|
| |
Issue no. 41 - June 1990
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
updated: 24 April, 2014
Pages 1-8 Dialogue on Diarrhoea Online Issue 41 - June 1990
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 41 June 1990
 Page 1 2
Page 1 2
ORT today and tomorrow
Infant and young child mortality could be greatly reduced if people used oral
rehydration therapy correctly and often enough. DD, celebrating ten years of
publication with this issue, has always reported on efforts to prevent and treat
diarrhoeal diseases. Promotion of ORT has been one of the main functions of the
newsletter. Global production of ORS is now more than 350 million packets a year, and access to OR
therapy has increased considerably in the last decade. At the same time, CDD programmes at
all levels have made great progress in spreading messages about interventions which can
prevent diarrhoeal diseases. More and more families and health workers have learned to use ORT, and many deaths have
been averted. It has also become increasingly clear that giving home fluids early to
prevent dehydration and continuing to give nutritious foods is the best way to prevent a
case of diarrhoea from becoming serious. Still much to be done Despite these efforts, four million children a year still die from diarrhoea. ORS
packets are not available to every child in need of treatment for dehydration. Families in
remote areas may not be able to obtain the packets, and poor families may not be able to
pay for them. In addition, while standard ORS treats dehydration effectively and safely, it does not
stop the diarrhoea, which is almost always the first concern of mothers. For this reason,
some health professionals and families still remain unconvinced about the benefits of ORS,
and tend to give dangerous and ineffective drugs. Recent research suggests that cereal
based ORS formulations reduce stool volume and duration of illness (see="#page4">pages
4 and 5). Therefore, cereal ORS could be promoted as having an
anti-diarrhoeal effect, which might lead to reduced use of inappropriate drugs. Home management Most cases of acute diarrhoea, if handled properly and early enough at home, will not
require treatment with ORS. Home management should be based on giving extra amounts of
safe fluids together with continued feeding with the child's normal diet.
|
To treat diarrhoea at home, give extra fluids and
continue giving nutritious foods. The choice of home fluids will depend on local circumstances. In some areas, sugar-salt
solutions have been used successfully, but in others there have been problems with
dangerous and ineffective solutions caused by incorrect mixing.
|
 |
Similarly, cereal-salt solutions have advantages and disadvantages. If made with local
staple foods, they are cheap, easily available, culturally acceptable and more likely to
be given earlier in the illness. Also, there is no risk of the osmotic diarrhoea
associated with solutions made with too much sugar. If too much cereal is added to an oral
rehydration solution, it becomes too thick to drink. However, it is most important that
cereal based ORT solutions are not confused with food, and that mothers do not dilute the
child's usual foods to make home fluids (For the latest guidelines from the World Health
Organization on the selection of home fluids, see="#page2">page 2). KME, WAMC and KA
|
In this issue:
- Home fluids for diarrhoea
- Cereal based ORT - research reports
- Practical advice on cup feeding
- Potassium - questions and answers
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 41 June 1990
 1 Page 2 3 1 Page 2 3
Selection of home fluids Home treatment of acute diarrhoea should:
- prevent dehydration by giving increased fluids; and
- maintain nutrition by continuing to breastfeed or by giving acceptable, nutritious
foods.
ORS solution made from a packet of oral rehydration salts is designed to treat
dehydration, but can also be used to prevent it. Where ORS is not available, other fluids
should be used to prevent dehydration. Fluids recommended, in addition to
breastmilk,
include:
- sugar-salt solutions
- food based fluids, such as cereal gruels or soups
- plain fluids such as water or weak teas without sugar.
