|
| |
Issue no. 22 - September 1985
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 22 -
September 1985
|
DDOnline
Dialogue on Diarrhoea Online Issue 22 September
1985  Page 1 2
Page 1 2
Newborns and diarrhoea
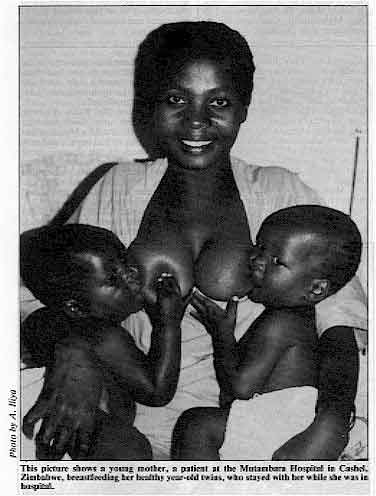 |
This picture shows a young mother, a patient at the Mutambara
Hospital in Cashel, Zimbabwe, breastfeeding her healthy year-old twins, who stayed with
her while she was in hospital. Severe diarrhoea can cause rapid death from dehydration in newborn infants if they are
given the wrong treatment. Our="#page4">centre pages describe the correct way
of giving oral rehydration therapy (ORT) for newborns with diarrhoea - in hospital, health
centre or home.
|
Doctors and nurses: a leading role
Enormous advances are being made in promoting the use of ORT at household and primary
health care levels. Unfortunately, places remain where this spread of knowledge still
fails to reduce the numbers of dehydrated children requiring hospital admission (see="#page7">page seven). Doctors and nurses everywhere should lead the way in
demonstrating the life-saving value of immediate ORT whenever diarrhoea occurs. With this
need in mind, this issue includes a 'clinical advice page' which covers management
problems related to oral rehydration therapy from a practical angle. There is also a
report of the way in which one hospital became more effective in treating children
admitted with diarrhoea. Breastmilk: natural protection The picture above, taken by Dr A. Iliya from Zimbabwe, wins our photographic
competition for the positive way in which it illustrates the benefits of breastfeeding -
essential for all infants and especially for newborns (see="su22.htm">insert
for other competition results). Breastmilk provides considerable natural protection
against diarrhoea. Both breastfeeding and the use of ORT need still wider promotion if the
lives and health of the world's children are to be properly safeguarded for the future. KME and WAMC
|
In this issue . . .
- Diarrhoea and the newborn
- Nurse training in Mozambique
- ORT - useful clinical advice
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 22 September
1985  1 Page 2 3 1 Page 2 3
Nutrition forum
The International Nutrition Planners Forum held a conference in the U. K. in August on
'Nutrition and Diarrhoeal Disease Control'. More than 30 invited participants, including
two of DD's Editorial Advisors, took part. USAID and WHO were also represented and
discussions centered on ways to integrate the control of diarrhoea and the improvement of
nutrition. Policy and planning, implementation issues and research needs were considered
by separate working groups. The final report from the conference will include, in addition
to the findings of the working groups, special papers presented at the plenary sessions by
Dr Leonardo Mata, Dr Majid Molla, Dr Jose Mora and Dr Dilip Mahalanabis. Chairmen for the
conference were Dr Shanti Ghosh and Dr Demissie Habte. The main theme for="dd23.htm">DD23, 'Feeding and diarrhoea', had already been selected and
we hope that the conference report will be available in time for it to be summarized in
that issue. The value of this newsletter as a means of conveying information to health
workers at all levels was recognized by the invitation to the Dialogue to be
represented at this important and extremely valuable meeting. ORT in practice
In many areas the message about oral rehydration therapy and its effectiveness is
still not reaching those who most need to know. This story, from a DD reader in
India, and others like it which we hope to publish as a regular series in future issues,
illustrates that the message can never be emphasized too often. We invite other readers to
tell us about their personal experience of "ORT in practice". Mrs Subhadra Masalkar is a Community Health Guide (CHG) in the village of Jategaon
which is part of the Vadu Rural Health Project under the K.E.M. Hospital, Pune, India. Mrs
Masalkar is 31 years old, married and educated to primary school level. After being
recruited to become a CHG, she received three weeks training and has since attended two
more short refresher courses. She also has continuing training every month in various
skills relevant to her job. The use of oral rehydration therapy (ORT) is one of the skills
she has been taught. This story illustrates her personal experience in the use of ORT in
treating a diarrhoea case and how it changed the attitude of the villagers. Jategaon has a population of 1,000 people and has no medical facilities. Primary health
care is provided by the CHG. Early one morning, Mr Maruti Rao, aged 50 years, was suddenly
taken ill with diarrhoea and vomiting. Mrs Masalkar was called to the house. She
immediately started to give ORT using packets of ready prepared oral rehydration salts
(ORS). The ORS was dissolved in clean water and Mr Rao was asked to sip the solution
continuously. However, the villagers had no faith in such simple treatment and decided to
take Mr Rao to the nearest village, Shikrapur, three kilometres away, where a doctor would
be available. They hired a cart and throughout the journey the patient was given ORS
solution by Mrs Masalkar. When they reached Shrikrapur, they found the doctor was not
there and so decided to take Mr Rao on to the nearest town, a further kilometre away. On
the way, Mr Rao began to feel much better and his weakness and exhaustion had almost
disappeared. He himself decided that he did not need any injections or other medicines
from the doctor and the villagers began the journey home with him. Meanwhile, the packets
of ORS had run out so Mrs Masalkar, who had stayed with the patient all the time, decided
to start him on the equivalent home remedy, using a mixture of common salt and cane sugar
and water in the correct proportions as she had been taught. She prepared it right away
and the patient was soon completely recovered and rehydrated. The news of Mr Rao's dramatic recovery using only ORS solution spread like wildfire.
