|
| |
Issue no. 27 - December 1986
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea
Online Issue 27 - December
1986
|
DDOnline
Dialogue
on Diarrhoea Online Issue 27 December 1986  Page 1 2
Page 1 2
Diarrhoea and gut parasites
 |
Clean hands help to prevent parasitic infections.
Parasites rely for food and shelter on other living things such as people and animals.
All humans have harmless commensals living in their intestines and some play a useful part
in the digestive process. But there are also harmful intestinal parasites which can cause
gut damage leading to diarrhoea, bloody stools, abdominal pain and weight loss. This issue
of DD discusses various common and less common gut parasites which are associated
with diarrhoea and malnutrition in different parts of the world. ORT - the life saver Acute watery diarrhoea, caused by bacteria, viruses - and also by the parasite
cryptosporidia (see="#page4">page 4) - can bring about rapid death from
dehydration. This type of diarrhoea is a major killer of young children in developing
countries. Oral rehydration therapy (ORT), started early enough and given in adequate
amounts can save lives by preventing or treating dangerous dehydration, allowing the
body's natural defence mechanisms to overcome the infection. Continued and proper feeding
during acute diarrhoea helps in this process (see DD 23). Drug
treatment is rarely indicated, except for dysentery (bloody diarrhoea) due to infection
with Shigella bacteria (see DD 25).
|
The long term answer In contrast, intestinal parasitic infections associated with diarrhoea are less
immediately dangerous and their significance should not be over-stressed. Nevertheless,
the part parasites may play in chronic diarrhoea and malnutrition must not be overlooked.
Not all produce obvious diarrhoea, although there are often noticeable changes in the
stools - looseness, frothiness, streaks of blood and mucus - and some general debility. A
parasitic infection should always be suspected where children fail to gain weight and lack
energy, especially in areas where the environment is known to be contaminated. Outside the
body, intestinal parasites can survive for long periods in the form of cysts and infection
is carried by food, water and unclean hands. Within the body, the natural defence
mechanisms have relatively little effect on parasites and immunity is slow to develop.
Where health is being seriously affected, drug treatment is needed (see articles in this
issue on="#page7">amoebiasis,="#page6">giardiasis and trichuriasis) but treatment is not likely to prevent reinfection if the
environmental circumstances remain unchanged. The long term answer is the same for all causes of diarrhoeal illness: improved hygiene
both within and outside the home. Basic health education about the importance of
handwashing, safer drinking water, safer faeces disposal and safer food handling can help
considerably to diminish the contribution made by intestinal parasites to ill health in
the Third World, especially among small children. KME and WAMC
|
In this issue . . .
- DD describes the relationship between various parasitic infections and diarrhoea.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 27 December 1986
 1 Page 2 3 1 Page 2 3
|
Refugee camps: reducing diarrhoea In Somalia, the Refugee Health Unit (RHU) of the Ministry of Health is responsible for
over 700,000 refugees. The peak incidence of diarrhoea, 55 to 65 per cent of all cases and
deaths, occurs every year between March and June. A campaign to reduce diarrhoeal deaths,
started in 1984 in all regions, has halved refugee deaths from diarrhoea in one region,
Hiran. The campaign included:
- Training of all doctors and nurses and community health workers (CHW) on the management
of diarrhoea with oral rehydration salts (ORS).
- Establishment of under-fives clinics in every refugee camp. Every child taken to a
clinic is weighed and measured. Malnourished children (70-80 per cent of the recommended
weight-for-height) are sent to a supplementary feeding centre. Those who are less than or
equal to 70 per cent of the recommended weight-for-height are taken to an intensive
feeding centre.
- Every child in the refugee camps has a road-to-health weight card so that growth and
immunisation status can be checked.
- Mothers are taught about diarrhoea, dehydration, preparation of ORS and infant feeding.
They are shown how to make up a litre of oral rehydration solution using cup sizes
available in the camps (for example, if the mother has a 200 cc cup, she is told to add
five cups of water to one sachet of ORS).
