|
| |
Issue no. 18 - August 1984
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
updated: 23 April, 2014
Pages 1-8 Diarrhoea Dialogue Online Issue 18 -
August 1984
|
DDOnline
Diarrhoea Dialogue Online Issue 18 August
1984  Page 1 2
Page 1 2
Making progress
Diarrhoea remains a major cause of ill health and death in developing countries -
especially among children. Much of this suffering is preventable and substantial progress
has been made since the World Health Organization set up its Control of Diarrhoeal
Diseases Programme in 1978 (see pages four and five). ORT: greater commitment required
The life-saving value of ORT is increasingly accepted around the world. However,
packets of oral rehydration salts (ORS) and simple instructions for their use are still
not reaching many communities where diarrhoea is worst. Also, some medical leaders are not
yet committed to ORT (see page="#page8">eight, letter from Trinidad). Support
from all health care professionals is crucial if ORT is to have the impact it deserves on
child mortality. Water and sanitation
 |
Encouraging handwashing early
Oral rehydration prevents death from dehydration due to diarrhoea. It cannot stop the
transmission of diarrhoeal infections. Protective vaccines are being developed but will
take time to perfect. There are also constraints to overcome in their delivery (see Diarrhoea
Dialogue issues 14 and 16). Improvements
in water supplies and sanitation come slowly and can be costly. Progress in a UNICEF-
supported water programme in Nigeria is described on page="#page3">three and
shows how community involvement from the start is essential for success. News from the
Solomon Islands (see page="#page2">two) confirms this conclusion. Latrine
developments in Zimbabwe emphasize the value of a realistic approach to sanitation systems
(see page="#page7">seven).
|
Other interventions
Other important ways exist to diminish the spread and the harmful effects of diarrhoea
- immunization against measles, promotion of breastfeeding and the encouragement of
handwashing and personal hygiene (see Diarrhoea Dialogue issues="dd16.htm">16
and 17 and page="#page2">two in this issue). All
require well designed educational programmes which are appropriate to local circumstances
and resources. The="#page6">practical advice page in this issue tells how
people can make their own soap from simple ingredients. Importance of evaluation
Evaluation of all interventions is essential. The="dd20.htm">first issue of Diarrhoea
Dialogue in 1985 will concentrate on 'operational research. ' Simple observations
and experiments can be undertaken by health workers and their communities (see page="#page2">two) to find out when, where, why and how much progress is being made -
and how progress may be speeded up! KME and WAMC
|
In this issue . . .
- A review of the WHO Diarrhoeal Disease Control Programme
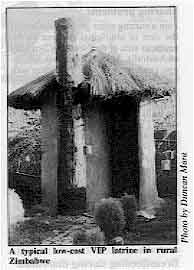
- Duncan Mara looks at low-cost latrines - the latest developments
- Practical advice - how to make soap
|
|
DDOnline
Diarrhoea Dialogue Online Issue 18 August
1984  1 Page 2 3 1 Page 2 3
Solomon Islands' success The Solomon Islands look set to mark the end of the International Drinking Water Supply
and Sanitation Decade in 1990, by becoming one of the first developing countries to
provide access to safe drinking water for its entire population, estimated at 250,000. Two
main factors have contributed to this imminent success. Firstly, community participation
(communities have been involved in all stages of the development process and have also
been trained to maintain and repair their own water systems). Secondly, technologies that
are both appropriate and affordable, such as bamboo-reinforced water tanks, have been used
and the water supply systems have been introduced on a small scale, to match local needs. Health and Development, April 1984.
Water and sanitation: health impact?
A meeting was held at Cox's Bazaar, Bangladesh, in November 1983 to discuss the best
way of assessing the achievements of water and sanitation programmes. Such programmes are
implemented in the widely held belief that automatic improvements in health will result,
but this is not always the case. High expectations often come from the policymakers,
donors or governments investing in the programme, who want to see concrete results. On a
large scale, such programmes are extremely expensive. Another important factor is the
time-lapse which occurs before any improvements can be seen. Benefits such as reduction in
disease and improvements in nutritional status often only appear gradually. With these
factors in mind the Teknaf discussions centred on the following subjects:
- why/when/how often should health impact studies be undertaken?