Mrs Masalkar has gained popularity and respect and now mothers knock at her door, even at
midnight. to ask for oral rehydration salts for treatment of diarrhoea in their children.
This proves that nothing can be more convincing than practical and simple demonstration. L. D. Puranik, K. E. M. Hospital Research Centre, Sardar Mudliar Road, Rasta
Peth,
Pune 411011, India.
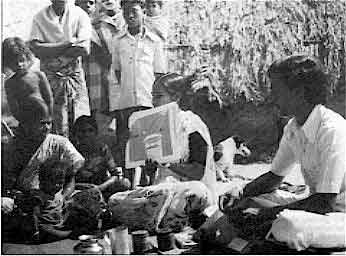
Health education about oral rehydration therapy in a village near
Pondicherry,
India.
This photograph was entered for our photographic competition by Dr R. D.
Bansal,
Professor of Social and Preventive Medicine, Jawaharlal Institute of Postgraduate
Medicine, Education and Research, Pondicherry 605006, India.
|
 |
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 22 September
1985  2 Page 3 4 2 Page 3 4
Reviews
Transitional diarrhoea in newborn infants. P. P. Maiya, M. Jadhar, M. J. Albert and
M. Mathan. Department of Child Health and The Wellcome Research Unit, Christian Medical
College Hospital, Vellore, India. Annals of Tropical Paediatrics, 1985, vol. 5, pp 11-14. Out of more than 3,000 full-term, breastfed infants not kept in the hospital nursery,
about two per cent developed acute watery diarrhoea between their third and sixth days of
life. Laboratory investigations showed that rotavirus and enteropathogenic serotypes of E.
coli could be found equally frequently in the stools of infants with diarrhoea and infants
without diarrhoea. Salmonella, shigella and cholera organisms were not found; other
possible pathogens, such as Cryptosporidia do not appear to have been looked for.
The diarrhoea was always brief (usually less than three days) and none of the babies had
signs of infection or dehydration. All received some extra fluid in addition to being
breastfed and all made a complete clinical recovery. It is suggested that such a
self-limited episode of diarrhoea soon after birth is not necessarily due to any type of
rotavirus infection. It could be caused by slow adaptation to breastmilk intake. The
microbial colonization of the gut that takes place after birth may also contribute to this
transitional diarrhoea. The syndrome obviously deserves further scientific investigation.
It is, however, clear that breastfeeding plays an important protective role in diarrhoea
among newborn infants and should always be encouraged. The following article may also be of interest to some readers: Enteropathogenic Eschericia coli (EPEC) and enterotoxigenic (ETEC) related
diarrhoeal disease in a neonatal unit. M. Adhikari, Y. Coovadia and J. Hewitt. Department
of Paediatrics and Child Health and Department of Microbiology, Faculty of Medicine,
University of Natal, Durban, Republic of South Africa. Annals of Tropical Paediatrics,
1985, vol. 5, pp 19-22. Clinical immunity after neonatal rotavirus infection. Bishop R. F. et al, 1983 New
England Journal of Medicine 309 pp 72-76. Rotavirus infection in newborns does not prevent further rotavirus infection, but does
prevent serious diarrhoea. Usually, rotavirus infection causes acute watery diarrhoea in
children between six months and three years of age. Sometimes newborn infants in hospital
nurseries are infected with rotavirus but many, especially the full-term babies, do not
show signs of diarrhoea. In Melbourne, Australia, a group of young children who were known
to have been infected with rotavirus in the newborn period were compared with a group who
were not infected. On follow-up over the next three years, about half the children in both
groups developed rotavirus infections. Those who had been infected with rotavirus during
the newborn period had much less diarrhoeal illness and, if they did develop diarrhoea,
they were less ill.