During '' the months of diarrhoea", from March to June 1984, there were 5,352
cases of diarrhoea in Hiran, and 62 deaths due to diarrhoeal disease. In the same period
of 1985, only 36 died out of a total number of 4,652 cases of diarrhoea - a fall in
the case fatality ratio from 1.16 per cent to 0.77 per cent. Deaths from respiratory
infections now outnumber deaths from diarrhoea for the first time in the history of the
RHU.
A survey of 3,000 mothers revealed some problems with their understanding of ORS. While
90 per cent knew what an ORS packet was, and 80 per cent said it was for rehydration, only
30 per cent mixed the contents of the packet with the correct amount of water. This was
partly because they believed that adding water to ORS would 'dilute' the medicine, and
partly because the teaching sessions had not included practical demonstrations by mothers
mixing up oral rehydration solution in front of the health worker. To overcome the problem
a new campaign, with community participation, was organised, including marking a suitable
household container to measure 1 litre.
Dr Hussein M. Mursal, Refugee Health Unit, Ministry of Health, c/o UNHCR, PO Box
2925, Mogadishu, Somalia.
|
Refugee camps: setting up a laboratory Establishing a Refugee Camp Laboratory: A Practical Guide by Warren Johns is a
new manual for expatriate and local laboratory technicians involved in establishing
laboratories in refugee camps. The manual will also be of interest to staff in UN
agencies, government and non-government organisations as well as to doctors, nurses and
village health workers. It includes useful appendices on Laboratory Equipment Suppliers,
Textbooks and Slides, Further Reading, Refugee Laboratory Kit, and Materials for
Establishing the Laboratory. Available from: Overseas Department, The Save the
Children Fund, 17 Grove Lane, London SE5 8RD, UK. Price: £2.50 per copy (plus
postage of £1.00 for Europe and the Middle East, £1.50 elsewhere, per copy). Donation to DD We would like to acknowledge a donation for DD from Memisa Medicus Mundi in the
Netherlands. We greatly appreciate this generous support which has enabled extra copies of
the Dialogue to be printed and distributed. Feeding and diarrhoea A report on Nutritional Management of Acute Diarrhoea in Infants and Children is
available from the National Academy of Sciences Press, National Research Council,
Commission on Life Sciences, 2101 Constitution Avenue, Washington DC 20418, USA. Price:
US$ 3.00 to readers in the United States and Canada; free of charge to readers from other
countries. Vitamin A publication Vitamin A + Sieve is a new twice yearly publication which provides information
on the latest research on vitamin A deficiency, the diseases it causes, and growing and
preserving foods rich in vitamin A. Each issue will review current literature and
research, as well as a specific topic of concern. Published by Prevention magazine and the
Rodale Institute (a non-profit group aiming to improve agriculture and food systems), the
newsletter is aimed at research scientists, field workers and administrators. It is
available free of charge to DD readers. Contact Janet Glassman, Rodale Press
Information Services, 33 East Minor Street, Emmaus, PA 18049, USA. Symposium proceedings The proceedings of the Ciba Foundation Symposium No.128 on Novel Diarrhoea Viruses held
in July 1986, and chaired by Dr Ruth Bishop, will be available in early 1987 from: John
Wiley & Sons, Baffins Lane, Chichester, Sussex PO19 IUD, UK. Price: £27.50. Nutrition poster The Office de Recherches sur L'Alimentation et la Nutrition Africaine has produced a
poster (in French) listing 150 African foodstuffs and their calorie and vitamin content.
The poster also shows the daily requirement of vitamins and calories for adults,
teenagers, children and infants. Available from: Dr Ndiaye, Documentation / ORANA, BP
2089, Dakar, Senegal. Price: US$ 12.00.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 27 December 1986
 2 Page 3 4 2 Page 3 4
An intestinal zoo
Anthony Radford describes some of the most common
intestinal parasites, particularly those which may cause diarrhoea, and some of the
factors predisposing towards infection. More than half of the people in the world carry around inside them an 'intestinal zoo'
of parasites: protozoa (microscopic, single-celled organisms), and helminths (worms),
which come in all sizes. Individuals may have from tens to hundreds of parasites of
several different species in their intestine. Most people are unaware of these internal
'passengers' but some intestinal parasites can cause diarrhoea, and other associated
problems. Transmission The great majority of intestinal parasites are transmitted to humans by swallowing the
egg or cyst forms of the parasite in contaminated food (e.g. roundworm), in water (e.g.