Sugar-salt solutions
Experience in many countries has shown that families may be unable to make special
fluids correctly. Some ingredients may not be available; it may not be possible to carry
out the careful measuring needed; or the recipe may be forgotten over time. Sugar-salt
solutions (SSS) made with too much salt or sugar are potentially dangerous for young
infants. Also it has been found that many families view SSS as 'medicine', and so too
little fluid is often given too late. Food-salt solutions Food-salt solutions could provide an alternative to SSS. They can be made from ordinary
ingredients and might be more likely to be given in larger amounts. Food-salt solutions
could include commonly available fluids looked on as drinks, which are familiar, easy to
prepare and acceptable for giving to children with diarrhoea. Such drinks include food
based fluids which contain cooked starch and protein, such as cereal soup or porridge. The
addition of salt (up to 3g/l) would increase their effectiveness for ORT. Food-salt
solutions may also promote sodium absorption more effectively than sugar-salt solutions
because they contain more of the carrier molecules (glucose and amino acids derived from
starch and protein) necessary for water and salt absorption in the gut. This means that
food-salt solutions may decrease stool output and reduce losses of salt and water. Whether or not mothers should be encouraged to add salt to food based fluids will
depend on the amount of salt usually included in food for children, and the feasibility of
teaching mothers to add the right amount of salt. If food based fluids are recommended for diarrhoea, it is important that families do
not confuse fluids for rehydration with food, and that children with diarrhoea are given
enough to eat. It is not recommended that children be given watered down versions of
thicker foods which are part of the normal diet. Food based fluids should be given in
their usual form, except for the addition of salt if this is necessary. Messages about
appropriate feeding as well as giving suitable fluids should continue. Familiar drinks Another approach is to promote drinks which are familiar and commonly available, but
which contain no added salt and relatively little starch or protein. These include weak
cereal solutions such as rice water, water in which other cereals have been cooked, and
plain water. These solutions do not provide the salt, starch and protein necessary to
prevent dehydration in cases of large stool losses. But they would adequately replace
losses in most cases, especially if given as well as foods that contain some salt. Use of
such drinks should be considered when the use of food based fluids containing salt is not
feasible.
|
Prevention or treatment? To treat dehydration, once it has developed, it is essential to replace water
and salts lost during diarrhoea. Giving the standard WHO/UNICEF formula ORS is the best
way to do this, because it provides exactly the right balance of glucose and salts. Other
solutions containing the right amounts of sugar and salt, such as a carefully measured
sugar-salt solution, are also good. It is always better to give fluids of some sort than
not to give fluids at all. To prevent dehydration, the formula of solutions given is less important: the
main thing is to give extra fluids as soon as diarrhoea begins, and to continue feeding.
Home management is important because, if effective treatment for diarrhoea is given at
home, dehydration can be prevented in many cases. What about cereals? Oral rehydration solutions made from the same formula of salts as WHO/UNICEF glucose
ORS, but with rice powder instead of glucose, have proved effective in treating
dehydration. More research is, nevertheless, needed on some aspects of cereal based ORS
before it can be widely promoted. Home made cereal based fluids have also been found to be
at least as good as other home fluids for ORT.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 41 June 1990
 2 Page 3 4 2 Page 3 4
Recommendations
 |
Always
continue breastfeeding a child with diarrhoea.
1. Home fluids to prevent dehydration (in order of effectiveness) include:
- oral rehydration salts (ORS) solution (although designed to treat dehydration, ORS may
be used, if available, as a home fluid from the start of diarrhoea to prevent dehydration)
- food based fluids (such as soups and porridges)
- sugar-salt solution
- other drinks (including plain water)
Food should always be given as well, with all of these fluids. |
2. Any home fluids used should be:
- readily available - easy to make from cheap, widely available ingredients
- safe - so that the recipe will not contain too much salt (or sugar) even if it is only
followed approximately
- familiar - the fluid or recipe should be well known
- acceptable for use during diarrhoea - with acceptable taste and no cultural barriers
- easily and readily given in large enough quantities
3. Home fluids should contain salt if possible. Otherwise, salt can be given in food.
Unsalted fluids should still be given if it is not possible or practical to give fluids
containing salt.
4. For food based fluids, it is usually best to use recipes which normally include a
safe amount of salt. Otherwise, salt can be added, if this is practical - 3g of salt per
litre of fluid is ideal (but up to 6g per litre would still be safe).
5. If sugar-salt solution is used, a recommended composition is 50
mmol/litre of salt
and of sugar (3g of salt and 18g of sugar per litre of water).