Infection with rotavirus during the newborn period does not prevent reinfection
occurring later but it does protect against severe disease from the rotavirus
re-infection. Editor's note: Dr Ruth Bishop wrote a review for DD on rotavirus research (DD14, August 1983). Issue 16 (February
1984) included an article by Dr T. Flewett on expectations for a rotavirus vaccine.
Readers might also be interested to refer to: Interventions for the control of
diarrhoeal diseases among young children: rotavirus and cholera immunization. I de Zoysa
and R. G. Feachem, 1985, Bulletin of the World Health Organization: 63(3): 569-583. ORT in infants
Dr Menakshi Mehta and her colleagues of the L.T.M.G. Hospital, Sion, Bombay 400022,
have used oral rehydration therapy with babies of less than three months of age. ORS
solution (the WHO formula) was alternated with water, glucose water or breastmilk. None of
these children had periorbital oedema or other signs of overload of salt or water, even
though the possibility was anticipated and specifically looked for. (Personal
communication). Also see="#page4">pages 4 and 5. Nepal: preventing dehydration
|
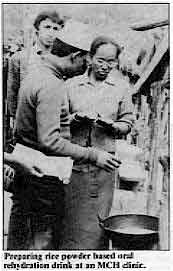
Preparing rice powder based oral rehydration drink at an MCH clinic.
Ruth Angove has written from Nepal to tell us about the successful use of an oral
rehydration drink made with rice powder, salt and water. Health workers and mothers were
shown how to mix and give the drink to both children and adults with diarrhoea. The rice
powder drink is very useful in the prevention of dehydration, the ingredients are readily
available locally and the easy recipe uses familiar ingredients and methods. Rice powder
or flour is a traditional weaning food in Nepal and the majority of both children and
adults who were given the rice powder oral rehydration drink greatly enjoyed the taste.
|
|
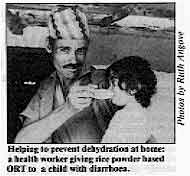
Helping to prevent dehydration at home: a health worker giving
rice powder based ORT to a child with diarrhoea. Further reading: Molla A M 1984 Advances with rice-powder ORS. Diarrhoea
Dialogue,="dd19.htm#page7">Issue 19, page 7. Molla A M et al 1982 Rice powder
electrolyte solution as oral therapy in diarrhoea due to Vibrio cholerae and Escherichia
coli. The Lancet, 12 June pp 1317-1319.
|
 |
Ruth Angove, formerly Nutrition Advisor, United Mission to Nepal, PO Box 126,
Kathmandu, Nepal.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 22 September
1985  3 Page 4 5 3 Page 4 5
| Dealing with diarrhoea in newborn infants |
Approaches to rehydration
Daniel Pizarro reviews current knowledge about use of
oral rehydration therapy in neonates. Developing a standard approach to the rehydration of newborn infants who have diarrhoea
is not easy. Scientists still seek to establish an accurate picture of the neonatal fluid
and electrolyte metabolism and current concepts are constantly being updated by new
discoveries. Not only dehydrated but also healthy newborn infants may show a wide
variation in blood serum sodium levels. The kidneys of premature infants (those born too
early) have a poor capacity for sodium reabsorption during the first two weeks of life,
whereas full-term infants (born on or near the expected date) are able to reabsorb more
sodium than water during the same period. Although such observations might appear to
complicate the management of fluid and electrolyte disturbance in newborns with diarrhoea,
evidence from several clinical studies indicates that these infants can be treated safely
and effectively by means of oral rehydration therapy (ORT). Diarrhoea has very different causes in developed and developing countries. In the
former, diarrhoea in the newborn is unusual and may be due to inborn errors of metabolism
such as congenital enzyme deficiencies. It may also be associated with severe infections
like septicaemia or necrotizing enterocolitis, which require appropriate antibiotic
treatment in addition to rehydration. In developing countries, however, diarrhoea is a
relatively common problem among newborns, particularly if they are fed breastmilk
substitutes by bottle. The diarrhoea is almost universally infectious in origin and has
been reported in association with specific pathogens, for example, rotavirus,
enterotoxigenic E. coli (ETEC) and cryptosporidium. Successful use of ORT Since the first report in 1976 of the successful use of ORT in neonates, many studies
have confirmed the effectiveness of this therapy. In addition, it has been found that
newborns with either hyponatraemic or hypernatraemic dehydration can be successfully
treated with the same rehydration schedule. Hypernatraemic dehydration refers to patients
with a high serum sodium, greater than 150 mmol/litre, and hyponatraemic dehydration to
patients with a low serum sodium of less than 130 mmol/litre. The standard WHO recommended
oral rehydration salts (ORS) solution containing 90 mmol/litre of sodium should be used.
