|
| |
Issue no. 15 - November 1983
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
updated: 23 April, 2014
Pages 1-8
Diarrhoea Dialogue Online Issue 15 -
November 1983
|
DDOnline
Diarrhoea Dialogue Online Issue 15 November
1983  Page 1 2
Page 1 2
Dangerous partners
The problem continues of how to make both sufficient food and good nutritional
knowledge available to the many families who need this help. Diarrhoea and malnutrition are dangerous partners, responsible for a vicious downward
spiral of ill health which too often ends in death for millions of Third World children.
The large number of watery stools that occur in diarrhoea cause dehydration which may in
turn lead to failure of the blood circulation and fatal shock. Rehydration - replacement
of the lost body fluids and salts - greatly reduces this immediate danger. Prompt oral
rehydration will save the lives of many children. Progressive malnutrition is a less obvious but equally serious risk among continually
undernourished children for whom diarrhoea is a frequent illness. Among poor communities
this kills as many children as does the more dramatic dehydration. Dialogue on nutrition
 |
Breastfeeding contributes greatly to the prevention of diarrhoea. From the first issue of DD in May 1980 we have emphasized the crucial
role of breastfeeding - both in preventing diarrhoeal infections and in reducing their ill
effects. We have also discussed other important aspects of the feeding of children (see
news page). Readers' letters show us that reliable information is badly needed about when,
how and with what types of food they should feed children who have diarrhoea.
|
Local traditions about this important aspect of treating diarrhoeal diseases vary
widely from good to harmful beliefs. We would like to hear more about the customs in your
area. Food for thought
|
Cereal gruel, inadequate nutritionally, is given as
weaning food in many places. Interesting new scientific evidence is now emerging about the extra value of enriched
rehydration solutions (see="#page4">page four). Equally, researchers are
emphasizing the importance of ensuring that children are given adequate food both during
and after diarrhoea to avoid unnecessary setbacks in growth and development. This
issue of Diarrhoea Dialogue focuses on the significant relationships between
diarrhoeal infections, malnutrition and feeding practices.
|
 |
K.M.E. and W.A.M.C.
|
In this issue...
- Nutritional value of ORT
- Weaning and diarrhoea
- Health education in North Yemen
|
|
DDOnline
Diarrhoea Dialogue Online Issue 15 November
1983  1 Page 2 3 1 Page 2 3
DD on nutrition and diarrhoea
|
Nutrition is a family responsibility
Earlier issues of Diarrhoea Dialogue have looked at a wide range of
issues connected with diarrhoea and feeding practices. For example:
- Breastfeeding problems (issues 1 and 2)
- Diarrhoea-malnutrition complex (issues 3, 6
and 12)
- Infant food and weanling diarrhoea (issue 2)
- Persuading children with diarrhoea to eat (issue 6)
- Feeding and chronic diarrhoea (issue 10)
|
 |
We can supply copies of these articles if you have missed them. Write to Diarrhoea
Dialogue, 85 Marylebone High Street, London, W1M 3DE, UK. "Power food"
The Mass Media and Health Practices Project in The Gambia (described in Diarrhoea Dialogue 14) has recently begun a rainy season feeding
campaign. Evaluation from the first year of the project showed that the promotion of
'feeding solid foods during diarrhoea' had not been as well accepted as the oral
rehydration message. It was thought that this was due to Gambian mothers' understandable
difficulty in feeding their sick children because of the anorexia associated with
diarrhoea. Since the beginning of the rainy season (and diarrhoea season) in The Gambia this June,
the Mass Media staff have been promoting a different feeding message, emphasizing solid
foods for a child recovering from diarrhoea. Specific energy-rich local
foods such as boiled or steamed rice and millet with oil-based sauces - are being
recommended. A slogan calling these dishes 'power foods' in the local Wolof and Mandinka
languages is being used to popularize them in the campaign radio programme and graphic
materials. The two main pictures being used are a poster for health workers and a handbill
which health workers distribute, after explanation, to mothers. Project staff hope that