6. Home fluids should not be prepared by diluting weaning foods.
7. When food based fluids are used for home treatment, it is very important to make
sure that they are not regarded as food, because this could result in a sick child getting
too little to eat. These guidelines and recommendations were developed at an international meeting of
experts held by the World Health Organization in Baltimore, USA, in March 1990. How to make a rice based drink for oral rehydration
With careful teaching and practice, mothers in Pakistan have learnt to make this
safe and effective rice based drink for oral rehydration.
|

|
1 Take one handful (20 to 25 grams) of rice grain. Wash and soak the rice in water until
it is soft. |
|

|
2 Grind the soaked rice with pestle and mortar (or any other grinder) until it becomes a
paste. |
|

|
3 Put two and a quarter glasses of water (about 600ml) into a cooking pot and mix in the
rice paste. |
|

|
4 Stir well, and heat the mixture until it begins to bubble and boil. Then take the pan
off the fire, and leave the solution to cool. |
|

|
5 Add one three finger (up to the first finger joints) pinch of salt (1.5 grams) to the
mixture, and stir well. The solution is now ready to be given to the person with
diarrhoea. |
Storage: this solution should be covered and kept in a cool clean place. It should be
used not more than six to eight hours after preparation. After this time, throw away any
solution which is left over. Pictures and text taken from Elliott, K, et al. (eds), 1990. Cereal based oral
rehydration therapy for diarrhoea (symposium report), page 51. Aga Khan Foundation and
International Child Health
Foundation. See="#page5">page 5 for publication details. Further reading: Molla, A M, et al., 1989. Food based oral rehydration salt
solutions for acute childhood diarrhoea. Lancet ii: 429-31.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 41 June 1990
 3 Page 4 5 3 Page 4 5
Cereal based ORT DD presents short reports of four recent studies. Sorghum ORS: Rwanda
Sorghum flour is the main ingredient of traditional weaning foods in Rwanda. It was
tested as a base for ORS in the treatment of 100 children with acute diarrhoea. The
children included in the study were boys with good nutritional status, aged six to 24
months, who had had diarrhoea for less than three days with moderate dehydration (loss of
five to nine per cent of body weight). Children were not included if they had dysentery,
fever on admission (temperature over 39° C) and/or the presence of another severe
infection (such as pneumonia or measles). During the first six hours (the 'rehydration
phase') children were given 100ml/kg of either sorghum based ORS or WHO/UNICEF ORS.
Breastfeeding was continued during the rehydration phase and food (milk and bananas) was
re-introduced as soon as rehydration was achieved. On admission, there was no difference between the children given sorghum ORS and those
given glucose ORS. However, the sorghum based ORS group showed a significant reduction in
the duration of diarrhoea, in the total ORS intake and in the total output of stools. This
study was a hospital based clinical trial, and it remains to be seen whether an ORT fluid
based on sorghum can be used successfully in
the community. Lepage, P, et al., 1989. Food based oral rehydration salt solution for acute
childhood diarrhoea. Sweet potato water: Papua New Guinea
In Papua New Guinea, there are limited choices for the selection of suitable home
fluids because no cereal grains are grown locally. In the coastal and lowland areas
coconut water is widely available and health workers recommend it for preventing
dehydration. However, in the highlands no suitable fluids are available. This problem led
to a pilot study of the efficacy and safety of a solution made from kaukau (sweet potato)
- the staple crop in many parts of the country, widely grown in the highlands. After
trying various recipes, a fluid was produced by boiling two pieces of kaukau in 1.5 litres
of water for 35 minutes. The potato was then mashed and water added to make one litre of
drinkable solution. Three grams of salt were also added. The sweet potato solution was then compared with the standard WHO formula ORS in a
small study. Thirteen children with mild to moderate dehydration caused by acute diarrhoea
were treated with WHO/UNICEF ORS and ten were treated with kaukau-salt solution. The ages
in both groups ranged from four to 23 months and there were approximately the same number
of cases of mild and moderate dehydration in each group. The average time for rehydration
was the approximately the same for both groups. There were no side effects in the kaukau
group and all infants seemed to like the taste of the solution. Mothers and nursing staff were enthusiastic about its use. Although this pilot project involved very small numbers of patients, the results were