- should the impact of water and sanitation on health be assessed independently of other
measurements of primary health care?
- can the project design and results be improved by taking preliminary surveys, and can
the results be applicable in other areas?
- what indices should be used to measure improvements, for example, the incidence of
diarrhoea, worms, eye and skin diseases or nutritional status, all of which may be
influenced by other factors?
- within what timescale should the study be carried out?
- what are the best ways of interpreting the findings and of communicating and
implementing the recommendations and conclusions drawn from these findings?
Findings
- It was suggested that using nutritional status as an indicator of improvements in health
would be more useful than using the incidence of diarrhoea. Participants gave evidence to
show that improved water supply does not necessarily reduce the incidence of diarrhoea.
Instead, it affects the type of pathogens causing the diarrhoea, and hence the type of
diarrhoea. Diarrhoeal incidence and duration are very hard to measure accurately,
depending largely on memory, whereas nutritional status is easier to measure and also
reflects diarrhoeal incidence and duration.
- Less direct but important health benefits may result from water improvements, if mothers
no longer have to spend several hours each day fetching water. Nutrition could improve if
mothers had more time and energy for growing crops, cooking, and looking after their
children, including breastfeeding.
- The participants concluded that the best time to evaluate a programme is from one to
three years after the project has started. This gives enough time for the work to have an
impact, but is soon enough to minimize the effects of other factors which can influence
the results.
- Another important finding discussed was that improvements in health seem to be directly
related to the amount of water used - for example, in St Lucia, this was the single
most important factor, and the amount of water used was inversely related to the numbers
of childhood illnesses.
Based on material presented in 'Glimpse' Vol 6 No. 2 March/April 1984.
Handwashing helps
Diarrhoea is usually caused by faecal-oral transmission of germs. It is difficult to
avoid this in dirty and contaminated situations. Simple personal hygiene, especially
hand-washing after using the toilet and before preparing or eating food, can reduce the
rate of diarrhoea attacks. This has been shown independently in several studies from as
far apart as Guatemala, Bangladesh and the USA where attack rates were reduced by between
14 and 48 per cent (Feachem 1984). At least two steps are required to achieve such an improvement: education about the
hygiene measures required to reduce transmission, and a change in the pattern of
behaviour. Economic constraints and cultural barriers prevent this in many communities.
There is also a need to identify the most important protective actions and the most
appropriate messages in any group. However, these limitations should not stop everyone
practising and preaching the value of handwashing in preventing diarrhoea. Feachem R G, 1984 Bull. WHO 62.1. WHO water checklist A recent WHO publication, Rural water supply: operation and maintenance - eight
questions to ask, is intended to be a guide for planners and engineers involved in
rural water supply projects. The eight questions consider such factors as site conditions;
socio-economic conditions; project planning and development; the influence of resource
availability outside the community; system management; manpower development and training
and on-site resource availability. The publication (reference ETS/83.9) is available in
English and French (shortly to be available in Spanish) from WHO, 1211 Geneva 27,
Switzerland. In the next issue . . . .
We will concentrate on oral rehydration therapy (ORT). Although ORT has already saved
thousands of lives, it is still not reaching all those who need it - DD19
looks at how ORT is being promoted and at research into an improved ORS formula.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 18 August
1984  2 Page 3 4 2 Page 3 4
| Water programme in Nigeria |
Promoting health
A successful UNICEF-assisted project in Imo State began health and hygiene
education long before water supplies were actually installed. The UN Water Decade aims to provide 'Clean Water for All by the Year 1990'. Through
this it hopes to reduce illness caused by inadequate water and sanitation facilities.
Evaluations have shown that better health does not automatically result from improvements
in water supplies and sanitation. One project which may provide data about the impact of
such changes on health is a UNICEF-assisted programme in Imo State, Nigeria, begun in late
1981. The most important aspect of this particular programme is the emphasis on health and
hygiene education, to try to change water use and excreta disposal practices so that the
people gain the maximum health benefit from the project. Many previous projects have not
led to improvements in health because the educational component has been introduced as an
'afterthought' once the new facilities have been established. Sequence of events In each local government area, such as Ohaozara in North-eastern Imo State, the
programme is initiated in overlapping stages. First, the community mobilisation team meets
with government officials, community leaders and villagers to explore village needs,
explain the project and its aims and foster a spirit of local ownership in the project.
