|
| |
Issue no. 23 - December 1985
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
updated: 23 April, 2014
Pages 1-8 Dialogue on Diarrhoea Online Issue 23 - December
1985
|
DDOnline
Dialogue on Diarrhoea Online Issue 23 December
1985  Page 1 2
Page 1 2
Diarrhoea, feeding and watching their weight
Diarrhoea kills Third World children two ways: dramatically quickly by severe
dehydration in acute watery diarrhoea; and more slowly, but just as surely, in a deadly
partnership with other infections and with malnutrition. ORT: first step in child survival Oral rehydration therapy (ORT) is immediately life-saving in acute diarrhoea. All
health workers and all families must be given the knowledge and the means to carry out
ORT. Its promotion is already keeping alive thousands of children who would otherwise have
died. On its own, oral rehydration may not be enough for many children. Previous issues of DD
have emphasized the need to carry on feeding during diarrhoea (DD 15)
and to give extra food afterwards. Both the nutritional and the protective values of
breastmilk have been constantly stressed (see="dd17.htm">DD 17), andDD 16 described the significant role immunization
programmes can play, particularly against measles.
|
Properly fed and immunized children will recover rapidly from
infections such as diarrhoea.
Properly fed and immunized children, like those in the picture on this page, recover
rapidly from acute dehydrating diarrhoea if given ORT and their growth and development
will only be temporarily affected.
|
 |
The situation of most Third World children is much less fortunate. Malnutrition goes
hand in hand with ignorance and poverty. Safe water supplies and sanitation are seldom
available and effective immunization programmes have still to reach vast numbers of
families. Primary health care services, if they exist at all, are always overstretched.
Diarrhoea is a recurrent danger which needs more than just ORT if these children at such
serious risk are to survive and to grow up into healthy adults. Their future can
nevertheless become much brighter if feeding during and after diarrhoea is recognized as
being equally as important as managing dehydration. Convincing the mothers In the short term, health workers must explain, in ways that mothers can readily
understand, the need to feed children with diarrhoea appropriately - and to continue extra
feeding for at least several weeks after the child has recovered. The child who is not
hungry has to be persuaded to eat (see page 6). Already
malnourished children who develop diarrhoea will need special care to improve their
general health and to make sure they catch up to normal in their growth( see pages="#page4">4, 5 and 6). If this is done,
they will then be less likely to be seriously affected by any further attacks of diarrhoea
or other infections. And giving suitable foods as well as oral rehydration fluids during
diarrhoea has an immediate benefit that mothers will appreciate: the amount of the
diarrhoea loss becomes smaller. Growth monitoring as prevention
In the longer term, the problem of diarrhoea combined with malnutrition requires a
preventive as well as a curative approach. Growth is the sign of a healthy child. Failure
to grow steadily is the signal that something is wrong with a child's health. More often
than not, growth faltering occurs simply because not enough food, or not enough of the
right kinds of food, is being eaten. Making sure that all of the children are maintaining
good growth and development should be the responsibility of everybody in a community, and
not something that is left to busy and scarce health workers. Information about how to
make better use of suitable local food resources (see="#page3">page 3)
can help a great deal to prevent malnutrition. The weighing and measuring of children to detect poor growth or growth faltering need
not be difficult. DD 24 will contain a pull-out supplement,
describing techniques and equipment suitable for growth monitoring at community and health
centre levels. Records of child growth must be kept simple so that everyone concerned can
see at once when children lose weight or fail to gain weight at the expected rate. Such
children should then be given special care immediately in the form of extra food and
treatment for any infection. With this care, children in deprived areas of the world will
be much less at risk of serious illness or of death the next time they get diarrhoea. K.M.E. and W.A.M.C.
|
In this issue . . .
- Feeding the anorexic child
- Issues in growth monitoring
- Persistent diarrhoea
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 23 December
1985  1 Page 2 3 1 Page 2 3
Reviews
Interventions for the control of diarrhoeal diseases among young children:
supplementary feeding programmes. Feachem R G, WHO Bulletin: 61( 6): 967-79. The link between diarrhoeal diseases and nutritional status has been accepted for many
years. Evidence that poor nutritional status predisposes to more frequent attacks of
diarrhoea, or that supplementary feeding programmes can reduce the incidence of diarrhoea,
is not strong. Research findings, however, suggest that poor nutritional status is
associated with more severe diarrhoea when infection occurs, and with a higher case
fatality rate. This article reviews the effect of supplementary feeding programmes on diarrhoeal
disease morbidity and mortality among pre-school children. It uses data from field studies
in developing countries, where children received an enhanced food intake over several
years on a continuing and community-wide basis. Therapeutic feeding has not been included;
such feeding can be life-saving for the severely malnourished child. Also excluded are
feeding programmes in emergency or disaster situations where shortage of food supplies may
be the cause of malnutrition in a majority of children. It is suggested that supplementary feeding programmes are of questionable value, being
expensive and requiring high logistic and managerial inputs. In addition, many programmes
have failed to significantly improve the nutritional status of the most at-risk group. It
is therefore unlikely that supplementary feeding programmes can be regarded as
cost-effective interventions for national diarrhoeal disease control programmes.