encouraging and suggest that sweet potato solution could be both safe and effective for
ORT, and culturally acceptable. Further studies are planned for 1990 to confirm the safety
of solutions prepared at home by mothers. Howard, P, et al., 1989. Proposed use of sweet potato water as a fluid for oral
rehydration therapy for diarrhoea. Papua New Guinea Institute of Medical Research,
Goroka,
Papua New Guinea. Wheat ORS in refugee camps
Mothers in Afghan refugee camps in Pakistan have been taught to use packet oral
rehydration salts, and to mix a home sugar-salt solution (SSS) for children with
diarrhoea. However, most mothers mix SSS incorrectly, leading to the risk of an
ineffective or harmful solution. Because research shows positive results with cereal based
ORS, it has been suggested that home made wheat and/or rice solutions would be better home
solutions. Research was undertaken to find out if mothers would use wheat based solutions - wheat
is cheap and widely available. Women (mostly non-literate) were taught the wheat solution
recipe: two fistfuls of wheat flour and a two to three finger pinch of salt per litre of
water. Teaching was carried out in homes and basic health centres by trained female health
workers. Follow up visits were carried out between two weeks and two months later to find
out: if mothers could still make the recipe correctly; if they had used it when their
children had diarrhoea; and what they thought of it. Of the 64 women interviewed, 60 per
cent said they gave one of the rehydration solutions on the first day of diarrhoea (other
fluids given on the first day included a yoghurt drink, green tea, traditional herbal
drinks and rice water). There were no cultural beliefs to prevent the use of a wheat based solution for
diarrhoea. Depending on the location and the method of teaching used, between 40 and 94
per cent of the women could demonstrate making the wheat based solution correctly. They
liked the wheat solution, as the taste is familiar and wheat flour is used every day to
make bread. Mothers also found the recipe easy to make. When discussing which solution the women preferred, and why, most mothers said all the
solutions were good. When asked which was easier, a significant number said that the
wheat, salt and water solution was a little easier than both rice water and
SSS, because
rice needed to be cleaned and washed and cooked longer, and SSS needed correct
measurement. While many thought rice water tasted best, they suggested that it was not
practical because of its expense (rice is considered to be a luxury and is not kept in
most Afghan homes). The Afghan women in this study learned the new recipe quickly and had
good recall when followed up. They knew why and when to give ORT, and continued to give
other foods in addition to the wheat solution, showing that they did not confuse the
wheat-salt solution and food. For Afghan families, sugar is expensive, ORS packets
unavailable, and it may not be possible to mix SSS correctly. Therefore, it is worthwhile
to continue to study wheat based, or both wheat and rice based solutions as alternatives
or additions to the sugar-salt solution being taught now. Siener, K, 1989. Wheat based ORS for Afghans, International Rescue Committee,
Peshawar, Pakistan. Bangladesh: field trials of rice based ORS Studies were carried out on rice based oral rehydration therapy from 1982 to 1987.
Packets of rice based ORS were given to one group of mothers; glucose ORS packets to
another; and no packets to a third group of mothers who had access to local treatment
facilities. All the mothers of children aged under four years in the first two groups were
taught to prepare and use ORS. Use of ORT was highest in the rice ORS group, and lowest in
the control group (where drugs were also most often used).
 |
Cereal based oral rehydration solution may reduce the duration
of diarrhoea.
Duration of diarrhoeal illness was shortest in the group given rice ORS, in which more
than 60 per cent of children with non-dysenteric diarrhoea recovered within three days,
and less than one per cent suffered beyond 14 days.
|
Of the children given glucose ORS, 30 per cent recovered within three days, and about
three per cent still had diarrhoea after 14 days. In the third group, only six per cent
had recovered in three days, and 12 per cent had diarrhoea after 14 days. Bari, A, et al., 1989. Community study of rice based ORS in rural Bangladesh,
International Centre for Diarrhoeal Diseases Research, Bangladesh. More information about these and other studies is available from DD.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 41 June 1990
 4 Page 5 6 4 Page 5 6
Glossary Dehydration: the loss of water and salts caused by diarrhoea. Serious
dehydration can cause death.