Calculate the volume of ORS solution required for rehydration. In moderate to severe
dehydration, this is 70-100 ml per kg body weight. This amount should be given gradually
over a few hours, either by cup and spoon, or by bottle if the infant is already being
artificially fed. After this initial rehydration period, the diarrhoea may continue and
the rehydration must be maintained by giving the infant 10 ml per kg body weight of ORS
solution, alternating with an equivalent amount of plain water after each liquid stool
until the diarrhoea stops. Feeding should begin as soon as the initial rehydration period
is completed.
|
This three weeks old infant recovered in eight hours with ORS
after being 10 per cent dehydrated.
At the National Childrens' Hospital (NCH) in San Jose, Costa Rica, ORT with 90
mmol/litre sodium and glucose electrolyte solution is the routine therapy for dehydrated
neonates. More than 300 newborn patients - 95 per cent of all newborns given ORT - have
been successfully treated without complications. From this experience, it appears that
there is no need to consider 'special techniques' to rehydrate neonates, but care is
needed not to overload them with ORS solution.
|
 |
Importance of breastfeeding Practical experience at the NCH over the past seven years has shown that newborn
infants with diarrhoea, who show little or no sign of dehydration, can be treated by
breastfeeding alone. Those with moderate or severe dehydration receive ORS solution alone
during the rehydration phase which lasts less than eight hours. Once the infant is
rehydrated, breastfeeding is continued, along with ORS solution given after each liquid
stool. In infants who are not breastfed, their usual formula, diluted 1:1 with water, is
given once rehydration is achieved, and ORS solution is given after every liquid stool
passed. An alternative is to give full strength formula and alternate giving ORS solution
and plain water after each liquid stool passed. Where possible breastfeeding should be
encouraged. This treatment approach has been successfully used for neonates with diarrhoea admitted
to the NCH. Five per cent or less have needed to be treated intravenously - severely
dehydrated infants with shock, intestinal obstruction or paralysis, or with persistent
vomiting. The Costa Rican experience has been successfully shared by other countries,
Venezuela (310 cases), Mexico (172 cases), Paraguay (23 cases), Argentina (10 cases) and
El Salvador (10 cases). In Paraguay and Egypt, as well as in Costa Rica, low birthweight
infants weighing as little as 1050 gm have been successfully treated using this regime and
giving the fluids by nasogastric tube. Dr Daniel Pizarro, Chief, Emergency Service, Hospital National de Ninos, San Jose,
Costa Rica.
*Neonates or newborns are infants from birth to 28 days after. Further reading: 1. Arrant Bs Jr, 1982. Fluid therapy in the neonate - concepts in transition.
Journal of Paediatrics 101 387:389.
2. Pizarro D et al, 1979. Oral rehydration of neonates with dehydrating diarrhoeas.
Lancet 2 1209: 210.
3. Pizarro D et al, 1980. Oral rehydration of infants with acute diarrhoeal
dehydration - a practical method. Journal of Tropical Medicine and Hygiene 83 241:245
4. Pizarro D et al, 1983. Treatment of 242 neonates with dehydrating diarrhoea with
an oral glucose-electrolyte solution. Journal of Paediatrics 102 153:156.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 22 September
1985  4 Page 5 6 4 Page 5 6
| Dealing with diarrhoea in newborn infants |
Careful management
Nisar A. Mir considers the special problems that can
arise when treating diarrhoea in newborn infants. It is essential to:
- recognise diarrhoea immediately
- prevent dehydration occurring or undertake early rehydration
- treat any other illness in the infant
- restore adequate food intake as soon as possible.