these changes in the feeding messages will encourage the mothers to rely less on the
watery paps they often feed their children when they are ill and to concentrate more on
energy rich solid foods. Mark Rasmuson and Nigel Taylor
Teaching mothers The Voluntary Health Association of India (VHAI) has produced a small booklet for
health workers who teach mothers about prevention of diarrhoea and the use of oral
rehydration therapy. The booklet, called Better care during diarrhoea, describes
what diarrhoea is, why it is dangerous and what mothers should do about it. It also
explains clearly at what point a mother has done all she can and should take her child to
the health centre. It has pictures for discussion and questions and answer pages to
develop better understanding about oral rehydration therapy and the prevention of
diarrhoea. If you would like to see the booklet write to VHAI, C-14 Community Centre, SDA, New
Delhi 110016, India.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 15 November
1983  2 Page 3 4 2 Page 3 4
Reviews
- Diarrhea and malnutrition: Interactions, Mechanisms and Interventions
Chen L C and N S Scrimshaw (editors) Plenum Press, New York, 1983
- Acute Diarrhea: Its nutritional consequences in children
Bellanti J A (editor) Nestle Nutrition Workshop Series, Vol 2,1983, Raven Press,
New York
These two recent publications emphasize the current interest in nutritional aspects of
diarrhoeal disease. The first reports a workshop held in Bellagio in May 1981, and the
second a workshop held in Washington a year later. There is a considerable overlap in the
participants and material, but the Chen and Scrimshaw workshop invited more Asian
participants while the Bellanti meeting contained mainly scientists from North and Latin
America. Both books review the pathophysiology and mechanisms of the interaction between
nutrition and diarrhoea, but Chen and Scrimshaw also consider possible interventions with
a view to policy planning and implementation under the following four headings: diarrhoea
and nutrient requirements; therapeutic interventions; prevention and control of diarrhoeal
diseases; and diarrhoea and malnutrition. These chapters are a valuable source of ideas
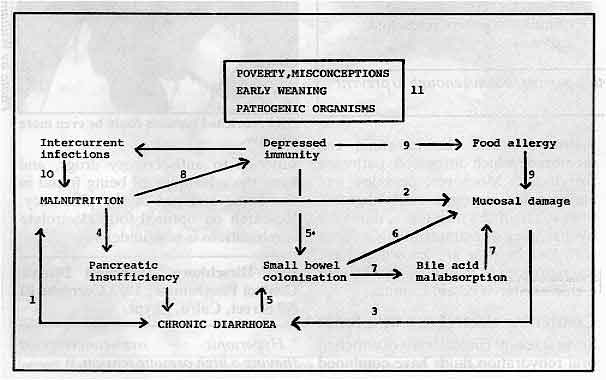
for both research and action. Commonwealth meeting in 1984 Paediatricians from Australia, Bangladesh, Canada, India, Malaysia, Nigeria and
Singapore are planning a meeting to be held in London on 5-7 November, 1984. The aim of
the meeting is to promote a closer dialogue about diarrhoea and malnutrition in childhood;
to catalyse further research collaboration; and to encourage a greater exchange of ideas
and expertise to improve child health throughout the Commonwealth - and the world. It is
hoped that the published proceedings will become an effective guide for better treatment
and prevention at all levels. The model below is proposed for the meeting and the idea is
to test the validity of each link.
Contributions welcome As well as 12 main speakers, a number of short papers (10 minutes) will be scheduled
for the ample discussion times. Membership will be limited to 150. Commonwealth citizens
interested in contributing on any aspect should send two copies of their abstracts to the
address below by 2 January 1984. Dr J. A. Walker-Smith, Reader in Paediatric
Gastroenterology, Academic Department of Child Health, Queen Elizabeth Hospital for
Children, Hackney Road, London E2 8PS, UK. Dr Cicely Williams
|
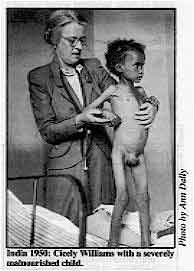
India 1950: Cicely Williams with a severely malnourished child. Dr Cicely Williams celebrates her 90th birthday on December 2nd, 1983. Her biography
has just been published by Green College, Oxford, UK and costs £12.50 ($ 25.00). Famous
for her identification of kwashiorkor (protein energy malnutrition) in West Africa fifty
years ago, Cicely Williams has never ceased to promote the cause of mother and child
health and is known and loved throughout the world. Appropriately, this issue of Diarrhoea
Dialogue re-examines the importance of good family feeding practices in
relation to diarrhoea. Many of our readers will undoubtedly wish to join in a special
birthday greeting and congratulations to someone who believes that 'mother and the
mother's lap are the best accompaniments to oral rehydration' (Diarrhoea
Dialogue 3, page 8).