Oral rehydration therapy (ORT): the administration of fluid by mouth to prevent
or correct dehydration.
Oral rehydration salts (ORS): the standard WHO/ UNICEF formula of glucose and
salts for ORT. Also known as 'glucose ORS'. Dissolving the salts in water makes ORS
solution.
Cereal based ORS: the standard WHO/UNICEF recommended formula but with 50 grams
of cereal instead of 20 grams of glucose (to be added to one litre of water). The cereal
contains starch which is broken down into glucose during digestion.
Cereal based ORT: the giving by mouth of a rehydrating fluid which is a thick
but drinkable mixture of a starchy food (approximately 50 to 80 grams per litre of water)
preferably with salt added (about three grams per litre of fluid).
Sugar salt solution (SSS): a solution containing only sugar, salt and water in
precise quantities (18 grams of sugar, three grams of salt and one litre of water).
|
International meeting
A symposium held in Karachi, Pakistan in November 1989 brought together many experts to
discuss the latest findings from studies of cereal based solutions for oral rehydration
therapy. Participants examined the scientific evidence supporting the claim that cereal
based ORS solutions can reduce stool volume and duration of diarrhoea. Clinical trials
reported showed that a range of cereals and starchy foods are as effective as glucose in
ORS for preventing and treating dehydration. Cereal ORS has been found to be especially
successful in cases of cholera. Further research was recommended in patients with
non-cholera diarrhoea, and in young children under four months of age or with
malnutrition. Cereal based ORS may prove a useful alternative to standard ORS, but more
research is needed to define its relative usefulness for young children with acute
diarrhoea. And it is important to find out if cereal ORS is better than standard ORS given
with cooked cereal food. Programme issues
The potential advantages and difficulties of introducing cereal based ORS into
diarrhoeal disease control programmes were also discussed. Where programmes have
established widespread distribution of ORS packets, or have a policy of promoting
sugar-salt solutions, it may not be advisable to introduce cereal ORS as an option,
because this may cause confusion or undermine existing health education. Where this is not
the case, and communities do not have access to standard ORS (in packets or otherwise)
cereal ORS could be an acceptable and effective option. Home use issues
Specific considerations discussed relating to promotion of cereal-salt solutions for
home use included:
- which cereals are most available and acceptable, as well as effective
- requirements for home preparation of cereal based solutions, including mothers' time and
fuel availability
- teaching and training required to ensure that cereal-salt solutions are safe and given
in timely and adequate amounts
- ensuring that the potential problem of confusion between cereal based ORT and food is
avoided.
Copies of the meeting proceedings are available. Details from Aga Khan Foundation, P
O Box 435, 1211 Geneva 6, Switzerland; and ICHF,
American City Building, Suite 325, 10277 Wincopin Circle, Columbia MD 21044, USA.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 41 June 1990
 5 Page 6 7 5 Page 6 7
How to feed a baby who cannot breastfeed
Cup feeding is much safer than bottle feeding and can be more practical than using
a spoon. Breastmilk is always the best food for babies, who need nothing else until they are
four to six months old. But, babies who are very small or ill may be too weak to suck at
the breast, and so must be fed - with breastmilk if possible - in another way. Why is cup feeding necessary?
Breastfeeding is the ideal way to feed a baby because breastmilk is the best possible
food and drink, and it gives the baby protection against diseases. With breastfeeding,
food for the baby is always ready and free from germs; and both mother and baby benefit
from close contact. However, another way of feeding is necessary when breastfeeding is not possible, and
feeding with a cup or spoon is the best and safest alternative. Breastfeeding may not be possible if:
- a baby is too weak to suck, for example during and after illness, or if it is born early
and very small
- the mother is very ill, or the baby has no mother or other woman to breastfeed it
- the mother cannot stay with her baby all day and a relative or friend has to feed the
baby.
