|
| |
Issue no. 26 - September 1986
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 26 -
September 1986
|
DDOnline
Dialogue
on Diarrhoea Online Issue 26 September 1986  Page 1 2
Page 1 2
Climate, customs and diarrhoea
Weather patterns have long been linked in people's minds with patterns of disease.
'Winter vomiting' and 'summer diarrhoea' were recognised as recurrent child health dangers
many years before scientists were in a position to explain why and how these infections
came about. Problems of seasonality
|
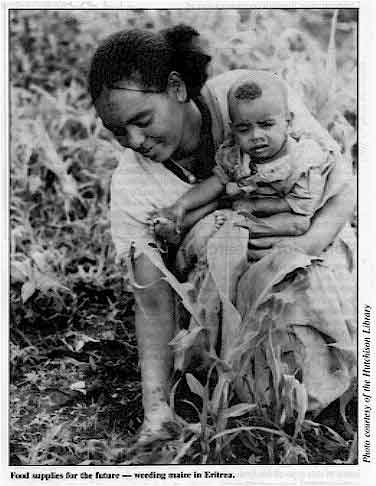
Food
supplies for the future - weeding maize in Eritrea.
In many parts of the world, people depend for their survival on rainfall which only
occurs at certain times. During the 'hungry season', when stores are running out, women
need to work extra hard in the fields to make sure the new crops benefit from precious
rains. Food supplies for the future are all important. In consequence, children and babies
suffer an increased risk of malnutrition and disease. Extremes of drought and of flooding
may make matters worse. Seasonal problems in The Gambia and in Bangladesh are described onpage three.
|
|
Value of behaviour change
People may not be able to change their weather but they can change their ways. Even
small alterations in the behaviour of mothers when handling their children will bring
about noticeable improvements (see="#page4">pages four and five).
The vital ORT message about how to prevent and treat dangerous dehydration due to
diarrhoea needs to be accompanied by appropriate family hygiene education, based on local
customs and circumstances (see="#page8">page 8). KME and WAMC
|
In this issue . . .
- Nasogastric feeding and rehydration
- The influence of climate, environment and behaviour on diarrhoea
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 26 September 1986  1 Page 2 3 1 Page 2 3
|
Water handling and cholera The majority of those infected with the cholera vibrio are not seriously ill, and many
are symptomless carriers. The germ spreads rapidly in overcrowded or slum conditions.
Person-to-person transmission through contamination of domestic food and water seems to be
important. A study carried out in Calcutta, India, found that carriers of V. cholerae
were contaminating domestic water with their dirty fingers, where water was stored
in wide-mouthed vessels such as buckets.
| Two methods were used
to see if transmission of infection could be reduced: chlorination of stored water, and
the use of a narrow-necked earthenware vessel (called a sorai) for water storage.
|

|
These were tried out in similar population groups in east Calcutta. The results showed
that transmission rates of cholera were significantly reduced in both the group
chlorinating their water (by 57.8 per cent), and in the group using a sorai to store their
water (by 74.6 per cent). A third control group, who used neither method, showed no
reduction in transmission. These results also suggested that exposure to infection outside
the home was relatively less important than transmission within the home. The sorai has
the additional advantage of being cheap and also acceptable to the local community. Its
narrow neck prevents the introduction of infected hands and germs into the stored water.
Bulletin of the World Health Organization, 64 (1): 127-131,1986. Studies on
interventions to prevent El Tor cholera transmission in urban slums. B C Deb et al.
Reprints of this article are available from Dr Deb at the National Institute
of Cholera and Enteric Diseases, P-33, C.I.T Road, Scheme XM, Beliaghata, Calcutta, 700
010, India.
|
Money for research
Funds will be available from WHO in 1987 to support biomedical and epidemiological
research in diarrhoeal disease control in the following areas: epidemiology and disease
prevention; immunology, microbiology, and vaccine development; case management. Applicants
wishing to apply for support should send 1-2 pages outlining the proposed project to the Research
Co-ordinator, CDD Programme, 1211 Geneva 27 Switzerland. Preference will be given to
projects of the most direct relevance to the problem of childhood diarrhoea in developing
countries. In addition, support is available for health services research, both operational and
applied research linked to national CDD activities. Those interested in this type of study
should write to their WHO regional office. Coconut water for rehydration?