Nevertheless, the local health infrastructure can be used to identify those children who
are at a high risk because of significant under-nutrition. Feeding which is targeted
effectively at this group can have a worthwhile impact on their nutritional status and
thus on the duration, severity and outcome of diarrhoea episodes. Unfortunately this
target group is hard to reach since it often includes the poorest and most underprivileged
children below two years of age. A new book, Diarrhoeal Disease and Malnutrition: A Clinical Update edited by
Michael Gracey, Professor of Child Health, University of Western Australia, Director,
Gastroenterology and Nutrition Research Unit, Princess Margaret Children's Medical
Research Foundation, Perth, Western Australia, has recently been published. The book is
available from the publishers, Churchill Livingstone, Robert Stevenson House, 1-3 Baxter's
Place, Leith Walk, Edinburgh EH1 3AF and is priced at £30.00. Guide to Mass Media Support Materials for Nutrition Education in Developing
Countries. Griffiths et al, 1985. The Guide was developed primarily for nutrition educators in developing countries, and
describes and reviews 316 nutrition education resource tools from a variety of country
sources. Copies of the Guide, which also contains contact addresses, are available from
(INCS) International Nutrition Communication Service, Education Development Center, Inc,
55 Chapel Street, Newton, MA 02160, U.S.A. Free to developing countries. Child Health in the Tropics: Edited by D. B. Jelliffe. Fifth edition.1985. Published
by Edward Arnold. Writing about growth and development, F John Bennett describes the importance of growth
monitoring and the serious consequences of malnutrition in both children and adults, and
provides information on average weight and height levels. Low birth weight babies, methods
of identifying the low birth weight baby, the causes and prevention of low birth weight,
and the risks to and the management of the low birth weight infant - including feeding -
are dealt with by Aaron Ifekwunigwe. The following chapter focuses on young child feeding
and describes the benefits of breastfeeding and correct weaning procedures, preferably
using locally available and affordable foods. This is particularly crucial in view of the
widespread malnutrition which causes many deaths, either directly or from associated
infections. Although the importance of oral rehydration treatment in the management of diarrhoea is
now generally recognized, Jelliffe and others were advocating giving drinks of salt, sugar
and water in currently acceptable proportions in the early 1960's, years before this
therapy received scientific acclaim and intense promotion. Throughout the book, the
sections on treatment have been updated, and preventive care is now strongly emphasized
with new chapters on linking the health of the child with that of the mother, training
primary health care workers, community participation and child health policies. This book contains much useful information for doctors and health professionals working
with children in tropical countries. Easier to open
|
Modified
packet design for easier opening.
In="dd13.htm">DD issue 13 we highlighted the difficulty some mothers
have in opening ORS packets without using their teeth or scissors. Since then, several
manufacturers have modified ORS packet design to include a small V-shaped nick for easier
opening. This picture shows an example produced by the Government Pharmaceutical
Organization in Thailand.
|
 |
|
In the next issue . . .
In DD 24 we will be reporting on the Second International
Conference on Oral Rehydration Therapy, held in Washington in December 1985. We will
also focus on the promotion of oral rehydration therapy outside the health services.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 23 December
1985  2 Page 3 4 2 Page 3 4
Promoting better nutrition: Leaf Nutrient
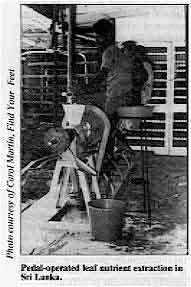 |
Pedal-operated
leaf nutrient extraction in Sri Lanka.
Dark green leafy vegetables (DGLV) have long been recommended as a cheap, good and
readily available source of protein, beta carotene (which the body can turn into Vitamin A
provided that at least some fat or oil is also eaten), iron, calcium and unsaturated fats.