Can you give breastmilk from a cup? Yes, definitely. If breastfeeding is not possible, the second best option is for the
mother to express breastmilk into a cup.
|
Express breastmilk into a cup for a baby who cannot breastfeed. The baby can then still have the benefits of breastmilk, even if it cannot breastfeed.
Other milks should be given only if no breastmilk is available from the mother, another
woman or a breastmilk bank.
|
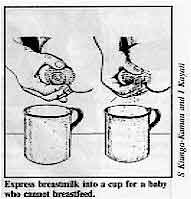 |
When can you start cup feeding? Whenever it is necessary - even straight after birth. Any baby who can swallow can
drink from a cup. How do you feed a baby with a cup?
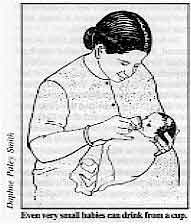 |
Even very small babies can drink from a cup Just hold the baby comfortably in your arms, and hold the cup to his or her lips. Be
careful not to tip the cup too far or too fast for the baby to swallow all of the milk
coming out of it. Give a little at a time, with short rests in between, especially if the
baby is sick or weak. Ordinary open cups should be used, not those with covers or spouts
which are too difficult to clean, and need to be sterilised like bottles.
|
What about bottle-feeding?
Bottle-feeding is dangerous because it is very difficult to keep bottles and teats
clean and free from germs without careful and regular sterilisation. Feeding bottles are a
major cause of infant diarrhoea. Because the bottles must be boiled before each feed,
bottle-feeding costs a lot in fuel, water and time. Bottle-feeding also stops babies
wanting to suck at the breast and makes them suck in a way which can cause sore nipples.
Bottle-feeding should always be avoided. What about spoon feeding? Spoon feeding is much safer than bottle feeding because spoons and bowls or cup are
much easier to clean. But it can take a very long time to give a baby enough food or fluid
using a spoon. Both the mother (or other caretaker) and baby are likely to get tired or
distracted before the baby has had enough food. However, if the baby can take only very
small amounts of milk, for example when there are breathing difficulties, or you think the
baby may choke or vomit, then it may be better to use a spoon than a cup. Acknowledgement: the information on this page is taken from the IBFAN
(International Baby Food Action Network) Statement on Cups. Copies available from
IBFAN-Africa, P O Box 34308, Nairobi, Kenya. More information
Feeding low birth weight babies IBFAN, 1986, VHS, 29 minutes. A training video
tape for health workers. This video demonstrates cup feeding of babies as small as 1.7kg.
Copies are available from: UNICEF, Communication and Information Services, P O Box 44145
Nairobi, Kenya; or contact the UNICEF office in your country. Breastfeeding - Dialogue on Diarrhoea Health
Basics series, originally published as an insert in DD issue 37, June 1989.
Six pages of information on breastfeeding including sources of further information and
publications. Copies available free of charge from AHRTAG.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 41 June 1990
 6 Page 7 8 6 Page 7 8
Cups are better than bottles because... CUPS have a simple shape and can be easily cleaned with soap and water.
Open CUPS do not encourage storage of feeds or carrying them about for several hours.
CUPS do not make babies unable or unwilling to suck at the breast.
CUPS used in hospital and by health workers teach the community a method which is safe
to use at home.
Using CUPS means that the small infant has some contact with the mother or another
person during feeds.
BOTTLES and teats have many awkward corners which cannot be cleaned except by boiling.
BOTTLES encourage the unsafe storage of feeds, increasing the chances for germs to
breed.
BOTTLES teach babies to suck in a way which makes them less willing to breastfeed.
BOTTLES used in hospital provide an example which cannot be safely or cheaply followed
by mothers at home.
BOTTLES can be propped up, depriving the baby of human contact. |
 |
Diarrhoea and potassium |
 |
Q What is the relationship between diarrhoea and potassium?
A
During diarrhoea, fluids and salts, including potassium chloride, are lost from the body.