Rapid dehydration The physiological characteristics of the newborn baby or 'neonate' result in more rapid
dehydration during diarrhoea than occurs with older infants. The more premature the
infant, the greater the risk of severe dehydration. Reduced fluid intake may result if the
neonate is unable to take breastmilk from its mother due to poor sucking ability or
lethargy due to illness. The fluid loss from the body caused by diarrhoea and vomiting may
be increased by water loss through the skin due to fever and from the upper respiratory
tract by rapid breathing, especially in hot, dry climates. Local treatment
 |
Bottle-fed full-term newborn needing rehydration in neonatal unit. Regional and cultural factors should be considered in the management of diarrhoeal
diseases in neonates. For example, in Benghazi, Libya, where heat-caused fluid loss in
newborns makes early rehydration essential when an infant also has diarrhoea, the
electrolyte content of the drinking water is higher than normal and extra care is needed
in preparing rehydration fluids. It has, therefore, been possible to treat mildly
dehydrated infants with diarrhoea with pre-measured glucose and bicarbonate fortified
drinking water, rather than resorting to ORS solution.
|
In Kashmir, however, the winter
temperatures are very low, and many parents do not like to give ORS solution because they
believe cold drinks will cause the common cold. Tea is recognized as hot and not
considered likely to cause a cold. Based on this traditional belief, health staff advise
mothers to feed infants who have diarrhoea with milkless 'Noon-chai' - the popular Tibetan
tea made with salt and bicarbonate of soda and fortified with glucose (see="dd21.htm#page3">DD21 page three). Suitable and modified home
drinks are now accepted as having a useful place in the early management of diarrhoea. Danger signs for the newborn
While most small infants with diarrhoea can be managed at home, either with locally
available remedies similar to those described above or ORS solution, some need to be
referred to a health facility for further treatment and investigation if they do not
improve. Signs to indicate that this is necessary include:
- bloody diarrhoea
- poor sucking or swallowing - often if the infant is very premature, ill or unconscious
- vomiting or shock
- severe diarrhoea with dehydration of more than 5 per cent of body weight.
Referral to a hospital is also indicated if the infant shows no sign of improvement
after treatment at home for 24 hours, or if the mother, for any number of reasons, is
having difficulties giving oral rehydration therapy. Drug therapy Antibiotics and other drugs do more harm than good in newborn infants and should never
be given. The only possible exception is where the cause of the diarrhoea has been clearly
identified as shigella, campylobacter or giardia. Early feeding The newborn infant should be breastfed as soon as possible after birth. Feeding both
during and after the diarrhoea is essential. Newborns have very limited nutritional
reserves to combat starvation and quickly become hypoglycaemic. After an episode of
diarrhoea, an infant needs extra food intake to rebuild reserves and prevent the cycle of
diarrhoea and malnutrition. Breastfeeding should always be encouraged. Bottle-feeding
carries a high risk of infection and good hygienic standards must be observed to prevent
recurrence of diarrhoea. In some cultures, inappropriate semi-solid and solid foods are
sometimes given to the very young infant with disastrous consequences. Management of diarrhoeal disease in the newborn requires accurate diagnosis and quick
responses from health personnel and mothers, with emphasis on preventing dehydration by
increasing fluid intake and on ensuring adequate calorie intake through suitable feeding.
Neonates with diarrhoea should be closely monitored to ascertain those who need early
referral to a hospital or other health facility. Dr Nisar A. Mir, Department Neonatology, Sher-I-Kashmir Institute of Medical
Sciences, P. B. 27, Srinagar 190011, India.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 22 September
1985  5 Page 6 7 5 Page 6 7
Successful ORT
Bert Hirschhorn and Ahmed Youssef
lists some important points for doctors, nurses and other health practitioners to remember
when giving oral rehydration therapy.
- A health worker must show the mother how to mix and give the oral rehydration
solution. This is equally important in the clinic and at home, to ensure understanding and
correct use.
- ORT does not stop diarrhoea; it stops and reverses the dangerous dehydration caused by
diarrhoea. In 50 per cent of children under the age of three, treated with ORT, diarrhoea
will continue for three to four days or sometimes even longer. This must be explained to
mothers. Once children have been properly rehydrated, they should be given about 400-500cc
of ORS each day, as well as being fed, to maintain rehydration until the diarrhoea stops.
The child with watery diarrhoea
- A child who has passed just three watery stools will have lost 150-300cc of fluid (water
containing essential body salts). This dehydration represents a loss of 1.5 - 3 per cent
of body weight in a child weighing 10 kg. Once 2 per cent of weight is lost, the body
reacts to conserve water and electrolytes (body salts). The recommended WHO/UNICEF formula
for ORS contains 90 mmol/litre of sodium and is the correct treatment for dehydration. If
packets of ORS are not available, an equivalent home-made sugar and salt solution should
be used. Plain water, or other drinks which contain little salt, are not recommended for
dehydrated children, except where salt and sugar are unobtainable. In such extreme
circumstances, any drink available should be used to treat a dehydrated child.