Is water from unripe coconuts suitable for rehydration of children with acute
diarrhoea? In Tanzania, it is a popular drink and the Tanzanian National Diarrhoeal
Diseases Control Campaign has recently analysed it to see if it could be safely
recommended for rehydration. Compared to the WHO-recommended ORS formula, it is low in
sodium, chloride and bicarbonate but also contains a higher concentration of glucose,
potassium, magnesium and calcium. The amounts vary depending on whether the coconuts have
been harvested from coastal or inland areas. Coconut water is therefore not recommended as an alternative to ORS for rehydration.
Mothers in Tanzania have proved that they can, with proper teaching, prepare a safe and
effective salt and sugar solution at home for early treatment of diarrhoea in
children.* Porridge made from maize or millet flour is the main weaning diet for
most children, and, like rice-ORS in Bangladesh, may form the basis for a future
cereal-based ORS in Tanzania. Dr Abel Msengi, Department of Paediatrics and Child Health, Faculty of Medicine, P.
O. Box 65001, Dar-es-Salaam, Tanzania. *Editors' note: Where sugar-salt solution cannot be easily made, coconut water
may be a useful, clean drink in the very early stages of diarrhoea, before any dehydration
occurs. Further reading
1. Msengi A E et al, 1985. The biochemistry of water from unripe coconuts obtained
from two localities in Tanzania. E Afr. Med J. 62 (10); 725. ORS production
The revised WHO manual ORAL REHYDRATION SALTS - Planning, establishment and
operation of production facilities, mentioned in DD 23, is
now available in French. A Spanish edition will be available soon. Readers should write to
Mr Hans Faust, CDD Programme, WHO, 1211 Geneva 27, Switzerland. Many countries have now set up facilities for local production of ORS. For example, in
Nigeria, WHO and UNICEF have provided technical expertise to a private company,
ASTRA-AREWA, to set up production of oral rehydration salts packets. The ORHESAL packets
have been designed to make up 600 ml of oral rehydration solution, using the standard
sized containers widely available in Nigeria: a 600 ml beer bottle or two 300 ml mineral
bottles. Stickers, posters and prescription pads for doctors promote the use of ORS for
dehydration. The current annual production of 2 million packets of ORHESAL is
expected to increase to 6 million in 1987. Breastfeeding - a new book
Breastfeeding for Modern Mothers is a practical, helpful paperback by
Dr Clair Isbister. It is well illustrated and costs $5.95 Australian from Hodder and
Stoughton (Australia) Pty Limited, 2, Apollo Place, Lane Cove, NSW 2066, Australia. Erratum
Maureen Minchin tells us that Breastfeeding Matters is available from: 5
Meredith Court, Alfredton, Victoria 3350, Australia, not the address given in DD 24. US $, sterling and other currencies are acceptable as well
as Australian $. The price of $12 Australian can be reduced for readers unable to pay the
full cost. The author is willing to exchange the book for other publications.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 26 September 1986  2 Page 3 4 2 Page 3 4
| The seasons and diarrhoea |
The Gambia and Bangladesh
Seasonal variations in rainfall and temperature often bring changes in disease
patterns, especially diarrhoea. Very little is known about why this happens and patterns
may change from one year to the next. Mike Rowland discusses
seasonality and diarrhoea in The Gambia and Bangladesh.
|
Bangladesh: severe seasonal flooding The Gambia and Bangladesh share some common characteristics in climate including a cool
dry winter of three months followed by a hot dry spring, and hot wet summers of five to
seven months in length. The main difference is in the amount of rainfall. While The Gambia
may have 20-30 inches of rain per year, Bangladesh usually has up to four or five times
this amount.