Next, each village chooses four village-based workers (VBWs) who undergo a four week
training programme under the direction of the training team. Meanwhile the sanitation team
has the task of assisting villagers in building ventilated improved pit latrines. All this
happens before drilling of boreholes for water is even begun - the community is persuaded
to alter existing habits and becomes aware of preventative health measures before the
arrival of new water supply. In five villages in Chaozara local government area, the
activities of an evaluation team have preceded all other activities by one year. The team
collects data at regular intervals to allow evaluation of the project's impact on the
health of young children. An important aim of this evaluation is to collect information on
diarrhoea incidence and aetiology. A simpler evaluative procedure to monitor the
functioning and use of facilities rather than health impact has been developed and is
being introduced into a sample of project villages. An important characteristic of the
five project teams - mobilization, evaluation, training, sanitation and drilling and pump
installation - is that they are seconded from six state government ministries and include
a variety of personnel ranging from sanitarians and health educators to social
statisticians. Overall coordination of the teams and the pace at which they work is
carefully handled so that the balance of village life is not unduly disturbed. Hygiene education and community involvement At village level the VBWs have responsibility for the hygiene education component of
the project - for example, promoting proper water use habits and excreta disposal
practices. The VBWs, usually two men and two women, are selected by their fellow villagers
and must fulfill certain criteria. They must be established members of the community,
married (preferably with children) and able to read and write to a minimum standard. A
steering committee is formed in each village, consisting of respected members of the
community. This committee supports VBWs and organizes VBW payment. Convincing fellow
villagers to change their hygiene habits is not always easy. Strong support from the
steering committee is necessary to give the VBWs authority in the eyes of the villagers.
Enthusiastic community involvement is also necessary to raise funds and organize the
building of latrines. Programme results
 |
Arrival
of new water supply
Photo by Deborah Blum The success of the programme depends to a great extent on the continued commitment of
the state and local governments, individual communities and on the educational activities
of the VBWs. Although it will be some time before the results of the health impact
evaluation are known, important accomplishments are already evident. The Imo State project
is now serving 370,000 people or some 8-9 per cent of rural Imo State at a low per capita
cost. The Imo State government is committed to extend the project throughout the state and
the federal government has agreed to introduce the project model in at least five other
states.
|
The project is already underway in two of these states with encouraging results. In
Gongola state in particular, community mobilisation has led to striking transformations in
project villages and fostered a spirit of community self-improvement. For example,
environmental sanitation campaigns and tree and flower planting activities have
accompanied the project activities. Finally, in participatory states and local government areas the project has established
an infrastructure to undertake other primary health activities. It is no surprise that
project areas have been particularly chosen as starting points for the national Expanded
Programme on Immunization (EPI), nor that the Imo Project has been recommended by the
Nigerian Council on Health as an example of primary health care to be visited by
delegations from all other states. Deborah Blum, London School of Hygiene and Tropical Medicine, Keppel Street, London
WC1E 7HT. Information also taken from Issue 116, UNICEF News.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 18 August
1984  3 Page 4 5 3 Page 4 5
| Five years on: review of the WHO/CDD programme |
Strengthening national initiatives
Reducing childhood illness and death due to diarrhoea is a major priority for WHO.