- The child will often pass a large watery stool just after ORT has been started. Mothers,
and even some health workers, may believe the ORT has increased the diarrhoea. This is not
true. What is happening is called the 'gastro-colic' reflex in which anything entering the
stomach causes the bowel to expel its contents. ORT does not increase diarrhoea except
when too much sugar is used.
The vomiting child
- If a child vomits, stop giving ORS for five to ten minutes. Then give ORS at the rate of
one teaspoonful (5cc) a minute. This may seem slow but provides 300 cc per hour and will
nearly always prevent further vomiting.
- The amount vomited is usually smaller than the quantity of ORS taken. If the child
vomits less than four times an hour, enough ORS is probably being retained. If vomiting
persists (more than four times per hour), use a nasogastric tube to give the ORS.
The thirsty child
- A thirsty child is a dehydrated child. Once rehydration is complete, children usually
refuse more ORS, unless hungry and not being offered food.
- A child with hypernatraemia (high blood serum sodium content) may drink a large amount
very quickly but seldom vomits in spite of this rapid intake. The child's thirst is a good
guide to successful ORT.
The child who refuses ORS This may be because:
- the child is no longer dehydrated and wants food or sleep.
- the child is still dehydrated but tired and needs to be patiently persuaded to drink
(see below).
- the child is irritable because of some other cause such as another infection. A
nasogastric tube may be the answer but first try to give ORS with a plastic dropper by
slipping this between the child's clenched teeth and cheek. The child will usually swallow
as a reflex rather than spit out the ORS.
The weak or drowsy child
- The child who is conscious but too weak to drink may need to be rehydrated by
nasogastric tube or by intravenous infusion if in shock. It is worth first trying the
plastic dropper technique (or a 5cc plastic syringe without the needle) to squirt the ORS
into the child's mouth.
The sleeping child
- Seriously dehydrated children sometimes sleep with their eyes partly open so that only
the whites show. Sleep during rehydration means one of two things. Either the child is not
recovering quickly enough and is becoming unconscious and needs to be woken up and given
more ORS; or rehydration is complete and the child is ready for normal sleep.
Abdominal distension A distended abdomen in children with diarrhoea is caused by:
- giving salt solution without potassium, either orally or intravenously
- giving anti-motility drugs
- giving cow's milk feeds to a child with lactose intolerance
- surgical problem - this is rare.
Newborns
- Most newborns can take spoon feedings. If not, a plastic dropper or plastic syringe
without the needle can be used to give ORS. Newborns are often seen to suck at the tip of
the dropper.
The child on a nasogastric tube Use this:
- at night in hospital when both mother and child need sleep.
- in persistent vomiting when the child is not in shock.
- in emergency - for example while setting up an IV in a shocked child or transporting the
child to hospital.
When using a nasogastric drip, mark the starting level of the fluid with a piece of
adhesive tape. Write the time on this and mark in the same way the correct level for each
following hour. This is to check the drip is working at the correct rate. The child in shock See above - the weak or drowsy child.
- Give ORS in addition to the IV if the child is conscious, and stop the IV as soon as the
child is drinking well.
Feeding the child with diarrhoea
- Breastfeeding should be continued throughout ORT.
- The child with diarrhoea needs extra feeding as soon as rehydration is complete. If
bottle fed, give smaller amounts of the normal feed more frequently. There is no advantage
to the old method of 'slow reintroduction' of milk and the mother may dilute the feeds for
far too long a time. Older children should be given their normal foods but fed more
frequently for a few weeks. Yoghurt, orange juice, bananas and coconut water are
recommended to bring up the potassium level. (Do not give coconut water during rehydration
as its potassium content is too high).
Dr N. Hirschhorn, JSI, 210 Lincoln Street, Boston, MA. 02111, USA.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 22 September
1985  6 Page 7 8 6 Page 7 8
| Country profile: Mozambique |
Training nurses
Alfredo Pisacane looks at how a training programme aimed
at improving nurses' understanding and use of oral rehydration therapy in hospital has
contributed to a decrease in mortality due to diarrhoea in one hospital in Southern
Mozambique. Whether people die at home or in hospital in developing countries depends on the
setting (urban or rural), the local culture and the availability and accessibility of
health services (1). In the city of Xai-Xai in Southern Mozambique, with 40,000
inhabitants, between 50 and 60 per cent of the total number of child deaths take place in
hospital (2). Diarrhoeal diseases remain the first cause of admission (excluding the
winter months when the prevalence of measles is high) and, up to 1981, diarrhoea caused 21
per cent of all child deaths and 20 to 25 per cent of children admitted with diarrhoea
died. Our team (one paediatrician and four nurses) tried to find out the reasons for these
disturbing figures. We decided to start six months of in-service training to improve our
collective knowledge of the problems of the paediatric ward and the needs of the patients.