giardia), or through contamination of the hands by infected faeces or faecally
contaminated soil. Others, like the pig and beef tapeworms, are transmitted by eating
infected meat which has been inadequately cooked. Most people who live where intestinal
parasites are common (endemic) are frequently reinfected. Factors influencing prevalence and transmission The prevalence of intestinal parasite infection is influenced by:
- poor sanitation and hygiene
- the age of the individual and any previous exposure to the parasite:
Infants
are not commonly infected until the middle of the first year of life because they are
largely protected from contaminated water, food and soil by an exclusive breastmilk diet,
and by being carried around; and, at least for some of the protozoal infections, mothers'
milk may carry protective antibodies. Because very young children live and play in
contaminated environments, their rates of infection tend to be higher. Rates tend to fall
as children acquire some immunity, learn to walk, and learn about hygiene.
- the particular characteristics and number of parasites:
At least one parasite,
E. histolytica, occurs as both pathogenic (illness producing) and non-pathogenic strains.
The presence of the former results in much disease in some communities, whilst the latter
cause little or no disease.
- climate:
Warm, moist conditions are required for some parasites to develop.
Thus, Australian Aboriginals in Northern Australia, where it is warm and moist, suffer
more parasitic infections than those in drier, more southern areas, even with the same
sanitation and hygiene patterns.
- the presence of animals known to be involved in transmission of parasites.
Signs and symptoms
|
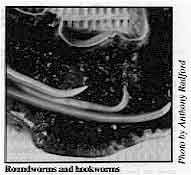
Roundworms and hookworms
In most people, many parasitic infections do not produce clinical symptoms. In some,
protozoal parasite infections can cause abdominal pain and diarrhoea or dysentery (bloody
diarrhoea). Chronic infections, especially with giardia, may produce a malabsorption
syndrome with intermittent frothy, foul-smelling, loose bowel actions, together with
weight loss and, in children, growth retardation.
|
 |
Most of the symptoms of worm infestation are due to the competition between worms and
host for food, or to blood and protein loss or intestinal obstruction. Poor general health
is also common with heavy parasitic infections. Anthony Radford, Professor of Primary Care and Community Medicine, The Flinders
University of South Australia, Bedford Park, South Australia 5042. Parasites and diarrhoea: research needs The 1985 meeting of the WHO Diarrhoeal Disease Control Programme Technical Advisory
Group recommended research in the following areas:
- development of standardised, reliable techniques for diagnosing, and effective,
inexpensive (and preferably) one-dose drugs for treating amoebiasis and
giardiasis;
- more community-based studies for better understanding of the transmission and clinical
patterns of amoebiasis and giardiasis; the relationship between parasites and other
intestinal pathogens; the effect of nutritional status on intestinal infections; and the
natural course of Entamoeba histolytica and Giardia lamblia infections;
- further studies on pathogenesis, especially those related to different parasite strains
and zymodemes and to the immunological responses of the host, including the role of the
immune complexes.
Promoting research activities requires:
- identification of workers and institutions, especially in developing countries, with an
interest and ability to carry out research;
- strengthening of those institutions by providing adequate professional training in
parasitology, equipment, materials and scientific information;
- inclusion, where possible, of aspects of parasite-related diarrhoea in clinical and
field studies, bearing in mind that intestinal parasitoses may be closely linked with
bacterial and viral infections as well as with the immune and nutritional status of the
host;
- addition of Cryptosporidiosis to the list of priorities, as evidence for the
importance of this parasite has increased greatly in the last few years.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 27 December 1986
 3 Page 4 5 3 Page 4 5
Cryptosporidia
Leonardo Mata outlines current understanding of
Cryptosporidia as a cause of diarrhoea. Cryptosporidia were first discovered in mice at the beginning of this century and later
in various species of mammals, birds, reptiles and fish. The importance of these tiny
parasites in humans was recognised in the early 1970s when patients with immunosuppression
or immunodeficiency were seen to become very ill with cryptosporidium diarrhoea, and many
died. Recent experience of acquired immunodeficiency syndrome (AIDS) has shown the
parasite to be an important 'opportunist' agent, able to cause chronic, emaciating and
fatal diarrhoea. Cryptosporidia as a cause of diarrhoea Cryptosporidia can also infect healthy small children, and sometimes adults with normal
immune systems. This was shown in Australia where the parasite was found in about seven
per cent of children with diarrhoeal disease. There have been similar findings among rural
and urban children in Costa Rica. Cryptosporidia causes self-limiting, watery diarrhoea.