We report on its achievements in this area since 1978. The WHO Programme for the Control of Diarrhoeal Diseases (CDD) was set up with the
formidable task of assisting WHO member countries to reduce the high levels of illness and
death - especially in children under five - due to diarrhoeal diseases. The CDD Programme
has a health services component and a research component. Information about Programme
activities is circulated through a mailing list of 5,000 and through publications such as Diarrhoea
Dialogue. CDD works closely with a number of other agencies, including UNICEF and the
League of Red Cross and Red Crescent Societies, in the promotion of oral rehydration
therapy (ORT) around the world. UNICEF and WHO recently published a
joint statement on the
management of diarrhoea and use of ORT(1). Health services component
By the end of 1983, seventy two countries had received assistance from CDD in planning
national diarrhoeal disease control programmes. Of these, 52 countries are now
implementing plans. Emphasis is put on sound programme planning; the training of health
workers at all levels; local production and development of oral rehydration salts (ORS);
and evaluation of programme activities. The major strategy of all the national diarrhoeal
disease control programmes is proper case management of acute diarrhoea with oral
rehydration therapy, emphasizing both the treatment of dehydration by use of ORS
throughout the health system and prevention of dehydration through treatment and
use of appropriate home-made solutions. Training:
The training of national CDD programme managers and others involved in diarrhoeal
disease control work continues to be a priority. In 1983, five training courses for
programme managers took place, attended by 170 people from 50 countries. Since this
particular course began, 677 people from 117 countries have been trained. In 1983, a new
course was launched in nine countries, aimed at first line supervisors in the health
system. The course deals not only with diarrhoeal disease control but also looks at other
primary health care interventions. So far, 410 people have attended the courses, coming
from 14 countries, and, in Thailand and Indonesia, the course material has been translated
for national use. The same material is being used by UNICEF training workshops; also in combined courses
between CDD and the WHO Expanded Programme on Immunization (EPI) to strengthen curricula
of nursing schools, the first being held in Egypt. Recognizing the importance of training
peripheral health workers in the use of ORT, CDD recommends that such training courses
should use nationally prepared materials based on the treatment and training sections of
the supervisory skills course. Technical training activities also continue in clinical
management; laboratory diagnosis; epidemiology and environmental health. Priority is given
to the clinical management courses for physicians and other senior level workers. As part
of the effort 37 regional and national CDD training units have been established. ORS production:
An essential part of national programmes is the availability of sufficient ORS packets.
CDD continues to work closely with UNICEF on the production and distribution of packets.
Thirty-eight developing countries are now producing their own ORS.
|
ORS production in Indonesia
Photo by H. Faust, WHO In 1983, UNICEF distributed 29 million packets to 78 countries, and other bilateral
agencies also provided packets through their own aid programmes. Commercial, national and
multinational companies have been encouraged to increase their production of ORS.
Important studies have been carried out during 1983 on the substitution of sodium
citrate for sodium bicarbonate in the ORS formula. Laboratory and clinical studies
have shown that not only is the new formula more stable in tropical conditions but also
results in some 20 per cent less stool output. This is because there is increased
intestinal absorption of sodium with citrate as compared with bicarbonate. The citrate
formula is also cheaper to pack. (Issue 19 of Diarrhoea Dialogue
to be published in November 1984 will carry a full report on the citrate formula).
|
 |
Evaluation:
Increasing emphasis has been put on developing CDD programme capability to evaluate
access to and use of ORS in children under five; impact of ORT in hospitals; and morbidity
and mortality due to diarrhoea. Information on all these subjects is essential to improve
the planning and development of national diarrhoeal disease control programmes. Guidelines
have also been developed to assess the cost-effectiveness of ORT at country level and
these are being tested in Indonesia and Honduras. An evaluation procedure has been
developed with the Environmental Health Division of WHO to assess the operation and use of
water supply and sanitation facilities.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 18 August
1984  4 Page 5 6 4 Page 5 6
| Five years on: review of the WHO/CDD programme |
Research component Biomedical:
The biomedical research component of the CDD Programme has made important advances
during the past year on many fronts - from studies into more effective ORS to clinical
trials for typhoid and rotavirus vaccines. CDD is now supporting 147 biomedical research
projects - 46 per cent of which are in developing countries. Research areas include
diagnostic microbiology, including simplified tests which can be used at the periphery
(see Diarrhoea Dialogue issue 9); immunology and vaccine
development, particularly in relation to typhoid fever and rotavirus infections (see Diarrhoea
Dialogue issue 16); drug development and the management of
acute diarrhoea. In the latter category, as well as the research into the citrate ORS formula described
above, CDD has actively pursued the development of even more effective ORS formulations -
both home-based and in packets. Studies have shown that a rice-based solution can reduce
diarrhoea output by up to 50 per cent. Trials are now being carried out to see whether
similar food-based solutions can be made from dal or maize. Unfortunately, the first
indications are that at least some of these solutions seem to ferment rapidly, which may
restrict their usefulness. Alternative methods of enriching ORT solutions are being
explored. Work has continued in the evaluation of traditional drugs for diarrhoea in
countries such as Bangladesh, China and Madagascar. Studies are also underway to examine
the absorption of different foods during and after diarrhoea. Information on these
approaches should be available at the end of 1984. In the area of epidemiology and ecology, research has shown that Vibrio cholerae can
survive in the environment in different forms. This important observation may explain the
seasonal occurrence of cholera in endemic areas. Operational research:
 |
Convincing doctors: management of diarrhoea using ORT in Bangladesh
Eighty-four operational research projects have now been supported by the CDD Programme,
the majority of them looking into aetiology/epidemiology or case management of acute
diarrhoea, especially the delivery of ORT in local settings . Overall, research activities
have been strengthened by CDD assistance to various institutions in developing countries
for training purposes. One important development has been the collaboration with Mahidol
University and the Ministry of Health in Thailand in the preparation of a proposal for
setting up a Centre for the Trial of Vaccines against Infectious Diseases at Mahidol
University. Research priorities in the area of chronic diarrhoea have now been established
and it is hoped to begin supporting research in this key area next year. Other new
research projects will include activities related to the additional diarrhoeal disease
control interventions of breastfeeding; use of clean water and sanitation; handwashing;
and measles immunization.