Part of the training was related to diarrhoeal diseases. Towards a scientific approach The training consisted of daily 15 minute meetings of one doctor and one nurse and
weekly general meetings of one hour. In the short daily meetings, we observed the children
together checking the effects of dehydration on vital bodily functions such as pulse rate,
respiration rate, blood pressure, urine output and weight; and evaluated signs of
dehydration. At our general meetings, we tried to agree on the correct management of a
situation, and we wrote short notes about our discussions which now constitute a manual
for in-service training*. We also obtained slides of nurses carrying out a definite task,
for example, showing mothers the quantity of oral rehydration solution to give to their
children, checking the weight at the beginning of and four hours after starting
rehydration and checking urine output. In this way, we obtained after some weeks a more
scientific approach to diarrhoea treatment as is shown in the following sample from our
manual: What nurses must know:
- physical signs of dehydration
- vital signs affected by dehydration
- how frequently to check vital signs and weigh the child
- how to carry out oral and IV rehydration
- how to assess the improvement or the worsening of the condition of the child
What nurses must be able to do:
- check vital signs at admission and at least every four to six hours
- assess physical signs of dehydration at admission and after four to six hours
- check urine output if requested by the doctor
- give (and explain carefully to the mothers how to give) the right quantity of oral
rehydration solution over the right period of time
- start IV infusion when requested by the doctor
What nurses must be able to decide:
- when to call the doctor in relation to deterioration of physical signs of dehydration or
vital signs, or decrease in weight.
- if there is frequent vomiting, whether to continue with ORT or call the doctor to start
an IV infusion
The evaluation After six months, we decided to evaluate our training. The personnel were the same both
before and after the training; criteria for admission and for IV rehydration remained the
same; the age distribution of the patients and the incidence of diarrhoea did not change. Even if it is difficult to conclude that nurse training is the only factor for the
observed decrease in child mortality in hospital due to diarrhoea, it seems to play an
important role in our situation. In other countries like Mozambique, where the death rate for diarrhoeal diseases is
still high in spite of diffuse practice of ORT, improved training of nurses could be a
cheap and effective means of intervention.
|
Indicators of nurse performance
Nurses' recording of data for children with diarrhoea. First trimester 1981 and 1982.
|
|
1981 |
1982 |
| Admissions |
30 |
34 |
- pulse checked during first 24 hours
|
0 |
24 |
- weight checked after six hours of rehydration
|
0 |
24 |
- diuresis checked during first 24 hours
|
0 |
18 |
|
|
0 |
24 |
|
|
1 |
15 |
Indicators of health status. First trimester 1981 and 1982.
|
|
1981 |
1982 |
| Total admissions |
450 |
553 |
- admissions due to diarrhoea
|
30 (6.6%) |
34 (6.4%) |
- children treated with IV infusions
|
5 |
5 |
- children who died - all causes
|
35 |
17 |
- children who died from diarrhoea
|
9 |
1 |
- case fatality rate for diarrhoea
|
30% |
3% |
|
Dr Alfredo Pisacane, Instituto di Paediatria Universita di Napoli Via
Surgio Pansini 5, 0131 Naples, Italy * For further information about the manual, write to Dr Pisacane at the the
doctor address above. 1. Puffer RR and Serrano CV 1985. Pattern of mortality in childhood. Pan American
Health Organisation Scientific Publication No. 32.
2. Registry General, Xai-Xai, Mozambique 1981.
|
|
DDOnline
Dialogue on Diarrhoea Online Issue 22 September
1985  7 Page 8 7 Page 8
Convinced about ORS The participants in our first national training session in Management of Acute
Diarrhoea were all physicians involved in diarrhoea case management. The evaluation of the
training course showed that everybody shared the view that it was the practicals - the
administration of ORS, involving the mothers in spoon-feeding of children with mild to
moderate dehydration - that had convinced them of the acceptability and effectiveness of
ORS. Dr Mariam Claeson, WHO, P. O. BOX 3069, Addis Ababa, Ethiopia.