|
 |
Drought is a recurring problem in The Gambia, floods in Bangladesh. These climatic
factors have an important impact on the incidence of diarrhoeal disease. A study in The
Gambia found there was a close link between the time of the annual peak in diarrhoea in
young children and the summer rains. A second peak of diarrhoea in the winter was also
significant and was shown to coincide with a short period of intense transmission of
rotavirus. The agents Of the enteric infections of childhood, the enterotoxigenic Escherichia coli (ETEC),
that is, those producing heat-stable toxin (ST), were found to be the most important
aetiological agents of diarrhoea in both countries, with a peak during the rains. ETEC are
thought to be transmitted mainly by food and water. In rural Gambia, water is obtained
almost exclusively from surface wells, 15 to 20 metres deep. It was found that, although
this water was faecally contaminated throughout the year, levels of contamination
increased by up to one hundred times within one or two days of the start of the rains
because excreta is washed into the wells. It was also clear that contaminated water and
domestic environment contribute to contamination of children's food. The high level of
contamination of food during the summer coincided with the time of high diarrhoea
prevalence. In Bangladesh it was shown that the incidence of ETEC diarrhoea in infants was
positively correlated with the frequency of consumption of weaning foods contaminated with
faecal coliforms. The seasonal peak of ETEC diarrhoea coincided with the time when food
was most contaminated due to higher bacterial growth caused by high temperatures. Cholera is endemic in many areas of Bangladesh but not in The Gambia. Though similar to
some other diarrhoeal diseases in showing a rainy season peak, the timing of peaks of
cholera incidence can and has changed from year to year in Bangladesh. The reason for this
and the variable occurrence of a less marked pre-rains peak of cholera is not known. A
similar pattern, with twice yearly peaks in incidence occurs with shigellosis, an
important disease in both countries, particularly Bangladesh where the more virulent
species predominate and are becoming rapidly resistant to routinely used
antimicrobials.
It has been suggested that diarrhoea epidemics occurring in the post-rains period might be
due to increasing concentrations of faecal organisms in dwindling water supplies, but a
study of village wells in The Gambia produced no evidence to support this. Social and economic factors In both Bangladesh and The Gambia women's' work is important in the rural farming
economy. During the main farming season, therefore, busy mothers have less time for
breastfeeding. In Bangladesh, for example, suckling time has been shown to be less, and in
The Gambia intervals between feeds are longer; children might even be prematurely weaned.
Smaller amounts of breastmilk were consumed by breastfeeding infants at this time of year
coinciding with poorer maternal nutritional status. This was also the season of poorest
nutritional status in children, leading to increased duration, and perhaps severity, of
diarrhoea. Personal hygiene, attitudes to breastfeeding, and weaning practices are important
factors in diarrhoeal diseases all year round, whatever the season. To be more effective,
health education messages could be varied according to the season, as different problems
occur at various times of the year. In a recent Mass Media for Infant Health Campaign in
The Gambia, the emphasis changed from nutritional to rehydration strategies at different
times. Changing the emphasis could help to offset the impact of the seasonal factors which
cause very high death rates from diarrhoea at certain times of the year. Dr M. G. M. Rowland, Associate Director, ICDDR, B, GPO Box 128, Dhaka 2,
Bangladesh. Further reading Seasonal Dimensions to Rural Poverty, 1981. Chambers R, Longhurst R, Pacey A, eds.