|
 |
In the next issue ...
Diarrhoea Dialogue will look at the relationship between measles and diarrhoea
in childhood. Vaccination against measles has many benefits if given correctly. We will
therefore also consider the practical problems of carrying out immunization programmes.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 15 November
1983  3 Page 4 5 3 Page 4 5
| Food is good for diarrhoea: when and how? |
Enriched ORT
Bert Hirschhorn considers the nutritional value of oral
rehydration therapy. Mothers and doctors alike have long believed that to feed a child with diarrhoea makes
the condition worse. Those who insisted that malnourished children ought not to be starved
did so apologetically, accepting a lesser risk. Now we are told that continued feeding is
good even for the adequately nourished. Why such a change in advice? It was oral
rehydration therapy (ORT) with the full formula that made this feeding possible. Contrast
the considerations before and after ORT was introduced:
| Before |
After |
| 1. A child with diarrhoea feels sick and loses
its appetite. |
1. ORT reduces nausea and vomiting and restores
appetite*, partly through rapid correction of acidosis, hypotension and potassium losses. |
| 2. Food, especially milk, increases diarrhoea
through osmotic fluid loss due to incomplete digestion after damage to intestinal enzymes.
|
2. Glucose-salt solution given as well as milk
increases absorption and decreases osmotic fluid loss. |
| 3. If food is withheld, diarrhoea was thought to
slow or stop. (This was only partly true, for diarrhoea results from intestinal secretion
which occurs independently of the digestion of food.) |
3. With easy and rapid replacement of fluid loss
by ORT, we are less concerned about stopping the diarrhoea immediately. Food is needed for
recovery and to stimulate digestive juices and enzymes. |
| * Some decrease in appetite and absorption persists, but
not enough to prevent adequate nutrition. |
So now we can feed during diarrhoea and protect children from
under-nutrition, without apologies. Another use for foods In the course of clinical experience, however, another use for food has been suggested.
As early as 1971, after initial rehydration of American Indian children suffering with
diarrhoea, an artificial milk formula made up from starch, glucose, casein, with medium
chain fats and electrolytes, could maintain fluid and electrolyte balance in spite of
continuing losses. The formula was effective, despite being hypertonic* and with a large
imbalance between sodium and glucose concentrations, conditions normally causing more
diarrhoea and fluid loss.
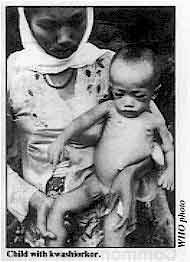 |
Child
with kwashiorkor.
Modern understanding of intestinal physiology suggests that it was the addition of
casein (milk protein) that made the difference. Casein is easily digested to tri- and
di-peptides and amino acids. Each of these molecule types stimulates sodium and water
absorption by pathways across the intestinal cell membrane which differ from pathways for
glucose. Moreover, peptides, and amino acids are more easily digested than sugars if the
intestine is damaged by diarrhoea or malnutrition. Children with kwashiorkor are known to
have less diarrhoea or malnutrition when fed a glucose-starch-casein formula.
|
Combining electrolytes with foods Several recent clinical trials of enriched oral rehydration fluids have combined a
sugar and an amino acid (glucose and glycine), or starch and protein (rice powder and
breastmilk) with electrolytes. In each study, stool output was actually reduced by about
half and duration of diarrhoea shortened by one third.