Weight loss is likely and, if oral rehydration therapy (ORT) and proper feeding are not
promptly established, dehydration and malnutrition will result. Although recurrence has
been observed, the role of cryptosporidia in persistent diarrhoea is not yet clear.
Cryptosporidia diarrhoea is not, however, as severe or as important as bacterial and viral
diarrhoeas. Incidence and severity Cryptosporidia have a high pathogenicity, and are almost always found in association
with diarrhoea and only rarely when there is no diarrhoea. Studies show its presence in
about 4 to 10 per cent of diarrhoea cases in many parts of the world, usually without
other pathogens being present. It seems to cause more diarrhoea than other parasites,
although giardia and E. histolytica may produce more serious disease. Life cycle, epidemiology and transmission Infection can spread between man and animals, and accidental infection of humans
handling animals has been documented. However, the method of transmission is not clear.
Animals, particularly calves, may be involved in rural areas, but in large urban centres
other explanations must be found. Infection may occur throughout the year in tropical
countries, but a marked seasonality has been observed in Costa Rica and Bangladesh with a
peak of transmission in the warmer wetter months. In developed countries, infections seem
more common in the summer. Exclusively breastfed infants are rarely infected, suggesting
that breastfeeding has a protective effect. Diagnosis and treatment Cryptosporidia can readily be detected by finding the parasite cysts in the stools.
Technicians can easily learn to recognise them under a microscope. Staining is recommended
to avoid confusion with similar organisms. One popular technique is the modified
Ziehl-Neelsen "in cold" or Kinyoun, which can be performed in any laboratory,
requires simple reagents, and provides an accurate and rapid diagnosis. The cysts appear
as ovoid (egg shaped) structures of uniform size and stained bright red. ORT, or
intravenous fluid for very severe cases, is effective in correcting dehydration. Children
should continue normal or extra feeding as soon as any anorexia and dehydration are
corrected, usually a few hours after starting rehydration. No drugs have been found to be
effective against the infection. Prevention Although not enough is known about transmission, the basic concepts of sanitation and
personal hygiene should be observed to prevent infection: handwashing; drinking clean
water; avoiding touching faeces; safe disposal of faeces; and clean careful handling of
food. Dr Leonardo Mata, Director and Professor, Instituto de Investigaciones en Salud
(INISA), Universidad de Costa Rica, Central America. Trichuriasis
Donald Bundy describes the relationship between whipworm
and diarrhoea in one community in the Caribbean. In many communities, at least one in four people may be infected with worms -- and will
continue to be reinfected throughout their lives. The most commonly recognised worm is the
large round worm (Ascaris), although the smaller whipworm (Trichuris) is in many areas
actually more prevalent. Worm infections are less frequently considered to be a factor in
diarrhoea than bacteria or viruses. One recent study in the Caribbean, however, suggests
there may be a need to reappraise this view. Incidence and illness
|
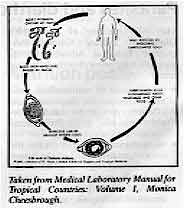
Taken from Medical Laboratory Manual for Tropical
Countries: Volume 1, Monica Cheesbrough Serious disease due to whipworm only occurs in a minority of cases where large numbers
of whipworms are present. In these cases symptoms may include diarrhoea containing blood
and mucus. The bloody diarrhoea may continue over a long period and result in the lower
end of the bowel being pushed out of the anus (a condition known as rectal
prolapse). Such
children may also lose weight, fail to grow and suffer from anaemia.
|
 |
Recent studies at the University of the West Indies have shown that this severe
condition is associated with the presence of between 500 and 1,000 worms in the gut. (1) In heavy infections the surface of the large bowel, to which the whipworms are
attached, becomes swollen and inflamed. It is thought that this inflammation (known as
colitis) causes the bloody diarrhoea, and that it is the long term effect of repeated
bouts of this diarrhoea which causes growth retardation. With light infections there may
be no symptoms or only mild illness. A study in one village showed that children with significant numbers of whipworm tended
to suffer from bloody diarrhoea and growth retardation, not those with large numbers of
roundworms. The study also suggested that the effect of this protracted bloody diarrhoea
on child health and growth very often goes unnoticed and children may not be brought to
clinics for treatment.