London: Frances Pinter (Publishers) Ltd. Diarrhoea and Malnutrition: Interactions, Mechanisms and Interventions, 1982. Chen
LC, Scrimshaw NS, eds. New York: Plenum Publishing Corporation. Mass Media and Health Practices. Field Notes, 1984. Offices of Education and Health,
Academy for Educational Development, Washington DC.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 26 September 1986
 3 Page 4 5 3 Page 4 5
| Environment, behaviour and the spread of diarrhoea |
A vulnerable age
A study in Bangladesh discovered high rates of diarrhoea in crawling infants. The
results and a range of interventions to help protect this age group are described in this
article. Diarrhoea occurs most often in Bangladesh in children between the ages of six and
eleven months - the time when they start to crawl. In rural areas, crawling infants come
into contact with chicken faeces and other animal dung on the ground inside and outside
the home. The ground is also contaminated with the baby's own faeces and those of its
brothers and sisters. Many infants put earth and faeces in their mouths and most suck
their fingers which have touched and will pass on germs and faecal matter. Infants in two villages near Dhaka were found to have high rates of illness and
malnutrition. Those whose families were poor and did not own land were more severely
affected - they had worse malnutrition and a higher incidence of diarrhoea. One village
suffered from severe seasonal flooding, contaminating the environment and probably
contributing to a very high diarrhoea rate. Crawling behaviour and environment In both villages most infants were put down to play for most of the day. In one village
nearly half the infants were down all day, and a further 23 per cent every morning and
afternoon. In the other, nearly 90 per cent were put down to play either all day or every
morning and afternoon. Fewer than 2 per cent of infants in both villages were put down to
play on the ground less than once a day. Most mothers said they rarely or never put a mat
or jute sack down for their baby to lie on or crawl around on, and only a third of mothers
were able to watch their babies continuously. The ground on which these infants were crawling was found to be highly contaminated.
Some sort of animal dung or faeces (usually chicken faeces) were found in 91 per cent of
play areas in one village, and in 70 per cent of play areas in the other. Half the mothers
had also seen their babies eating or touching faeces during the previous two weeks. Traditional beliefs
It was discovered that while most mothers knew that faeces were dirty, they were not
aware that faeces can cause disease. Hence they do not see the need to keep their homes
and yards clear of faeces and do not know that they are exposing their children to germs.
In fact most mothers bathed their babies every day to keep them clean. Poor traditional
weaning practices and poor food hygiene also contributed to high attack rates of
diarrhoea. Interventions and health education
Basic messages and a range of interventions to improve traditional hygiene and child
care practices were developed. Firstly, mothers needed to understand about germs, and the
fact that these cause diseases such as diarrhoea, even though they cannot be seen. Local
materials and ideas were used to demonstrate this to a mainly illiterate audience. Mothers
already knew that fishermen use alum crystals to purify river water for drinking. Alum
crystals were mixed with a glass of pond or river water that looked clean, but was not
free from germs. The dark coloured sediment that collected at the bottom of the glass was
explained to mothers as the bodies of tiny dead germs 'smaller than chicken lice' killed
by the alum. To show that germs stay on the hands and are passed on after washing with
just water, the mothers' hands were rubbed with red magenta make-up powder. Even after
washing, mothers could see that they still left a red handprint on their babies or any
household objects they touched. Interventions to keep the baby from touching and eating faeces:
- Sweeping the baby's play area four times a day. All households possessed a broom made of
stiff straw. Messages emphasised that brooms keep away germs and keep homes beautiful.
- Using a dirt disposer, like a trowel, or a farming hoe to remove faeces from the ground.
The dirt disposer was adapted from the hoe, made in the local bazaar and was popular with
villagers because they could remove faeces without soiling their hands.
- Using a covered pit or latrine to dispose of faeces.
- Using a special place for disposing of garbage.
- Keeping crawling infants in a playpen instead of letting them play freely on the ground.
Inexpensive locally made playpens of bamboo, jute and nylon kept the infants off the
ground, and could be easily cleaned. Mothers liked the playpens because they could get on
with their work and know their babies were safe.
Interventions to reduce transmission of germs:
- Washing hands with ashes or soap after defaecating (most households could not afford
soap but ashes were available and acceptable).
- Handling the water carrier (used for washing after defaecation) with the right hand so
that germs from the left hand do not contaminate the carrier for other users.
- Cutting the fingernails of all family members with a blade every week. (This helps to
prevent transmission of germs to the mouth as it is customary in Bangladesh to eat with
the hands.)
- Washing babies in a particular place after defaecation so that germ-contaminated water
does not spread everywhere.
Interventions to reduce transmission of germs during weaning:
- Keeping food covered to protect from flies, dirt, chickens and dogs.
- Storing clean plates and pots and pans upside down or covering them.
- Washing hands and plates with tubewell water before eating.