But DGLV are bulky and it is difficult for children to eat sufficient quantities to offset
an otherwise poor diet. A simple pulping machine, as shown, can separate the fibre (which
makes excellent cattle feed) from the juice which contains the important nutrients. The
juice is heated to 90°C to curdle it. After straining, the curd washed and pressed before
being added to local dishes or eaten as it is. Any non-poisonous green leaf can be used to
make this leaf nutrient (LN), which field trials have shown to be an effective food
supplement to promote growth and to prevent anaemia, night-blindness (xerophthalmia) and
protein energy malnutrition (PEM).
|
The process can become an appropriate and profitable community activity, and trials
have so far not encountered any objections to the colour, flavour or texture of the LN.
For further information, please write to: Find Your Feet Ltd, 13-15 Frognal, London NW3
66LP, UK. ORT: educational campaign in Malawi
|
This poster is one of a series of
visual aids for ORT education being field-tested in 24 rural villages in Malawi. The
results will be incorporated into a mass media campaign to combat childhood communicable
diseases, including diarrhoea, being planned by the Ministry of Health*. Sent to DD by Ann Kurth, Centre for Population and Family Health, Faculty of Medicine,
Columbia University, 60 Haven Avenue, New York, NY 10032, U.S.A. (Formerly Research
Fellow, Centre for Social Research, Zomba, Malawi.) Editors' note: Where safe water is not available, and
boiling water is difficult, the cleanest water available should be used without delay to
make up oral rehydration solution.
|
 |
Taken from: ORT education: results of a pilot study in the Lilongwe Agricultural
Development District, 1985. *USAID is supporting mass media am other ORT-related health education activities in
Malawi. Tata Trust A donation from the Sir Dorabji Tata Trust in India has enabled us to set up a
distribution office at the Christian Medical Association of India (CMAI), 'Suvarna' 58/
C-l, Gokulpeth, Nagpur 440010, India, to begin the expansion of DD circulation in
India. We would like to express our appreciation of this generous support for the Dialogue. Nutrition forum 'Nutrition and Diarrheal Disease Control', the report of their third International
Conference held at the West Dean Conference Centre, U. K. in August, 1985, was published
by the International Nutrition Planners Forum in December, 1985. Edited by Dr. Jose O.
Mora, the Conference Co-ordinator, and Mr. Jim McEuen, copies can be obtained from the
Office of Nutrition, Bureau for Science and Technology, USAID, Washington DC 20523, USA. WHO manual: ORS production A revised manual: ORAL REHYDRATION SALTS - Planning, establishment and operation of
production facilities - has been produced by the Diarrhoeal Diseases Control Programme
in collaboration with the Pharmaceuticals Units of WHO and UNICEF. The guidelines in the
manual may be adapted for use in different countries and are an updated version of Guidelines
for the production of oral rehydration salts (80.3). Available from CDD
Programme, WHO, 1211 Geneva 27, Switzerland. Erratum The clinical advice page in issue 22 of DD was co-authored by Dr Ahmed Youssef
and Dr Norbert Hirschhorn. The editors would like to offer their sincere apologies to Dr
Youssef for omitting his name from the credits for this article. Note to readers Copies of this page 'Successful ORT' are available from DD as an information sheet or
as a large poster.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 23 December
1985  3 Page 4 5 3 Page 4 5
| Practical issues in growth monitoring |
Diarrhoea and growth
Frequent episodes of diarrhoea may result in malnutrition and set-backs in growth.
Growth monitoring enables health workers to identify children at risk. David
Nabarro discusses important factors to consider before growth monitoring is
introduced as part of a community health programme. Steady growth is a sign of a healthy child. Monitoring growth means that progress is
regularly checked, and should be part of good health care. Growth faltering (poor weight
gain, or weight loss) may result from malnutrition and/or other conditions which put the
child's health at risk - such as infectious diseases, particularly diarrhoea. Recent
studies in Bangladesh (1) confirm that poor weight gain or weight loss are sensitive
indicators of the risk of child death in the succeeding two months. Growth monitoring, and
the detection of those children whose growth is faltering, enables mothers and health
workers to discover which children are in danger, and also to check a child's response to
treatment. It is therefore a potentially valuable strategy to improve the health of
children. Issues of implementation Two important issues to consider are:
- will growth monitoring be worth the effort involved?
- how can growth best be monitored in the context of existing health services?
- Growth monitoring takes time.