Treatment Whipworm infections are very easy to treat using drugs such as albendazole and
mebendazole, although not, unfortunately, with the more commonly used worm treatments.
Controlling worms in the community is more difficult than treating individuals, however,
and little progress is likely to be made until the extent to which trichuris is a problem
in different communities has been established through further studies. Dr Donald A P Bundy, Parasite Epidemiology Research Group, Department of Pure and
Applied Biology, Imperial College, Prince Consort Road, London SW7 2BB. 1. Bundy D A P, 1986. Epidemiological aspects of Trichuris and trichuriasis
in Caribbean communities. Transactions of the Royal Society of Tropical Medicine and
Hygiene, 80, 706-718.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 27 December 1986
 4 Page 5 6 4 Page 5 6
Strongyloides
The role of Strongyloides in causing ill health and, in particular, diarrhoea is
not always clear. Dick Ashford reviews some recent findings
about the parasite. The role of intestinal worm infections as a cause of ill health should neither be
over-estimated nor ignored. For example, in Papua New Guinea, a new species of Strongyloides
sp. infection was found to be a major contributing factor to infant deaths in one
isolated community. Much still remains to be learned about the importance of intestinal
helminths and Strongyloides stercoralis is one of the least understood, although it
is a common infection among children in the tropics, especially in warm, humid regions. Life cycle in the intestine The adult female lives in the small intestine where it burrows, and lays eggs. After
the eggs hatch, the larvae enter the faeces where they can become infective in as little
as 24 hours. The larvae may also become infective before reaching the anus and penetrate
the large bowel wall or skin round the anus (autoinfection). The role of Strongyloides as a cause of diarrhoea is not always clear. In the small
intestine the parasite causes malabsorption which results in offensive, but not
necessarily liquid stools. Infection with S. stercoralis may start with
frequent, pale, loose stools. This lasts about six weeks and there may be some pain or
discomfort. Following this phase, the body's immune processes limit the parasite numbers
but allow the infection to persist indefinitely with minimal symptoms. The interaction
between Strongyloides infection and other causes of diarrhoea is not clear; it is possible
that the worms create conditions which facilitate other infections. Incidence The common Strongyloides stercoralis is not specifically an infant infection; a
recent survey in Kenya showed a rise in prevalence with age, reaching a plateau around six
years of age, very like hookworm. But the little known Strongyloides fuelleborni infection
in the forested parts of Africa, and the newly discovered infection in Papua New Guinea
(PNG) are essentially parasites of the very young.
|
Peak incidence of parasite infection in PNG is found in young
children.
In the heavily infected parts of PNG, the peak incidence is around four years of age,
the highest worm loads occur at 12 months, and mortality is greatest around two months of
age. The disease in PNG is characterised by peripheral oedema, a swollen belly and
respiratory distress, as well as diarrhoea.