|
More information on all the Programme activities described above is available from
the Director, Programme for the Control of Diarrhoeal Diseases, WHO, 1211 Geneva 27,
Switzerland. (1) The Management of Diarrhoea and Use of Oral Rehydration Therapy. Joint
WHO/UNICEF Statement, 1983 (available in five languages from WHO).
|
|
DDOnline
Diarrhoea Dialogue Online Issue 18 August
1984  5 Page 6 7 5 Page 6 7
How to make soap
This article shows how soap can be made cheaply and easily on a small scale, in
the home or village, using locally available ingredients.
Soap is a very great help to people in being able to keep themselves and their
surroundings clean, and is therefore important in preventing the spread of disease. In
some countries soap is unavailable or very expensive. The table below shows the
ingredients necessary to make soap.
Basic ingredients
For one bar of soap you will
need:
- 230 ml (1 cup) of oil or clean, hard fat.
- 115 ml (½ cup) of water.
- 23.5 gms (5 teaspoons) of caustic soda (sodium hydroxide) crystals or lye.
- Borax and a few drops of perfume are optional.
For 4 kg of soap you will need:
- 3 litres/2.75 kg (13 cups) of oil or clean, hard fat.
- 1.2 litres (5 cups) of water.
- 370 gms of caustic soda (sodium hydroxide) crystals or lye.
|
- Animal fats such as tallow, mutton fat, lard, chicken fat or vegetable oils such as
olive, coconut, palm and palm kernel, cottonseed, castor, maize, soybean, safflowers and
groundnut can be used. The best soap is made from a mixture of oil and fat. Even polluted
fat can be used as long as it is first melted then strained through a finely woven cloth.
Coconut oil makes a softer soap than the other oils (because it is low in stearic acid)
and can be greasy. It is however the only soap that will produce a lather in seawater - so
in some cases using some coconut oil is good.
- The best water to use for soapmaking is soft water. Rainwater is therefore good. Hard
water contains mineral salts which hinder the cleansing action and lathering of the soap.
To soften water, add 15 ml or 1 tablespoon of lye to 3.8 litres/ 1 gallon of hard water
and leave to stand for several days after stirring. The water poured off from the top,
leaving a sediment behind, is soft water.
- Only caustic soda can make hard soap. The alternative, if caustic soda is not available,
is potash or lye, leached from ashes. Caustic soda should be stored in sealed containers
to prevent absorption of moisture from the atmosphere.
- Borax, although not necessary, can be used to improve the appearance of the soap and
increase the amount of suds produced.
- Perfumes can act as a preservative, but, if used should be resistant to alkali. For 4 kg
of soap one of the following should be used: 4 teaspoons of oil of sassafras; 2 teaspoons
of oil of wintergreen, citronella or lavender; or 1 teaspoon of oil of cloves or lemon.
- Different proportions of ingredients produce different types of soap: for hard scrubbing
soap use tallow for the fat quota; for laundry soap use ½ lard/cooking fat with ½
tallow; for toilet soap use ½ tallow with ½ vegetable oil.