The incidence of malnutrition and of diarrhoea varies with age and, often, with the
seasons. Children becoming malnourished can only be identified through regular growth
monitoring - at least every two months. Growth monitoring is a time-consuming activity for
health workers and community members alike. Most health workers have far more to do than
the available time allows. Mothers are expected to bring children for regular monitoring,
whether or not a child is unwell. This takes time for travel and waiting at the clinic,
and a day's wages may be lost.
- Growth monitoring on its own is not enough.
If growth monitoring is to lead to an improvement in child health:
- Health workers must have time to weigh or measure children, record results and interpret
them, discuss them with mothers and recommend action. This takes a minimum of four minutes
per child.
- Health workers need to be trained to recognise growth faltering and to diagnose reasons
for it.
- Health workers must also have access to facilities that will permit successful
intervention if a child is not growing adequately.
- Mothers can play an important role.
Some problems can be overcome if they, rather than health workers, are responsible for
monitoring their children's growth. Reports from Indonesia show that, while mothers cannot
be treated as 'professional weighers', a different approach has led to good results.
Neighbourhood nutrition clubs were established, using social marketing techniques to
emphasize the importance of weight gain rather than reaching a particular nutritional
status, and to stress the 'wisdom of village motherhood' rather than the 'scientific
basis' of nutrition (2).
- Is the measuring technique the key to a successful growth monitoring programme?
Not necessarily. The energy, skill and commitment of the health worker, the degree of
community involvement and the resources available for intervention when growth failure is
detected, are all as important in determining the results of any programme as the
technique that is selected.
Infection and weight loss Facilities for treating illness must be available since in many cases weight loss
results from infection. Infections, such as diarrhoea and measles, cause decreased
appetite, reduction in food intake and nutrients and a breakdown of tissues. Together
these cause weight loss. The role of infections in precipitating malnutrition has been
well-documented in Central America (3), Bangladesh (4), and The Gambia (5). In one
programme in Nepal, over 95 per cent of malnourished children attending a Mother and Child
Health Centre were suffering from infectious illness (6). Studies carried out in
Bangladesh suggested that, even if mothers are given additional food for their children
and intensive education, the potential for increasing child food intake during illness is
limited. Children with severe malnutrition or anorexia need careful re-introduction of
food (see page 6). Without appropriate medical treatment and
restored appetite, children will not eat and regain the weight that has been lost. Growth
monitoring therefore must be associated with an effective curative service, if the
incidence of malnutrition is to be reduced in an environment where infections and
diarrhoeal disease are common. Health education and nutrition education on their own are
not enough. Integrating health and nutrition
The incidence of malnutrition and diarrhoeal disease is likely to be highest among the
poorest families in the least developed countries. A growth monitoring programme can do
little to overcome the underlying economic and social causes of malnutrition and disease,
but may help to direct interventions to those at greatest risk. Where well-developed
primary health care services do not exist, it might be better to concentrate resources on
programmes that benefit all the children in the groups at greatest risk of malnutrition
rather than to try to identify individuals in difficulty. Dr David Nabarro, Liverpool School of Tropical Medicine, Pembroke Place, Liverpool
L3 5QA.
- Bairgari R et al, 1985. Alternative anthropometric indicators of mortality. Am. J.
Clin. Nut. 42 pp 296-306.
- Rohde J and Hendrata L, 1983. Development from below: transformation from
village-based nutrition projects to a national family programme in Indonesia. Practising
Health for All: by Morley, Rohde and Williams, Oxford, OUP.
- Mata L, 1978. The children of Santa Maria Cauque: a prospective field study of health
and growth. Cambridge, Mass, NUT Press.
- Black R E et al, 1984. Effects of diarrhoea associated with specific enteropathogens
on the growth of children in rural Bangladesh. Pediatrics 73: 799-805.
- Rowland M G Met al, 1977. A quantitive study into the role of infection in
determining nutritional status in Gambian village children. Br. J. Nut. 37: 441-50.
- Padfield N and Nabarro D, 1985. The management of children with protein energy
malnutrition in Nepal: results of treatment in the Dhankuta Nutrition Unit. J. Inst. Med
(Nepal): in press.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 23 December
1985  4 Page 5 6 4 Page 5 6
| Clear and appropriate messages |
Home fluids: food or drink?