If potassium (K+) lost is not replaced, low levels in the blood result (this is
hypokalaemia). However, most of the potassium in the body is stored in the cells, and so
measuring the level of potassium in the blood does not always give a true indication of
the status of body potassium. Children with protracted diarrhoea and malnutrition are
especially likely to be potassium-depleted. It may be wise to consider any child who is
undernourished and who has had diarrhoea for more than a few days likely to be
hypokalaemic, and to take appropriate action.
Q What are the signs of
hypokalaemia?
A
Hypokalaemia can lead to vomiting, anorexia or obstruction of the bowel. The signs of
severe K+ loss are weak and relaxed muscles, abdominal distension, and slowing of the
heart rate.
Q Does oral rehydration therapy replace lost potassium?
A
Children with diarrhoea need potassium during rehydration to prevent or replace any K +
loss. Packets of ORS formula contain enough potassium chloride (1.5 grams per packet for a
litre of water) to replace losses during diarrhoea. Proper use of ORS usually ensures that
any hypokalaemia is corrected within 24 to 36 hours of starting oral rehydration therapy.
Where packets of WHO/UNICEF ORS are unavailable, home made sugar-salt solutions
(SSS) and
home available fluids are usually used to prevent and (if necessary) treat dehydration.
SSS does not contain potassium, and other home available solutions also may not. It is
therefore important to give children adequate amounts of locally available
potassium-containing foods to replace losses, and to help restore appetite and food
intake.
Q What are good sources of potassium?
A
Fruits and vegetables are good sources. Those with the most potassium (in mmol per 100g)
include spinach (12.6) avocado (10.3), banana (9.0), pumpkin (8.0) and coconut water
(8.0). Plantain, papaya, oranges, grapefruit, tomato juice, carrot, pineapple, soya and
peanuts are also good sources. Thirty grams of banana supplies approximately 115mg of K +
; the same amount of K+ would also be supplied by 6g of defatted soy flour, or 20g of
lentils, peanuts or potatoes, and 30g of whole wheat flour or dark green leafy vegetables
(DGLV). Soy flour should be toasted, and DGLV should be steamed (since K+ is soluble in
water). In general, leaves may contain more potassium than fruits, although it will depend on
the type of soil in which the plant is grown. Where soil is very deficient in K + , plants
do not grow well, but probably maintain a minimal concentration of potassium. For small children who cannot eat large quantities of starchy foods like bananas,
drinking water which has been dripped through about 5g of wood ash may be a more effective
way of increasing potassium intake. The ash should be fresh (but cooled) and therefore
free of germs. The ash from some fresh water weeds, such as the water hyacinth, is an even
richer source of K+.
Q When should potassium rich foods be given?
A
Foods rich in K + should be given during diarrhoea and for at least a week afterwards to
ensure that potassium levels are returned to normal. References Dialogue on Diarrhoea issues 3 (Potassium losses and replacement in
diarrhoea) and 5 (Pirie, N W).
Moy, R J D, and Booth, I W, 1988. Acute diarrhoea: who needs potassium? (Editorial). J.
Trop. Paed. 34: 2-3.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 41 June 1990
 7 Page 8 7 Page 8
Traditional recipe Thank you for DD39 on traditional beliefs and
treatments for diarrhoea. The Burundian traditional method is to give the patient some
honey and salt in a glass of water. I know this from experience - when I was a small
child, my mother gave me this mixture, and it always seemed to help. Simeon Bandy A Yera, P 0 Box 97, Gitega, Burundi.
Does ORS treat diarrhoea? Diarrhoea is recognised as one of the main killer diseases in children in developing
countries. Though the diarrhoea itself (more than three loose stools per day) is usually a
self-limiting problem, the death of many children can be caused by both the short and long
term effects of diarrhoea, including dehydration and malnutrition. Many efforts in Third
World countries are therefore directed at the fight against these results of diarrhoea,
not against the diarrhoea itself. In this, ORS plays an important role. In our approach to the parents of sick children we should be very explicit. What
parents worry about most is the diarrhoea, not dehydration or malnutrition. Though in our
approach we say that we treat the diarrhoea, in fact it doesn't always stop it. Some of
the methods used by parents to stop the diarrhoea can seem much more efficacious than
ours. For example, if they restrict feeding or buy 'anti-diarrhoeal' drugs in the market,
they see that the frequency of stools seems to diminish, but when they give oral
rehydration fluids and continue feeding, the number of loose stools does not always
diminish. This does not help to build trust in 'a new way to treat diarrhoea'. This problem has been raised in discussions with health workers in Cambodia who
remarked: 'We tried it, but the diarrhoea did not stop! ' We have realised that the
parents do not care so much, or understand, about dehydration. Dr Chhour Y Meng and Dr G van Bruggen, Phnom Penh National Paediatric Hospital,
Cambodia.
