shown that where there is a reliable supply of fresh green leaves, leaf
nutrient costs only twice as much as cereal grains or about the same amount as beans and
other legumes. Cost analyses have shown that leaf nutrient is actually a least cost food
which provides many of the nutrients required by man. As such it can and should play a
vital role in combating malnutrition around the world. Walter J Bray, Sesaco Corporation, P. O. Box 4546, Yuma, Arizona, 85364, USA.
Editors' note: We would like to thank Dr Bray for pointing out the value of
using leaf nutrient for children with malnutrition, and during recovery from diarrhoea.
However, it is not always simple to produce, and where it is not available, other foods
should be given during and after the recovery period of diarrhoea. (See articles in="dd23.htm">DD23.)
Different tastes in water
Recently I have observed that the rural children, brought to our hospital with
diarrhoea, do not accept oral rehydration fluid as well as the town children. While
searching for the cause, a mother said 'My child is used to drinking well water and your
municipal tap water is tasteless.' The child accepted the well water readily. Since then
we have started asking whether a child is used to well water or tap water and have started
offering ORS in the water a child is used to. Our acceptance rate of ORS has increased
since then. Dr Anil Mokashi, Editor, Journal of Rural Paediatrics, Baramati, 413102, India.
ORT activities in Turkey
The main causes of child death in Turkey are bronchopneumonia and diarrhoea. The first
step taken in the field of child health was an immunisation programme targeted at children
aged under five years which has achieved a remarkably high coverage rate: over 80 per
cent. The second step towards lowering child mortality rates was the decision to use ORS
in diarrhoea. As part of the new ORT programme, the Ministry of Health and Social Affairs and the
Hacettepe Children's Hospital have worked together on an ORT education programme. Two oral
rehydration and diarrhoea research and training centres have opened in Hacettepe
Children's Hospital and the Gulveren Health Centre. Gulveren Health Centre is in a rural
'pilot' area of the University. It serves a population of 65,000. Mothers accepted the
training programme with great interest and more than 200 have already been taught about
ORT in each centre. It is expected that this number will rise once the educational
programme begins and with the help of promotion on television. A team has been established
in Hacettepe Children's Hospital to work on diarrhoea control with the Ministry, in
collaboration with UNICEF and WHO. AtiIIa Buyukgebiz M. D. and BenaI Buyukgebiz M. D., Gulveren Health Centre, Ankara,
Turkey.
Editors' note: A range of maternal and child health programmes are underway
in Turkey, led by the Ministry of Health and Social Affairs in co-operation with the
Ministry of Education, and DD will focus on these activities in a future issue. In
recognition of outstanding achievements in child survival activities, Turkey received a
special award in June 1986 at a National Council for International Health meeting held in
Washington D. C.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Editor Kathy Attawell
Editorial assistant Maria Spyrou Editorial advisory group
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Ruth Tshabalala (Swaziland)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), ODA (UK), UNICEF, WHO and GTZ
|
Issue no. 25 June 1986
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
updated: 23 August, 2019
|