When designing health care interventions, in-depth knowledge of local cultural
attitudes and beliefs is needed. Survey information and results alone may not give the
whole picture. A study carried out in an urban 'shanty town' area near Lima examined mothers' beliefs
and practices during diarrhoea. Using this information, a culturally appropriate
intervention to encourage early home rehydration of children, aged six months to two years
with acute watery diarrhoea, was designed and is currently being tested. From the start,
the study was interested in a local remedy which mothers themselves make at home called
'panetela'. This is made by boiling toasted rice or bread with carrots, water, cinnamon
and sugar. Recent health education efforts have encouraged mothers to add salt, but while
many knew salt should be added, very few actually did it. It seemed that panetela might be
a good 'traditional liquid' to promote for use during diarrhoea, as the survey showed that
over half the mothers said they already used it. It was discovered, however, that panetela was thought to have soothing properties, and
was given to replace milk and the child's normal food during what the mothers perceived to
be severe episodes of diarrhoea. The panetela is usually strained before use and the solid
portion discarded; therefore the actual liquid given has very little food value. The study
showed that, during early diarrhoea, mothers continue to give a near normal diet to the
child until they themselves notice the following danger signs: increased stool output,
stomach pains, loss of appetite, vomiting and fever. These signs of severe illness often
cause mothers to seek medical help. If a mother is asked to give panetela earlier than she
normally would during an episode of diarrhoea, this may unintentionally worsen the child's
nutritional status. The danger of promoting the use of this liquid for rehydration is that
it carries a hidden message: that when panetela is given, other food is avoided.
Therefore, it was decided instead to promote the giving of extra sips of teas and soups
which are part of the normal diet. In this way confusion is avoided when mothers are also
advised to continue feeding their children during diarrhoea. Problems of perception When planning interventions of this type, it is important to take into consideration
such local customs. In this situation the mother may either not comply at all because what
she is being asked to do goes against all her beliefs; or, if she does comply, she may
withhold food as this is traditionally not given at the same time as the panetela. Advice
given to mothers about early rehydration at home must include instructions about
continuing feeding during diarrhoea and giving extra food afterwards. Adequate research
must be done to identify suitable liquids for early rehydration at home. Dr Claudia Lanata and Josephine Gilman SRN, Instituto do Investigation Nutritional,
Apartado 55, Miraflores, Lima, Peru. Promoting ORT correctly
Since it began in 1980, the Jamaican Diarrhoeal Disease Control Programme has
successfully promoted oral rehydration therapy (ORT) throughout the health care system and
the community. Before ORT began to be widely used in Jamaica, mothers tended to respond in two ways
when their children had diarrhoea. They had commonly given the child breastmilk or teas,
black mint or spearmint served sweetened with brown sugar, coconut water or fruit syrup
and water. A few mothers had used 'purging' to give the child a 'good wash-out' and get
rid of the 'bad do-do', and a few also continued to believe that a laxative was
appropriate. In line with this, a recent Jamaican newspaper article recommended the use of
Epsom Salts as a more mild and suitable alternative to castor oil and other strong
laxatives. Misunderstanding advice
In a recent survey of what they do when their children have diarrhoea, we interviewed
mothers in the community and those bringing children with diarrhoea to health centres and
hospital out-patient clinics. The latter group were given oral rehydration fluid for the
child to drink there, a talk from the nurse, and a packet of ORS to take home. They were
told not to use teas or fruit syrup drinks any more, but only the contents of the packet
mixed with boiled water*. To get an additional packet mothers had to invest further money
and time in travel and waiting to obtain one from the health centre or hospital. Although the talk the nurse gave was medically correct, in interviews immediately
afterwards only five per cent of mothers knew that the purpose of the therapy was to
replace fluid. The rest understood the packet as 'medicine' to stop diarrhoea or
facilitate a 'good wash-out' and, of those who had an opinion about the content, 40 per
cent thought it was a laxative salt. Some said 'we used to give mint tea but now we give
salt water' or 'fine salts'. Confusion with other types of salts The salts most widely available in pharmacies are Epsom Salts (magnesium sulphate) done
up in ORS-type packets, Andrew's Salts (magnesium sulphate), Glauber's salts (sodium
sulphate) and other similar preparations. Because reference to oral rehydration 'salts'
reinforces the lay concept of purging with salts, it would seem better in Jamaica for
nurses to talk of an oral rehydration 'drink'. Packets should not be labelled oral
rehydration salts, and also should be made available in the private sector where mothers
can get them with minimum inconvenience. Nurses might also look for new ways to explain to
mothers why they should not purge children with diarrhoea, and use less teaching time
dissuading mothers from using traditional drinks. Carol MacCormack and Alizon Draper, London School of Hygiene and Tropical Medicine,
Keppel Street, London WC1E 7HT, in collaboration with the Jamaican Ministry of Health. *See Editors' note on page 3.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 23 December
1985  5 Page 6 7 5 Page 6 7
Feeding the anorexic child
Children with diarrhoea may not want to eat, yet feeding at this time is
particularly important. Shanti Ghosh suggests ways to overcome
this problem. A child with diarrhoea may lose his appetite (become anorexic) and, as a result, be
difficult to feed. Anorexia can reduce the amount of food consumed by up to 40 per cent.