|
ORT:
enriched versions could be even more effective. This is just what mothers and doctors have always wanted: a treatment that prevents
dehydration, reduces stool output and, at the same time, provides the nourishment to
hasten recovery. Certain foods, in an enriched ORT, may turn out to be superior to
antisecretory drugs, and have the advantage of being found in the home and not in the
pharmacy. Research on optimal food-electrolyte combinations is now underway.
|
 |
Bert Hirschhorn, Diarrheal Disease Control Programme, 1053 Corniche El Nil Street,
Cairo, Egypt. * Hypertonic - over-concentrated (having a high osmotic tension.)
|
|
DDOnline
Diarrhoea Dialogue Online Issue 15 November
1983  4 Page 5 6 4 Page 5 6
| Food is good for diarrhoea: when and how? |
Carry on feeding
In communities where malnutrition is common, correct feeding is as important as
rehydration for children who have diarrhoea. We report on studies from Bangladesh
illustrating this point. A recent careful survey of young children in Bangladesh revealed that, on average, each
child suffered 6.8 episodes of diarrhoea per year. Added up, this meant they had diarrhoea
for 55 days or 15 per cent of the year(1). Such children will end up severely deprived of
nourishment if they are starved all the time they have diarrhoea. Although digestion is
less effective during diarrhoea, there is still a significant amount of absorption of
nutrients. The Dhaka work has shown that, in children given as much ordinary food as they
will take, the amount of protein absorbed is reduced to about 50 per cent, the amount of
fats to 60 per cent and the amount of carbohydrate to 80 per cent (2). This fall in
digestive efficiency varies to some extent with the cause and mechanism of the diarrhoea,
but the figures show that, in spite of the disease, the children manage to absorb valuable
amounts of essential nutrients. Breastmilk - energy value
Another Bangladesh study compared the normal dietary intake of small children with
diarrhoea with that of a group of matched controls. The energy intake of the ill children
was reduced by 40 per cent, but among those children who were being breastfed, the energy
intake from mother's milk showed very little decrease (3). This suggests that the loss of
appetite is mainly associated with supplementary foods. Breast milk is therefore a
particularly valuable nourishment for children with diarrhoea, especially among deprived
communities where it may be the main source of high quality protein. Every effort ought to
be made to continue breastfeeding during diarrhoea, not least because breastmilk supplies
depend on the stimulus of sucking. If breastfeeding is interrupted every time diarrhoea
occurs, there will soon be much less of this important food available for the child at the
time of greatest need. Which foods and when?
 |
Correct feeding is as important as rehydration for
children with diarrhoea. Despite recent studies, unanswered questions remain about what are the best foods to
offer during diarrhoea and when to introduce them. In acute diarrhoea, most foods can be
given safely and soon. In chronic diarrhoea, feeding may be more of a problem (see="dd10.htm">Diarrhoea Dialogue 10 for Professor G. C. Cook's article on
causes and control of chronic diarrhoea). Mother's milk is better tolerated than cow's
milk and breastfeeding should continue during diarrhoea. Children with diarrhoea who are
being bottle-fed need to have the formula diluted with an equal volume of water while the
diarrhoea continues.
|
|
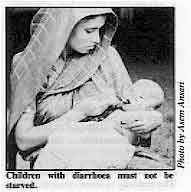
Children
with diarrhoea must not be starved.
The important point is to start giving small, frequent feeds of a familiar diet as soon
as rehydration is complete, preferably mixed with a little extra vegetable oil to increase
the energy content. Vitamin A supplementation is required in areas where xerophthalmia
(night blindness) is common.
During convalescence after diarrhoea, children need extra food for 'catch-up' growth.
This can be given as nutritious snacks between meals or as an extra meal every day for
several weeks.
|
 |
Compiled by the Scientific Editors from information provided by A. and A. M. Molla,
ICDDR, B, Dhaka, Bangladesh. (1) Black R E et al 1982 Longitudinal studies of infectious diseases and physical
growth of children in rural Bangladesh. I Pattern of morbidity. American Journal of
Epidemiology 11 5, 3: 3 0 5-31 4.