- Using only tubewell water for drinking and for mixing food for the baby.
Taken from Sanitary Conditions of Crawling Infants in Rural Bangladesh by
Marian E Zeitlin, Georgia Guldan, Robert E. Klein and Nasar Ahmad, with the collaboration
of Kamal Ahmad, and; Messages and Interventions for Social Marketing from A Village
Trial Laboratory for Developing Diarrhoeal Disease Control Behaviours by Marian F.
Zeitlin, Azmat Ara Ahmad, Nasar Ahmad, Georgia Guldan and Suaib Ahmed.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 26 September 1986  4 Page 5 6 4 Page 5 6
| Environment, behaviour and the spread of diarrhoea |
Soiled saris
Clothes can act as carriers of disease. Bonita Stanton
and John Clemens look at how the sari may spread diarrhoeal
infections.
Saris are worn by most women in India, Pakistan and Bangladesh and fairly widely
throughout the rest of Asia. The authors noticed that Bangladeshi women in slum areas of
Dhaka often used their saris for many household tasks as well as for clothing purposes. A
study was carried out to see whether this behaviour was common and if it affected the
rates of childhood diarrhoea.
Collecting data
 |
Mothers have many household tasks to do, as well as
looking after small children. Information was obtained from 247 families in Dhaka slum areas about the sex and age of
children under six; family income; maternal education; and attitudes of mothers towards
'misuse' of saris. Mothers were observed at home to learn about their usual hygienic
practices, including what they did with their saris. Information was also collected on the
incidence of diarrhoea among their children. Contamination of saris There was no practice that all mothers believed to be a wrong use of the sari,
including wiping a child's bottom after it had defaecated. Very few suggested that a
particular use 'can spread disease'. Misuse of saris was seen as wrong for other reasons.
such as 'it will make the sari wet'.
|
Altering behaviour
Discussion with mothers clearly showed that the women were not aware they were
contaminating their saris, or that the soiled saris could pass on diseases like diarrhoea
to their children. It is important to convince them of this danger, because they can
easily change their own behaviour and see results for themselves, unlike many other
hygiene interventions. Success in preventing misuse of saris could serve as a good
indicator to health workers of the effectiveness of an educational message in altering
behaviour in a sanitation programme. Also, as general hygiene conditions improve, personal
hygiene practices such as misuse of saris will become even more important. Bonita Stanton, Director, Urban Volunteer Program, and John Clemens, Scientist,
ICDDR, B, GPO 128, Dhaka 2, Bangladesh.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 26 September 1986  5 Page 6 7 5 Page 6 7
Using a nasogastric tube
Christine Candy describes the practical issues involved. Where possible, oral rehydration solution and food should be given by mouth. A
nasogastric tube is useful when children are unable to drink safely and in sufficient
amounts for any of the following reasons: severe dehydration; if IV therapy is
unavailable; low birth weight infants; or the child is drowsy or vomiting. Severely
malnourished children may be fed initially in this way if they are too weak or anorexic to
eat or drink normally. It is therefore important that health workers know how to use
nasogastric tubes.
|
Equipment The health worker will need the following:
- Nasogastric tube. A 6 french gauge tube with an internal diameter of 1.4mm, or an 8
french gauge tube with an internal diameter of 1.8mm, is usually suitable. Check that
fluid will flow easily down the tube, before passing it down. (If proper nasogastric tubes
are not available, polythene/nylon tubes of the right size can be used, provided they are
clean, rinsed and have no rough edges.)
- Lubricating fluid such as: 'KY Jelly' or Vaseline if available; water; or mothers'
saliva, if working in field conditions.
- Syringe (20 ml or 50 ml). This can be used afterwards as a funnel for giving feeds.
- Blue litmus paper, if available.
- Adhesive tape.
- Stethoscope if available.
- Fluid to be given.
|
Method
- Explain to the child's parents and the child, if old enough to understand, what you are
going to do.
- Lie infants flat. Lie unconscious patients on their sides to avoid aspiration (the
regurgitation and inhalation of fluid into the lungs). Older children may prefer to sit
up.