In many cultures, deliberate withholding of food during diarrhoea is very common and
further reduces intake. In addition, medical advice often supports withholding of food
both during and after diarrhoea, in the belief that food is not absorbed and that the
bowel needs to be rested. This leads to rapid worsening of the nutritional status of a
child who may already be malnourished. Breastfeeding Fortunately, even an anorexic child will usually breastfeed happily. This is because,
as well as nourishment, breastfeeding gives comfort and a feeling of closeness to the
mother which is particularly important when a child is unwell. Studies have shown that the
amount of breastmilk a child takes does not decrease dramatically when a child becomes ill
with diarrhoea. Therefore it is important to continue breastfeeding, even after the age of
six months when diarrhoea is more common. (After six months breastmilk alone is not enough
for the total nutritional needs of the child and additional semi-solid foods should be
given.) As far as possible, this additional food should continue to be given to the child
with diarrhoea, even though the appetite may be reduced. It has now been shown that the
ability of the intestine to absorb nourishment is not greatly diminished in diarrhoea.
 |
Breastfeeding gives comfort as well as nourishment to the sick child.
Even the most dedicated mother may find it difficult to feed an anorexic child; she
will have to use all her powers of persuasion and ingenuity to make the child eat. Often
the child will turn its head away when food is offered, and may not want to eat the usual
family food. The anorexic child may find chewing difficult as not enough saliva is
produced, so rolls the food around in its mouth and either keeps it there or spits it out.
Small quantities of 'soft' foods, which do not need chewing, and which can easily be
swallowed, should be offered frequently. There are suitable foods in every culture. For
example, porridge, gruel, boiled rice, a mixture of rice and lentils, yoghurt, mashed
banana, boiled potatoes or carrots. Fish and eggs can be given where culturally acceptable
and available. A mother needs plenty of patience not to get cross with her child,
especially if she is tired and busy.
|
Give the child the food it wants
|
A mother needs plenty of patience when feeding an anorexic child.
Some children may want to eat savoury foods, and others may prefer something sweet.
Mothers should not be too particular about what the sick child eats, as long as it eats
something. Many mothers have their own ideas about which foods are easily digestible and
which are not. They may insist that a child takes what they consider to be more suitable,
while an anorexic child may have its own preferences. The child may not want to eat bland
or tasteless food, instead it may prefer familiar foods that have more flavour or are
spicy. What is important is that food is eaten, rather than which food.
|
 |
The bulkiness of cereal based foods can be a problem, as a large volume may contain
little nourishment. This can be even more of a problem for the anorexic child. The bulk
can be reduced by roasting the cereal before cooking, or, better still, by malting, a
process involving germination, drying and then roasting again. Adding some oil or butter
will increase the energy density. During the recovery phase of diarrhoea the appetite increases and the mother should
take advantage of this to offer more food to the child. Extra food at this stage is
important as it helps a child's growth catch up some of the loss which occurs during the
illness. Dr Shanti Ghosh, A1/18 Panchshila Enclave, New Delhi 110017, India. The feeding and care of infants and young children, 1985. Ghosh S. Voluntary Health
Association of India (VHAI), C-14 Community Centre, Safdarjung Development Area, New Delhi
110016, India. Price: 14 rupees.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 23 December
1985  6 Page 7 8 6 Page 7 8
Adding to malnutrition
Most episodes of diarrhoea only last for a few days, but diarrhoea persists in an
important group of children. Andrew Tomkins discusses possible
reasons for and ways to manage persistent diarrhoea. Diarrhoea lasting more than fourteen days is usually called persistent (protracted)
diarrhoea (PD). (PD usually develops from acute diarrhoea, whereas chronic diarrhoea does
not necessarily start with an attack of acute diarrhoea.) There have been few prospective
studies on how many attacks of acute diarrhoea go on to PD but results from The Gambia
suggest that it may be up to 10 per cent. PD is often accompanied by severe growth
faltering and the "PD/malnutrition" syndrome is an important cause of death
during the second and third years of life. What causes PD? The main feature is damage to the small and/or large intestine. Several factors are
thought to cause PD:
- Persistent colonisation by a microbe.