Equipment
To make soap you will need:
- Two large bowls or buckets made from iron, clay, enamel or plastic. Never use aluminium
- it is destroyed by lye/caustic soda.
- Measuring cups made from any of the same materials as above, again except for
aluminium.
- Wooden or enamel spoons, or smooth sticks for stirring.
- Watertight wooden, plastic, cardboard or waxed containers for a mould; gourds, coconut
shells or split bamboo halves can also be used.
- Cloth or waxed paper can be used to line the moulds so that the soap can be easily
removed.
|
Method
- Dissolve caustic soda in water to produce lye water.
- Pour oil into separate container (add borax at this point if desired).
- Pour the lye water slowly onto the oil, stirring continuously in one direction. If an
oil-fat combination is being used add the melted and cooled fat to the oil/lye solution.
- Add perfume/ colouring now if desired/ available.
- When the mixture has a thick consistency, put into lined moulds/cooling frames and leave
to set for two days.
- If fat only is being used, it should first be clarified by boiling it up with water and
allowing the mixture to cool down and set. The clean fat can then be easily separated and
melted again for soapmaking. Always allow the fat to cool down before adding to the lye
water, slowly stirring in one direction.
Once the soap is made
- Do not move the moulds.
- When ready, cut the bars into slabs/ smaller bars.
- Stack on trays and leave to dry thoroughly for 4-6 weeks.
- When dry, cover to prevent further loss of moisture.
- If the soap is not set after two days, or there is grease visible on top of the soap,
leave it to set a little longer.
How to recognise good soap
Good soap should be hard, white, clean-smelling, tasteless and should shave from the
bar in a curl. It should not be greasy or taste unpleasant. The main point to remember is
that the soap you make does not have to be perfect. As long as it is usable it is better
than no soap. If, however, problems occur, there may be several reasons. Spoiled soap only
happens when:
- the wrong materials are used.
- the oil or fat is too rancid or salty.
- the lye water used is too hot or cold.
- the mixture is stirred either too fast or not long enough.
To reclaim soap:
- cut into small pieces and add to five pints of water.
- melt over a low heat.
- boil the mixture until it becomes syrupy.
- pour into a mould and leave for two days before cutting up as before.
| WARNING caustic soda is very dangerous and can burn skin and eyes.
Protective gloves should be worn if possible when making soap. If burns occur they should
be washed immediately with cold water and then treated with vinegar or citrus juice. Never
add water to caustic soda-always add the soda to the water. |
For further reading, please write to AHRTAG
|
|
DDOnline
Diarrhoea Dialogue Online Issue 18 August
1984  6 Page 7 8 6 Page 7 8
On-site sanitation
Duncan Mara describes some recent developments in the
design of VIP latrines and pour-flush toilets On-site sanitation systems can provide major health benefits at a fraction of the cost
of sewerage. They do not depend on piped sewerage or regular emptying methods of
sanitation that will never reach the vast majority of people in developing countries. The
Technology Advisory Group (TAG) of the World Bank/UNDP has published information on the
designs of ventilated improved pit (VIP) latrines and pour-flush (PF) toilets, which have
been developed in Botswana, Brazil, India, Tanzania and Zimbabwe. Two general design
manuals will shortly be published. Issue 5 of Diarrhoea Dialogue
described twin-pit VIP latrines and PF toilets. This review highlights some of the
developments that have taken place since then. VIP latrines
|
A
typical low-cost VIP latrine in rural Zimbabwe The most significant developments in VIP latrine design have come from Zimbabwe.
Latrines for rural areas can cost as little as US $10, since local materials - freely
available in the bush - are used extensively. The rectangular pit (1.5m x 0.6m x 3m) of
the low cost rural VIP latrine has a rough timber cover-slab, over which a spiral,
doorless superstructure is built in mud and wattle. The roof is thatched and the vent pipe
is made from a mat of reeds rolled up and plastered with cement mortar. A PVC-coated
fibreglass fly-screen is fixed at the top of the vent pipe. The only materials the
householder has to buy are the flyscreen, a bag of cement (to render the outside of the
superstructure and the vent pipe) some nails and tie-wire. This latrine can last a family
of six for over twenty years, although it needs regular annual maintenance to repair any
damage occurring during the rainy season. This is not a great problem, however, since the
latrine is built in almost the same way as the houses, so the local people already have
the necessary maintenance skills.