- Measure the approximate length from the child's nostril to the ear lobe and then to the
top of the abdomen (just below the ribs) with the tube, and mark the position. This will
be a guide to how far to insert the tube.
- Clean the nostrils to remove mucus. Lubricate the tip of the tube and gently insert into
the nostril. Pass the tube down through the nose slowly and smoothly. Stop if the child
gags (retches or chokes) and see if the tube is coiled in the mouth. If it is, gently pull
out the tube and try again.
- If the child is conscious, give a drink of water. This helps to pass the tube down
towards the stomach and reduces discomfort.
- If the child coughs, the tube may be going into the trachea (windpipe) - pull it out
gently and try again. NB. A child who is partly or completely unconscious, may not have a
cough reflex and the tube could go down the trachea without causing coughing. Always watch
for cyanosis (blue lips and tongue) and distressed breathing. These may be the only signs
in an unconscious patient that the tube is entering the lungs.
- Continue to pass the tube down until the position marked reaches the nostril. The end of
the tube should then be in the stomach. Check once again for choking, restlessness or
cyanosis. Fix the rest of the tube with adhesive tape below the nose and to the cheek or
side of the forehead.
- To check that the tube is in the stomach, use the syringe to suck up some fluid and test
with blue litmus paper. If the colour changes from blue to red the tube is in the stomach.
If blue litmus paper is not available, but the fluid sucked up is clear, containing mucus
or partially digested food, this also shows that the tube is in the stomach.
- Another test is to inject 20 to 50 ml of air down the tube while listening to the upper
abdomen, either with a stethoscope or directly with the ear. A distinct gurgle will be
heard as air enters the stomach. (This will not be heard if the tube is in the lung).
- If satisfied the tube is in the correct position, inject 5 to 10 ml of fluid (saline or
OR solution, not milk formula) by syringe, and again look for choking or cyanosis.
Rehydration and feeding
Where possible, give a continuous drip of fluid. If this is not possible, give frequent
small amounts using the syringe as a funnel. Hold the syringe upright, about 30 cms above
the child's head, for a slow and gentle flow. After each feed, close the tube with a
stopper or clamp and note amount given. Before each feed (or every four hours in
continuous feeding), look into the mouth to make sure the tube has not come out of the
stomach into the throat. Suck up a little fluid and check as before. Children who are able to drink will normally refuse ORS once rehydration is complete
and they are no longer thirsty. However, in nasogastric feeding, the normal thirst
mechanism is bypassed and it is possible to give too much fluid. It is therefore important
to stop giving ORS by nasogastric tube as soon as the child is able to drink normally or
is fully rehydrated. Overhydration can be dangerous. Prolonged nasogastric feeding If feeding continues for more than 24 hours, do the following:
- Clean the nostrils with warm water every day, especially around the tube. Change the
tube to the other nostril every few days. Keep the mouth very clean with a dilute solution
of 8 per cent sodium bicarbonate, if available, or citrus fruit juice. This helps to keep
the saliva flowing and prevents infections.
- Wet adhesive tape quickly makes skin sore. Take off damp tape with plaster remover or
ether. Clean skin with water and dry thoroughly. Change the position of the tape from time
to time.
Stopping nasogastric feeding If feeding has been continuous, start by changing to hourly then two hourly feeds. Then
give every other feed by mouth during the day, continuing tube feeds at night. Tube feeds
can then be gradually stopped as the amount taken by mouth increases. To remove the tube:
- Remove the adhesive tape.
- Take the tube out gently and smoothly. (Older children may prefer to remove it
themselves).
- Offer the child a drink and gently cleanse the nostrils.