Unnecessary prescribing I work in government service in Iran and I have read every issue of Diarrhoea
Dialogue. You present everything in an informative and creative way. I have found
whilst working in Iran that most of the doctors in private and government service
prescribe multiple antibiotics for simple diarrhoea. This type of attitude may be due to
lack of confidence or lack of recent information. Diarrhoea Dialogue solves both of
these problems by giving up-to-date scientific information and showing them how to treat
diarrhoeal disease confidently with ORT. The doctors would then not waste costly
antibiotics on their patients, and would save the patients money. In the long run they
would also prevent patients from becoming immune to antibiotics. If every doctor in the
developing world treated patients with diarrhoea properly, countries would save tons of
antibiotic syrups such as furoxone, ampicillin, chloramphenicol and neomycin . Here in my part of Iran, patients like a lot of medicine even for a little illness. If
a village mother brings her child with diarrhoea to the doctor, she expects him to
prescribe at least half a dozen drugs. She takes it for granted that antibiotics will cure
her child, and neglects the main part of the treatment - rehydration. In future, with the
enlightenment of the public with Diarrhoea Dialogue, attitudes may change. Dr N M Reddy, Khosf, Birjand, Korasan Province, Iran.
Local remedies CRS in Mauritania operates a monthly food and nutrition (F&N) programme serving
approximately 40,000 pre-school age children and 30,000 mothers country-wide. Health and
nutrition education is an integral part of the programme and diarrhoea management is
particularly important in this environment. The Mauritanians who work in the F&N
centres are trained to teach mothers about dehydration and ORT. They know the recipe for
the sugar/salt solution and are familiar with the UNICEF packets which are widely
distributed to health centres in Mauritania. Unfortunately Mauritanian women are often
reluctant to give water to a child suffering from diarrhoea, particularly during the cold
season, when water is completely withheld from a sick child. Most Mauritanian mothers do traditionally treat diarrhoea with a rice porridge often
containing seeds from the baobab fruit. This can be an effective treatment. They
additionally give their sick children a beverage of diluted sour milk (usually made from
powdered milk and soured with yoghurt) which is sweetened with sugar. Our question is as
follows. Can an effective ORT solution be made by simply adding a pinch of salt to the
sour milk beverage or by adding sugar and a pinch of salt to a diluted rice porridge?
Would it be safe and effective to add a UNICEF packet to either of the two? By promoting and strengthening already existing means of diarrhoea management we feel
we can achieve greater results. We look forward to your reply. Jill Gulliksen, Food and Nutrition Project Manager, Catholic Relief Service, B. P.
539, Nouakchott, Mauritania.
Editor's note: We asked Dr Mahalanabis of the Diarrhoeal Diseases Control
Programme at WHO to answer Jill Gulliksen's queries. "Can an effective ORT solution be made by simply adding a pinch of salt
to the sour milk beverage?"
As we understand it, the sour milk beverage refers to diluted yoghurt with added sugar.
Although we have not studied this, we believe that such a beverage with an appropriate
amount of added salt could be an effective ORT solution for early home therapy to prevent
dehydration. "Can an effective ORT solution be made by adding a pinch of salt to a diluted
rice porridge?"
Evidence so far suggests that rice powder suitably cooked and diluted (i.e. to contain
30 to 50 gm dry rice per litre), with added salt, may be useful for early home therapy to
prevent dehydration in infants and children older than three months. Sugar should not be
added to such a solution. The efficacy of such a solution in infants less than three
months old has not been determined. It should be noted that neither of the above solutions are suitable for treating
dehydration. For treatment, a more complete formulation such as the one recommended by
WHO/UNICEF should be used. "Would it be safe to add a UNICEF packet to either of the above
solutions?"
It is not advisable to add UNICEF packets to either diluted sour milk with or without
added sugar, or diluted rice porridge with or without added sugar. WHO/UNICEF packets
should be made up in water used for drinking. Adding such a packet to either of these
solutions will increase the carbohydrate concentration, which is undesirable, and in the
case of the diluted sour milk could also increase the sodium concentration.
DD for training I am a doctor from Bangladesh working with refugees in Somalia. We are involved in
primary health care and my responsibility is to train and supervise the medical staff
working in the refugee camps. Diarrhoea is the major killer. I received some issues of DD
from a friend of mine and I believe it will be very useful for me and my staff. Please
include my name on your mailing list for five copies of each issue. Dr Akran Hossain, P. O. Box 1502, Mogadishu, Somalia.
|
In the next issue . . .
DD 23 will focus on diarrhoea, growth and
nutrition
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Executive editor Denise Ayres
Editorial assistant Kathy Attawell
Editorial advisory group
Professor David Candy (UK)
Dr I Dogramaci (Turkey)
Professor Richard Feachem (UK)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Professor Leonardo Mata (Costa Rica)
Dr Mujibur Rahaman (Bangladesh)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), UNICEF and WHO
|
Issue no. 22 September 1985
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
updated: 23 August, 2019
|