|
 |
A slightly better, but more expensive design is available at US $46. The pit is
circular (1.2m in diameter) 3m deep and is covered by a reinforced concrete slab 1.5m in
diameter. The spiral super-structure and vent pipe are built with local burnt bricks,
which are readily and cheaply available in rural Zimbabwe. A thatched roof is often used
although ferro-cement ones are also common. Stainless steel flyscreens are now preferred
to fibreglass ones since they last longer. These brick VIP latrine designs are becoming
very popular in Zimbabwe, especially as timber for the low-cost version described above is
now in scarce supply. There is also more space in the brick latrines; this permits
'bucket' showers to be taken in greater comfort. Two beneficial effects of this are
improved personal hygiene and a lower rate of solids accumulation in the pit (the addition
of small volumes of water improves the bacterial breakdown of faecal material). In urban areas, single-pit VIP latrines can be used for population densities of up to
300 persons per hectare. At slightly higher densities it is possible to built alternating
twin-pit VIP latrines (of the type described in Diarrhoea Dialogue, issue 5) but, in major urban VIP latrine programmes, it is generally
better to use single-pit latrines which can be desludged at regular intervals (once every
2-5 years). In parts of Ghana and Brazil, in-house VIP latrines have been constructed -
the pit itself is partly outside the house, so that it can be desludged regularly. Pour-flush toilets The alternating twin-pit PF latrine design described in Diarrhoea Dialogue, issue 5, is still preferred wherever desludging is done by
hand, as in India for example. A single-pit design is more suitable if a vacuum tanker is
used to empty the pit, as in Brazil. The most interesting developments in PF toilet design
have been concerned with the squat-pan or pedestal seat unit. The Swedish company, Ifo
Sanitar AB, has developed an add-on unit for the Indian glass-fibre squat-pan which
converts it into a low-volume cistern-flush toilet. Only 1.5 litres of water are needed
per flush. The cistern can be any size (15-30 litres) as there is a special valve which
releases only 1.5 litres of water when the cistern is operated. This is especially useful
where municipal water supplies are intermittent and service is often only provided for 1-2
hours a day, as the cistern can hold enough water for 10-20 flushes. In Brazil, following
prototype development work by the Institute of Technological Research in São Paulo, three
major manufacturers are now producing low-volume flush toilets which can be initially
operated in the pour-hush mode, but which can be upgraded later to operate as low-volume
cistern-flush units. The Brazilian models are made in glazed ceramic-ware and, at US $5,
are becoming extremely popular in low-income urban slum communities. Duncan Mara, Department of Civil Engineering, University of Leeds, U. K. Technical
Advisor TAG (World Bank UNDP) Further information on TAG's activities in low-cost sanitation, and copies of the
various TAG Technical notes on VIP latrines and PF toilets can be obtained from Richard N
Middleton, Project Manager, UNDP INT/81/047, WUDOR, The World Bank, 1818 H St NW,
Washington DC 20433, USA.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 18 August
1984  7 Page 8 7 Page 8
Sharing problems I am a nursing sister greatly involved in the care of aboriginal children in the
southern area of the Northern Territory of Australia. My work involves follow-ups;
guidance to people unfamiliar with the aboriginal ways; rural clinic every two weeks;
overall general paediatric care; teaching aboriginal health workers skills to better their
people in health ways. I feel it would be of great value for them to read your magazine Diarrhoea
Dialogue to let them know that other places have problems too, not just them.
Also I feel nursing staff would find it of great value. Would it be possible to obtain
regular copies for myself and staff? Sister Carmel Hattch, Paediatrics Clinical Assistant, Alice Springs Hospital and
Rural Area, Northern Territory, Australia.