Dr N Pierce of WHO replies: Drs Meng and van Bruggen are correct that ORS does not stop diarrhoea immediately, but
neither do 'anti-diarrhoeal' drugs (they only restrict bowel movements). It is better to
tell parents that ORS is medicine to make their child feel better, and stronger. ORS will
make the diarrhoea stop, but after a few days.
Local beliefs Following the 'Viewpoints' on local beliefs about diarrhoea (DD
39) I would like to add some information from Kerala. Fewer
children here are dying of dehydration, because there is good access to medical services.
But, many people do not know how diarrhoea is caused, often believing that teething is
responsible. Mothers often give very diluted feeds of cows milk or infant formula to sick children,
fearing that less watery food will cause indigestion. This means that many children are
underfed and sometimes malnourished. Fewer mothers from richer families are breastfeeding
their babies. Most people do not understand that diarrhoea is caused by germs in food or
water, and that breastfeeding provides the best and cleanest possible food. Often, mothers
go from one doctor to another looking for an instant cure for their child's diarrhoea, not
realising that they are putting the child in danger by not giving it enough food. People do not understand that fluids are needed during diarrhoea - they believe that
giving a child more to drink will only increase the diarrhoea. Many mothers here know
about ORS, but instead of using it at home, they will want to see a doctor whatever their
financial or educational status. In Kerala, a two child family is accepted by most
parents, and they want to do everything possible to make sure that the children are
healthy. In our practice, we have found that home fluids such as home made rehydration
solutions, coconut water, and arrowroot gruel are more acceptable to children than
commercial ORS . Dr K Jacob Roy, Tropical Health Foundation of India, Guravayar Road, Kunnamkulam
680503, Kerala, India.
ORS for diabetics? I have a problem for which an explanation from your organisation will be of great help
to me and my colleagues. The problem is about management of moderate and severe
dehydration using ORS in diabetics (insulin dependent and non-insulin dependent alike),
since sugar forms a major part of the formula. Joshua N Wilson, Nguru Clinics and Maternity, P O Box 104,
Nguru, Borno State,
Nigeria.
Dr Peter Milla, Senior Lecturer, Institute of Child Health, London, replies: The problem is probably best considered in two parts: insulin dependent diabetes and
non-insulin dependent diabetes. As far as insulin dependent diabetes is concerned, the difficulty is no greater than
that posed for any severe infection in a diabetic dependent upon insulin, when control of
the diabetes may be disturbed. The carbohydrate load imposed by oral rehydration solution
is not likely to be greater than that contained in the diabetic's normal diet. Clearly,
however, the electrolyte disturbance may make control of the diabetes more difficult and
it should be managed in the same way as any other severe infective process. I think that
if one remembers that the carbohydrate intake of a patient with diabetes is likely to be
within the region of 100 to 200g of carbohydrate depending on the severity of the process
and the presence or absence of peripheral insulin resistance, then this allows between
four and ten litres of oral rehydration solution to be used each day if the patient is
taking no diet by mouth. With regard to non-insulin dependent diabetics, then the limiting factors are the
disturbance caused by the diarrhoeal infection and the carbohydrate restrictions imposed
by dietary management. For those on a 100g carbohydrate diet, then this is the equivalent
in carbohydrate terms to four litres of OR solution per day. I think in ordinary clinical
practice it is unlikely that this will pose a major problem.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Assistant editor Nina Behrman Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 41 June 1990
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 24 April, 2014
updated: 24 April, 2014
|