Shigella, Salmonella and Campylobacter are important bacterial pathogens isolated in
faecal specimens. Many children have abnormally high levels of E. coli and Klebsiella in
the upper intestine. These may play a role in causing PD. Giardia lamblia, Cryptosporidium
and Entamoeba histolytica may all contribute to PD during an initial infection, but
thereafter, when some immunity has been established, these parasites may not cause so much
damage. No consistent pattern of virus excretion exists.
- Dietary allergies.
Damage to the intestinal lining provides easier access by dietary proteins to immune cells
lying in the intestinal lining. Certain dietary proteins cause a strong immune reaction in
susceptible individuals, releasing chemicals from the immune cells which damage the lining
further. It is important to recognize that reliable diagnosis of dietary allergies is
complex and difficult even in sophisticated paediatric units.
- Carbohydrate intolerance.
Whatever the individual or combined cause of intestinal damage, many children have some
carbohydrate malabsorption during and after diarrhoea - a majority of children in African,
Asian, Latin American and Mediterranean communities suffer a decline in lactase
concentration in the intestinal lining from about four months of age. They are known as
'lactase-deficient' populations - this condition is rare among those of European stock.
Lactase is necessary for the digestion of lactose (the main sugar in milk), splitting it
into glucose and galactose for easy absorption by the small intestine. If undigested
lactose enters the large intestine, it causes watery diarrhoea and abdominal distension
because of an osmotic effect. Lactase deficiency is clinically significant in very
few children, and lactose in small amounts can usually be digested by healthy
lactase-deficient populations; excess lactose may contribute to PD.
(Even severely malnourished children with marked thinning of the intestine and low levels
of intestinal lactase, usually have enough of the enzyme to digest lactose if fed 'little
and often'. Good absorption of food and fast rates of growth can in fact be achieved using
dried skimmed milk as the only protein source - it is best given with sugar and oil to
supply adequate quantities of energy for growth.)
Risk factors in PD Among the risk factors which may predispose to PD are:
- Decreased host immunity,
which reduces the body's defences. Measles, for example, may depress immunity for several
months after the attack, during which time a variety of microbes - (especially Shigella)
can establish a PD. Post-measles PD is well-recognized as a major cause of malnutrition
and death in West Africa. Children with moderate or severe protein energy malnutrition
(PEM) may often develop PD, possibly due to the depressed immunity and decreased gastric
acid production.
- Delayed repair of intestinal damage.
In a well-nourished child damaged intestinal cells are rapidly replaced. However,
nutritional deficiencies such as PEM, or lack of folate or zinc can each slow the rate of
repair.
It has been suggested that other risk factors to consider are: young age; previous history
of diarrhoeal illness; inappropriate drug treatment of acute diarrhoea; disorders of the
pancreas and intestinal mucus layer; and abnormal intestinal motility, especially in young
infants.
Nutritional problems Many children lose weight or stop growing when they have PD because of:
- Reduced food intake.
This is probably the most important cause. Children with PD in The Gambia eat 30 per cent
less than they do when they are well. This decreased appetite may be because the child is
miserable, has abdominal pain, or anorexia, and perhaps fever. Mothers may have firm ideas
about which foods should be avoided during diarrhoea. Individual dietary taboos vary
widely, but the overall result is usually that most children with PD eat less food than
normal, and certainly less than they need to grow.
- Malabsorption.
In spite of intestinal damage and abnormal absorption in PD, the intestine usually absorbs
more than 70 per cent of dietary calories, including most of the protein and fat, even in
cases of severe diarrhoea. In severe cases fat malabsorption may adversely affect the
absorption of certain fat soluble vitamins (especially vitamin A), and xerophthalmia may
develop.
- Intestinal losses.
Loss of blood and mucus from the large intestine is an important precipating cause of PEM.
When fever accompanies the PD, as it may in Shigella infections, extra energy is needed.
Prevention and treatment It is far more difficult to manage PD than acute diarrhoea. It is especially difficult
to evaluate whether treatment is effective as the pattern of diarrhoea in many children is
so variable. Nevertheless there are several steps which can help:
- Prevention.
Proper control of acute diarrhoea is the most effective way to prevent PD developing.