Breastfeeding during diarrhoea I would like to congratulate you for packing so much information in such a concise and
lucid manner in Diarrhoea Dialogue issue 17 on
breastfeeding. The issue covers different practical aspects of breastfeeding like the
establishment and maintenance of lactation, the advantages to mother and infant, storage
of breastmilk etc. The pull-out poster was very inspiring. I am sure everyone who happens
to come across it will be stimulated to design and utilize similar material in their own
place of work. I would like to stress the importance of continuing breastfeeding during diarrhoea. For
one thing it will minimize weight loss due to diarrhoea, but, even more important, it will
reduce the number of mothers who switch to breastmilk substitutes after the infant has an
episode of diarrhoea. In South India an important reason for switching to breastmilk
substitutes and consequent lactation failure is the advice of misinformed health
professionals - doctors, nurses and health workers who advise withholding breastmilk for
2-3 days when the infant has diarrhoea. This often breaks the habit as well as the
mother's confidence in her own milk. More effort must be directed by all of us towards
protecting breastfeeding during diarrhoea. Dr Kingsley Jebakumar, Paediatrician, Church of South India Mission General
Hospital, Woriur, TiruchirapaIli-3, South India, 620003.
DD: health education My name is John A Chermack and I am a Peace Corps Volunteer from the United States
working in Honduras. I am a public health educator working in a town of 5,000 people. I
also will be working with surrounding pueblos of smaller sizes. I teach health, hygiene
and sanitation, nutrition and small vegetable gardening and a variety of health related
topics. David Werner in his book 'Helping health workers learn' suggests that your Diarrhoea
Dialogue newsletter is excellent. If it is possible I would appreciate being on your
mailing list and would also appreciate any other educational materials you might be able
to send. Any material in Spanish is of even greater value. John A Chermack, PVC, Marcala, La Paz, Honduras, Central America.
Editor's note: The Spanish edition of DD is available from PAHO, 525
Twenty-third Street, N.W., Washington D. C. 20037, USA.
Changing doctors' attitudes
The letters from Drs Puranik, Chandari and Nazmy in Diarrhoea Dialogue issue 16 as well as my experience in Trinidad and Tobago, Grenada, St
Vincent, St Kitts-Nevis and Venezuela have prompted this letter. I think all health
workers involved in managing children with diarrhoeal diseases would agree with me that
the major problem today, with the treatment of diarrhoeal disease, is the attitude of most
of the general practitioners. Invariably these doctors overprescribe antibiotics,
antidiarrhoeals, antimetics and antispasmedics for diarrhoea. Invariably an injection is
given. Invariably no information on rehydration or nutrition is given. We all know the
consequences, both to the children and to the doctors' lifestyles. Why has this not been
identified as the major problem? Are we scared of reasoning with our colleagues? Are they
not willing to talk over these things with us? What are the best ways to convince them,
not only of the benefits of ORT but of many other things, e. g. the misabuse of
antibiotics, that need to be corrected. Can we not identify the doctors in a country as
part of the problem of treating diarrhoea and give this the publicity it needs. Our
experience in Trinidad and Tobago suggests that this is a viable option when allied to the
more traditional means of reaching the medical practitioner e. g. seminars, letters from
the Hospital Consultant to the referring physician. Obviously however a great deal needs
to be done to answer these questions. David Bratt, Paediatrician, Port of Spain, General Hospital, Trinidad, W. I.
Editors' note: DD 16 reported on changing attitudes
among paediatricians in the U. K. towards ORT. Hopefully this may encourage a greater
acceptance of ORT amongst their colleagues in other countries.
Practical ideas Please send me six copies in addition to my own copy every month of Diarrhoea
Dialogue for distribution to my nurses and clinical officers in the Paediatric
diarrhoea ward of Kenyatta National Hospital. I find the publication very informative and
filled with practical suggestions and ideas on implementing oral rehydration therapy and
nutritional support in diarrhoeal illnesses. Your recent issue on breastfeeding was
excellent. Thank you. Dr Verna Jean Turkish, Lecturer in Paediatrics, Kenyatta National Hospital, P. O.
Box 30588, Nairobi, Kenya.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Executive editor Denise Ayres
Editorial assistant Kathy Attawell
Editorial advisory group
Professor David Candy (UK)
Dr I Dogramaci (Turkey)
Professor Richard Feachem (UK)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Professor Leonardo Mata (Costa Rica)
Dr Mujibur Rahaman (Bangladesh)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), UNICEF and WHO
|
Issue no. 18 August 1984
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
updated: 23 April, 2014
|