(2) Molla A et al 1983. In Diarrhoea and malnutrition. Plenum Press, New York.
(3) Hoyle B et al 1980. Breastfeeding and food intake among children with acute
diarrhoeal disease. American Journal of Clinical Nutrition, 33: 2365-2371.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 15 November
1983  5 Page 6 7 5 Page 6 7
Breast to family diet
Weanlings are particularly vulnerable to infection. Michael Gurney
considers how this important time can be made safer and more beneficial for the baby. Weaning does not refer only to the stopping of breastfeeding. It is the gradual process
by which a baby becomes accustomed to semi-liquid and solid foods which increasingly
complement breastfeeding. It is complete when the child is eating the regular family diet
and breastfeeding has completely or nearly stopped. Phrases such as "the baby
should be weaned at six months" can be very misleading. Weaning is one of many changes that all take place together. The weanling child is
becoming accustomed not only to new foods but to a new environment and to new physical and
mental skills. He is very vulnerable to illness at this time. When should weaning start? The best way to wean varies according to the circumstances of each family. If a mother
has to go out to work she may have to start giving extra foods earlier than is best for
the baby, while continuing to breastfeed whenever she is at home. Where sanitation and
cooking facilities are poor, she may be wise to start weaning foods later than is ideal. In general, breastmilk is perfectly adequate until the baby is at least four to six
months old, or weighs about seven kilograms. Other foods need to be introduced about this
time to complement breast milk. They are unnecessary, and can be dangerous, if given
earlier. What makes a good weaning diet? Texture:
At first, the baby needs liquid foods. These become thicker until, by his first birthday,
he is able to chew pieces of food. A good practice is to start with a porridge or pap
containing the food ingredients mixed together into a creamy consistency. Quantity:
Babies have very small stomachs and are growing very fast. They need small amounts of
foods which are rich in dietary energy. Little and often is the rule.
|
Small, frequent meals.
At first weaning food is extra to breastfeeding; as time goes on it becomes the main
food, and breastfeeding becomes less important. The frequency of feeding should increase
rapidly until the baby is soon taking at least five meals a day plus
breastmilk. Feeding
should continue at this rate well into the baby's second year. Snacks, such as fruit,
between meals are useful - as long as they are always clean.
|
 |
Quality:
Most weaning diets around the world are based on starchy staple foods such as rice,
potatoes and cassava. This is fine as long as certain precautions are taken. Such staples
are not nutritious enough in themselves. A porridge using the staple mixed with
something extra is excellent. The best additions are peas and beans mashed with the skins
removed; milk; meat (finely chopped) or other animal foods; plus dark green leafy
vegetables or yellow-orange fruits such as papaya and mango. Suitable recipes and methods
of preparing weaning mixes can be found and developed in most cultures. Energy supplement:
Many weaning porridges do not contain enough energy for the baby's needs. During cooking,
the starch used in the porridge takes up water and becomes very bulky. Extra oil added to
the porridge has two benefits: it adds energy (oil is very rich in calories); and the oil
changes the consistency of the porridge, making it easier for the smallest babies to
swallow. Oil should be incorporated in all weaning foods except where obesity is a
problem. Two other ways of reducing the bulkiness of weaning foods and making them better and
easier for the infant are fermenting or roasting the staple grains. This is done in some
parts of the world and can be of great benefit. Economy:
If people spend extra money to buy special weaning foods they are likely to give too
little in order to make it last. Weaning foods made at home can be just as good as those
bought from shops. In fact, some products sold for babies are very poor in nutritional
quality. It is usually best to rely on foods available from the family pot. Hygiene:
Contaminated food is one of the most critical problems during the weaning period. In poor,
unsanitary environments it is very difficult to avoid diarrhoea in young children.