General improvement of hygiene and sanitation, and measles immunization are particularly
important.
- Improved nutrition.
Whatever the cause of PD, it is important to ensure that adequate food intake is
maintained. Mothers may be concerned at the 'waste' of food in diarrhoea and need to
understand that much is still being absorbed. It is also important to advise them to
increase the energy content and frequency of feeds. Any harmful beliefs, about breastmilk
for example, should be corrected.
- Antimicrobials.
Various drugs may be useful. Metronidazole and tinidazole are effective against G.
lamblia, E. histolytica, and certain bacteria which colonize the upper intestine of
children with PD. Children with post-measles PD may be helped by a short course of
ampicillin or cotrimoxazole, if the local antibiotic sensitivity pattern suggests that
Shigella sensitive to these antibiotics may be present.
- Low lactose diets.
If children fed with cow's milk formula are given half strength feeds for a few days, the
diarrhoea may improve. Lactose free milks available commercially are often expensive.
Fermentation of milk (yoghurts), as practised by many traditional communities, reduces the
lactose concentration.
- Exclusion diets.
If the particular cause of any dietary allergy can be established, exclusion diets can be
helpful. Certain cereals may act as dietary allergens, but further research is necessary.
Future developments It is obvious that our understanding of the causes of PD and the best way to manage
such children is unimpressive. At present, we should emphasize careful combined use of:
attention to increasing food intake; and careful, selective use of antimicrobials.
Considerable interest exists in improving the dietary management of PD. Further work on
appropriate exclusion diets for use in poor communities may be valuable. Dr Andrew Tomkins, Department of Nutrition, London School of Hygiene and Tropical
Medicine, Keppel Street, London WC1E 7HT, U. K.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 23 December
1985  7 Page 8 7 Page 8
Doctors still need convincing
I am tremendously impressed by the efforts made by DD to circulate the idea of
ORT in developing countries. But with all this publicity I really doubt if the idea has
penetrated well into the minds of all the medical profession in this country. I enclose
the discharge slip and prescription given for a child who was in hospital for two weeks,
was given various drugs, and it was advised that she stop being breastfed altogether. In
medical colleges, the emphasis is still on drugs and not ORT. Asked what they knew about
ORT, the parents told me that they were given some fluid by the nurse to be given to the
child, without mentioning or showing any interest in what the contents were, and the baby
never took it because of the bad taste. Quite a number of medical officers in rural areas are not convinced of the role of ORT
in preventing dehydration and saving the patient. Also the emphasis continues to be on
drugs and stopping mothers breastfeeding sick children, rather than treating the child
with ORT. Though I cannot suggest any magical remedies, I am convinced that the message has still
to reach many places. Dr E G Suresh, Palace Ward, Alleppey 688 001, India.
Solar dryer for Vitamin A It is unfortunate that in your article on sources of vitamin A in="dd21.htm">Diarrhoea
Dialogue No. 21, you include a picture of what appears to be a type of
solar vegetable dryer that destroys most of the carotene in the vegetables. In the text,
you quite correctly bring out the point that direct solar radiation does the damage, but I
cannot see any way that the air will pass through the dryer, and if it is not so warmed it
will not flow. I suppose that if the frame was covered with black plastic rather than a transparent
surface, it would be satisfactory. We have had some experience here with black PVC tent
dryers into which we place trays of vegetables or fruit for drying. Another possible
design is basically a box in which trays of vegetable matter for drying can be placed,
attached to a panel in which incoming air is heated by direct solar radiation. I favour plastering the lower surface of the heating panel (i.e. the one that absorbs
the incoming heat radiation) with a cement plaster containing enough black oxide to give
it a black colour. This is commonly done in rural kitchens, so the technique is familiar
to the people, the air warmed over this surface will contain no contaminents from the
heating panel. Glass as the upper surface of the panel admits more radiation than
polythene, but is much more expensive. I hope my brief comments will ensure that none of your many readers who, like myself,
find DD such a valuable source of information, get the wrong idea from that
picture. Brian McGarry, Silvira House, Development Education Centre,
Chishawasha, PO Box 545,
Harare, Zimbabwe.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Editor Kathy Attawell
Editorial assistant Maria Spyrou Editorial advisory group
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Professor Leonardo Mata (Costa Rica)
Dr Mujibur Rahaman (Bangladesh)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), UNICEF and WHO
|
Issue no. 23 December 1985
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
updated: 23 April, 2014
|