After prolonged nasogastric feeding a child may have feeding problems or loss of
appetite. Patience and encouragement are needed to establish feeding by mouth again. Christie Candy, Paediatric Nurse Tutor, Queen Elizabeth School of Nursing,
Edgbaston, Birmingham, U. K.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 26 September 1986
 6 Page 7 8 6 Page 7 8
An ORT centre in Malawi
Dr Mbvundula describes the impact of an ORT training
centre at the Kamuzu Central Hospital in Lilongwe. The CDD programme in Malawi became fully operational during 1985, when oral rehydration
therapy (ORT) units were set up in all hospital out-patient departments, and ORT was
integrated into the activities of all health facilities. Before this, an ORT training
centre had been established in July 1984 at the Kamuzu Central Hospital out-patient
department in Lilongwe. During the next five years, the national CDD programme plan hopes
to be able to meet the following targets:
- offer effective out-patient and in-patient diarrhoeal disease treatment;
- educate mothers about ORT,
- decrease hospital admissions from diarrhoeal diseases;
- decrease hospital case fatality rates from diarrhoeal diseases.
The ORT Centre The Kamuzu Central Hospital (KCH) is the main referral centre for the Central and
Northern regions of Malawi, and has a paediatric ward with 97 beds. The occupancy rate of
the ward is around 200 per cent all year round, with many children sharing beds. The
greatest number of admissions to the ward occurs between December and May, coinciding with
the peak season of diarrhoeal diseases. Between 1981 and 1983, approximately seven per cent of admissions to the paediatric
ward were for diarrhoeal diseases. Of children hospitalised with diarrhoeal disease during
this period five per cent died. Impact of activities
|
A meal for a small child in Malawi
An evaluation of the ORT Centre after one year showed that:
- A total of 1,711 children had been treated, of whom 35 (two per cent) were admitted as
in-patients.
- Seventy-five per cent of these children had diarrhoea alone, the rest had diarrhoea in
combination with other illnesses such as malaria and acute otitis media. (Children with
measles are admitted directly to the paediatric ward to avoid spreading the disease in the
ORT Centre. Therefore measles associated with diarrhoea was rarely seen at the ORT
Centre.)
|
 |
- Of the children treated at the ORT Centre: 62 per cent were aged 0-12 months; 26 per
cent were aged between 13 and 24 months; and 12 per cent were over 24 months of age.
- Admissions to the paediatric ward decreased by 40 per cent compared to figures for
1981-1983.
- The case fatality rates for the paediatric ward did not change, perhaps due to the fact
that only severely ill children were admitted - milder cases being treated in the ORT
Centre.
National hospital reporting during 1985 showed a decrease in admissions due to
diarrhoeal disease throughout Malawi, and this is probably the result of the establishment
of ORT units in all health facilities in the country. Dr Mbvundula, Chief Paediatrician and Chairman, CDD Committee, Ministry of Health,
Kamuzu Central Hospital, P. O. Box 149, Lilongwe, Malawi. Editors' note: WHO has recently published a manual entitled: Diarrhoea
Training Unit-Director's Guide. It contains useful information on setting up and
running a diarrhoea training unit. Copies are available free of charge from the Director,
Diarrhoeal Diseases Control Programme, WHO, 1211 Geneva 27 Switzerland.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 26 September 1986  7 Page 8 7 Page 8
ORS composition
I am receiving DD regularly. Thanks for the valuable information. I use it for
the teaching of health workers who only know 'Farsi' language. We are using ORS with
satisfactory results in terms of tolerance, and response. I wish to know your opinion
regarding the composition of the ORS packet enclosed. Dr Gopal P. Gupta, PO Box 458, Sanandaj, Iran.
Editors' note: Thank you for your letter to DD enclosing the oral electrolyte
packet (Pursina) which you are currently using in Iran. As you can see from the comparison
table below, the Pursina solution is deficient in sodium and chloride for severe secretory
diarrhoea. It also contains rather too much glucose which could hold fluid in the gut
lumen by osmotic tension. The trace elements are not necessary if children are receiving
milk or other food, which is the WHO recommendation as soon as initial rehydration is
completed within 2-4 hours. The solution will, however, probably be of some value in
milder cases.