Breastfeeding provides a major protection against diarrhoea. Good hygiene is essential in
preparing weaning foods and keeping them until the next feed. But it is difficult to feed
a baby five or more uncontaminated meals a day, when the mother can only afford to light
the kitchen fire once. Local technologies need to be used to resolve the problem. Utensils:
Bottles and rubber teats are difficult to keep clean. Moreover, in order for a weaning
porridge to pass through the teat it has to be very dilute; therefore the baby risks not
getting enough food. It is best to keep suckling from the breast, not the bottle.
When food is mashed for a baby, avoid using sieves which are difficult to clean. A cup and
spoon are suitable for giving weaning foods; this allows the mother to change the food
from liquid to semi-solid as the baby grows. Breastfeeding:
Breast milk is very nutritious and protects against infections. It also provides the
close, loving contact that encourages secure development. As far as possible,
breastfeeding should continue throughout the difficult process of weaning. Dr Michael Gurney, Nutrition Unit, WHO, CH-1211 Geneva 27, Switzerland.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 15 November
1983  6 Page 7 8 6 Page 7 8
Combining science with tradition Christine Ansell and Pauline Wright
describe health education in North Yemen that combines new health practices with
traditional beliefs. Diarrhoea associated with bottle-feeding is a major killer of young infants in North
Yemen. Even in very remote areas bottle-feeding is widely advertised and used by mothers.
The feeds are often made up incorrectly, with dirty water. In a situation like this,
health education is obviously essential. However, it is wrong to think that as soon as
people are given proper information about a health problem they will forget old beliefs
and follow the new set of rules. One way of approaching this is to base a health education
programme on both scientific fact and local health beliefs. We describe
two examples of this approach below: Breastfeeding Recently one of us watched 'one to one' health teaching in a clinic for mothers of
babies with diarrhoea, in which the nurse was emphasizing the superiority of
breastfeeding. The usual routine was followed: Nurse: Are you breastfeeding your baby?
Mother: No, bottle-feeding.
Nurse: You know that breast milk is better for your baby . . . it contains
antibodies against diarrhoea . . . it does not cost money . . . it is from God . . . it is
cleaner and easier . . . etc.
Mother: But I do not have enough milk. The nurse then shows the mother a picture of a healthy fat baby feeding from the
breast, and another of an under-nourished baby lying next to a bottle.
 |
In this Egyptian community breastfeeding is routine. Elsewhere,
as in North Yemen, mothers need to be convinced of its merits. The parents listened patiently to the nurse, but they had heard these messages before
and it was clear that they were not convinced. By chance, another nurse came into the
clinic and listened for a while. Suddenly, and quite without emphasis, she said 'you know,
nowadays men are growing up without close bonds with their mothers, because they were not
breastfed. ' The couple responded to this with a very lively interest and were obviously
giving the idea careful thought and consideration, and clearly thinking that it could be
true.
|
The idea suggested by the second nurse has semi-magical overtones normally found in
concepts about health common amongst people unfamiliar with western medicine. It might,
therefore, have an appeal built into it which would be helpful in producing the right
behaviour. Oral rehydration therapy
The second example occurred after a teaching session about oral rehydration therapy
with primary health care trainees, who were then asked to teach the mothers in the clinic.
Suddenly the whole scientific emphasis was switched around. One trainee, instead of
relaying the facts as she had been taught, began talking in terms of 'cleaning the
stomach. ' Contrary to previous sessions with mothers, which concentrated on teaching
about giving replacement fluids and salts, this produced lively interest and discussion.
Salt is a well-known cleanser in North Yemen and the ORS mixture was being advised as one
which would cleanse the stomach and therefore cure the diarrhoea. Surely the essential
point is that use of ORS is taught and demonstrated correctly. The underlying reason for
its acceptance is less important. And it is obvious that these mothers had a theory of
their own which made ORS acceptable. These examples provide clear instances of other approaches to reasoning which, if used
in health teaching, will encourage better acceptance of important practices such as
breastfeeding and oral rehydration therapy. Christine Ansell, Nutritionist, Oxfam and Pauline Wright, Public Health Nurse, WHO.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 15 November
1983  7 Page 8 7 Page 8
Information through illustrations
I am a Peace Corps Community Health Volunteer working in Sierra Leone, West Africa.
Very occasionally I have found old issues of Diarrhoea Dialogue in our Peace
Corps office. They have proved to be informative and extremely useful, especially when
passed to my counterparts in the Ministry of Health and the Ministry of Social Welfare.
It's a definite motivator for the health workers here to see that they are not alone with
their troubles; and especially to learn techniques that they can use, like ORT. However, it is difficult for us here in the Eastern Province to receive Diarrhoea
Dialogue on a regular basis. We presently have ten PC CHV's in the East. And
we all have Chiefdom Health Overseers or Public Health Inspectors as counterparts.
Together we work with social welfare workers and village health committees. So if we could
get 10-12 copies sent directly to Kenema I feel that we can guarantee widespread
distribution of the ideas and techniques presented in DD.
 |
Pictures
liven up a nutrition class in Papua New Guinea. I do have one suggestion. Pictures are invaluable to any health lesson. Do you think it
would be possible to run one full page picture or illustration in each issue? When working
across the bilingual border one picture is truly worth a thousand words. Any help will be
appreciated. Thanks again for what you have already helped us to do.
|
Tom Bik, PCV Taninahun, c/o Mr J. S. Conteh, Senior Health Inspector, Ministry of
Health, Kenema, Sierra Leone, West Africa. Lines of communication I would like to make one comment about Diarrhoea Dialogue 13that mentioned the four UNICEF priorities to save the 15,000 (or was it 20,000?)
children each day from dying from diarrhoea with dehydration and malnutrition - the use of
the growth charts, oral rehydration, immunizations; and I think the final one was
breastfeeding. Not one of these priority items is new but, in spite of this, the message
is still not getting to the target population. Perhaps if all the available lines of
communication are used, then it will work. Learning the very ordinary things about daily
survival are often the most difficult ones to get straight. With thanks to you for your very clear and lucid way of presenting material that all of
us ought to know. Myrtle Elizabeth Keller, MD, Kamuzu Central Hospital, P. O. Box 149, Lilongwee,
Malawi, Central Africa.
Using DD for surveys I am a final year medical student at Ghana Medical School. I came across an issue of Diarrhoea
Dialogue (issue No 9, May 1982) at Danfa, a rural suburb
near Accra, whilst doing my Sub-internship in Rural Medicine there. I was so impressed
with the publication that I read it cover to cover! The practical advice series column
gave me enough information to carry out a survey on mothers' attitudes to diarrhoea in
Bawku District, Northern Ghana. I used the results as my dissertation in partial
fulfillment of the Final Part II Examinations in Community Health 1983 for the award of
MB. ChB degree. I would also be very pleased if you could regularly supply me with Diarrhoea
Dialogue and any other publications which will help in my full understanding of the
problems of diarrhoea and its management. Frank K. P. Nyonator, C2/W1 Students' Hostel, Ghana Medical School,
Korle-Bu Teaching Hospital, Korle-Bu, Accra, Ghana.
DD for extension workers
I should be very grateful if you could include my name on your mailing list to receive
the Diarrhoea Dialogue. I'm an Agricultural Extension Officer working in a Joint Oil Palm Project financed both
by the World Bank and the Government of Ghana. I work in rural areas, that is farmers who
have their own lands and are interested to participate in the project known as the
Outgrowers. I work in a 50 kilometers radius from the main plantation. Diarrhoea Dialogue would
benefit me a lot during my usual rounds to the villages. As an Extension Worker, I should
know something about health education and pass on the knowledge to the rural dwellers,
especially where health posts and clinics are not available. J. N. Asiedu, GOPDC - (Kwae Plantation), P. O. Box M428, Accra, Ghana.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Executive editor Denise Ayres Editorial advisory group
Professor David Candy (UK)
Dr I Dogramaci (Turkey)
Professor Richard Feachem (UK)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr D Mahalanabis (India)
Professor Leonardo Mata (Costa Rica)
Dr Mujibur Rahaman (Bangladesh)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from WHO, UNICEF and SIDA
|
Issue no. 15 November 1983
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
updated: 23 April, 2014
|