Rehydration solutions (comparison in
mmol/l) |
| |
ORS solution
WHO/UNICEF |
|
OraI Electrolyte
(Pursina) |
| Bicarbonate |
Citrate |
|
| Sodium |
90 |
90 |
30 |
| Potassium |
20 |
20 |
25 |
| Chloride |
80 |
80 |
25 |
| Citrate |
- |
10 |
25 |
| Bicarbonate |
30 |
- |
- |
| Glucose |
111 |
111 |
194 |
| Sulfate |
- |
- |
4 |
| Magnesium |
- |
- |
4 |
| Phosphate |
- |
- |
5 |
| Calcium |
- |
- |
4 |
| Saccharin |
- |
- |
(10 mg) |
Taste and temperature
Since UNICEF introduced ORS packets in Pakistan a few years ago, we have been using and
promoting ORT. I have observed that sometimes children refuse to take it. Probably because
commercial packets of ORS are widely available in Pakistan, homemade ORS is not popular.
(However, I do not think ORS packets would be available in remote areas of Pakistan, and I
do not think people there know how to prepare ORS at home either). One pharmaceutical
company has made orange-flavoured ORS. That too is often refused by children. I feel it is
because of the TASTE of the solution and also the TEMPERATURE of the water added. Here in
towns and cities, children, unlike those in the villages, are used to cold water. My
mother tried to give my child ORS with a little ice in it. It was very well accepted. I
agree it is costly for people in the villages to use ice, but wherever we can find ice
prepared from boiled water, we tell the parents to add it to ORS. Do you agree? Do you
think orange-flavoured ORS is technically sound?
Dr (Capt.) Mohammed Asif, Director General, Gulshan Hospital, A-2/3 Gulshan e-Iqhal,
Karachi, Pakistan.
Editors' note: One important symptom of dehydration is thirst. Because they
are thirsty, most dehydrated children will accept ORS readily, even if it is unflavoured
and given at room temperature. Refusal to accept ORT usually means dehydration has been
corrected or is quite mild. Some children, especially those over two years and with only
mild dehydration, may accept flavoured or cooled solutions more readily, but it is not
certain that this has much practical importance; moreover, the possibility of excessive
intake should also be considered. See See="dd22.htm">DD 22 for
practical hints on giving ORT.
Hygiene outside the home
We are currently implementing an educational program for rural mothers with children of
five years or less in the areas of oral rehydration therapy and child growth monitoring.
In developing educational materials, investigation and subsequent testing of materials, we
have encountered a real difficulty. Mothers and children spend a large portion of their time in the fields - often long
distances from their homes. This means that they are working and eating almost every day
with little or no access to water, outhouse or any type of sanitation facilities.
Promoting good hygiene is a primary concern of ORT/CGM. This, however, becomes a major
obstacle when the 'target' group spends such a large portion of time working in the
countryside where they have to prepare food and feed young children. As you well know, the
classic educational materials for ORT etc. demonstrate hygienic practices in the home,
with sufficient water, bowls, soap, heating facilities and so on. This is not the Bolivian
reality, nor do we think it is the reality in most developing countries. We are concerned
about how this problem can be dealt with effectively and would like any suggestions or
ideas you may have. Certainly there are no easy answers but, based on the world-wide DD
readership, we would be very interested in your response to this problem.
Curt Schaeffer, PRITECH Representative, and Dra. Ana Maria Aguilar, Consultant to
PRITECH, La Paz, Bolivia.
Editors' note: Several actions could help overcome these problems. For
example, special areas for defaecating well away from any water source, play areas or
places where people rest or eat. Even cleaning and rubbing hands with grass, soil, sand or
leaves after defaecating and before handling food, and keeping fingernails short, can
help. Cover food to protect against flies and, where possible, reheat thoroughly before
eating. The Editors would welcome suggestions from DD readers with experience of similar
problems, for publication in a future issue.
|
| In the next issue . . .
DD 27 will look again
at the role of parasites in diarrhoea |

Scientific editors Dr Katherine Elliott and Dr William Cutting
Editor Kathy Attawell
Editorial assistant Maria Spyrou Editorial advisory group
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Ruth Tshabalala (Swaziland)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), ODA (UK), UNICEF, WHO and GTZ
|
Issue no. 26 September 1986
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
updated: 23 August, 2019
|