|
 |
It has not yet been recognised in Africa, but could easily have been missed in such
young infants, and should be looked for. Diagnosis and treatment Effective drugs are available to treat Strongyloides infection. Although larvae of
other parasites may be present, heavy infection with Strongyloides can usually be detected
in a direct fresh stool smear. With the exception of heavily infected communities, it
would be unrealistic to try to specifically control Strongyloides infection. The lifecycle
is sufficiently similar to that of hookworm for most measures, such as the improvement of
sanitation, to affect both infections. In the many areas where people are living in poor
conditions, the use of thiabendazole or albendazole will eliminate not only hookworm but
also Strongyloides. Dr R W Ashford, Department of Parasitology, Liverpool School of Tropical Medicine,
Pembroke Place, Liverpool L3 5QA, UK.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 27 December 1986
 5 Page 6 7 5 Page 6 7
Giardiasis
John Ackers and Andrew Tomkins
discuss amoebiasis and giardiasis as causes of diarrhoea. Giardia intestinalis is a protozoan parasite that sometimes causes acute and persistent
diarrhoea in many parts of the world, especially among infants and young children. It may
also contribute to malnutrition. Modes of action The parasite is usually swallowed in the inactive cyst form and then changes into the
active trophozoite as it enters the duodenum which it colonises. Trophozoites stick to the
gut wall and may damage or destroy the enterocytes immediately under the parasite. Epidemiology Giardia is most commonly found among older infants and young children in developing
countries - in some population surveys, up to 50 per cent of subjects may be asymptomatic
carriers of giardia. There are protective factors in breastmilk, and giardia is rarely
found in infants less than four months of age. A first infection with giardia, often in later infancy and early childhood, can cause
diarrhoea of varying severity. If left untreated, symptoms improve spontaneously but many
individuals become 'asymptomatic cyst passers'. Among adults without previous immunity,
the first infection can produce severe diarrhoea. Furthermore, when immunity breaks down,
as may occur in severe malnutrition, the parasites multiply unchecked and may cause
serious damage to the lining of the gut. Clinical features
|
Shortening of the villi and increased numbers of inflammatory
cells causing malabsorption in giardiasis.
Initial symptoms include watery diarrhoea, nausea, abdominal pain and flatulence. These
often progress to persistent diarrhoea (more than fourteen days duration) with
'malabsorption' stools. There may be considerable abdominal distension and unpleasant 'bad
egg taste' in the mouth. Some of the symptoms are due to secondary lactase deficiency from
intestinal damage. Fever or the passage of mucus and/or blood are rare. Weight loss or
growth faltering, vitamin A and folate deficiency can occur - as a result of a combination
of decreased nutrient intake and malabsorption.
|
 |
Diagnosis Microscopic examination of a portion of moist stool mixed with saline on a glass slide
will often reveal the characteristic cysts or trophozoites (active forms). A negative
stool test does not exclude the existence of giardia infection since the parasites may be
passed only intermittently. Giardia are also visible on jejunal biopsy specimens. Recently
an ELBA test has been developed for detection of giardia antigens in faeces. Prevention Giardia is transmitted in water supplies and food. Faecal contamination of municipal
water supplies has been responsible for epidemics throughout the world. Contaminated food
sources, especially vegetables which are grown or sold in areas where hygiene is poor, are
also important. The outbreaks of giardia infection in nurseries and day care centres
suggests that person-to-person transmission also occurs. Treatment There are several effective drugs but repeated courses of treatment may be necessary
(see table) because reinfection is common. Nevertheless treatment is still beneficial
where giardia occurs in children or adults with persistent diarrhoea, children with severe
protein energy malnutrition, and adults or children with acute giardiasis in epidemic
form.
| Drug |
Children |
Adults |
Comments |
| Metronidazole |
20mgm/kg/day divided into 4 doses per day for 5 days (max
800mgm) |
400mgm 3 times a day for 5 days or 2g daily for 3 days |
Syrup is available (200mgm/5mls) but often expensive and has
short shelf-life. Tablets can be crushed but bitter taste - needs sweetener to encourage
child to take. Large doses cause nausea and dizziness in some individuals. |
| Tinidazole |
20mgm/kg/day as single dose, for 3 days |
2g daily for 3 days |
Syrup is not available. Nausea and dizziness less prevalent
than with metronidazole but still a problem in some children. |
| N. B. Metronidazole is only a "type" drug for
numerous nitroimidazoles, including for example tinidazole, ornidazole, secnidazole and
nimorazole. These last four have shorter treatment courses than
metronidazole. |
Dr Andrew Tomkins, Departments of Clinical Tropical Medicine and
Human Nutrition, London School of Hygiene and Tropical Medicine, Keppel Street, London
WC1E 7HT. Tomkins, A. M. Intestinal Parasites: Part 1. Nutritional Importance. pp. 61-67 In:
Diarrhoea and Malnutrition in Childhood (1986), eds. Walker-Smith and McNeish,
Butterworths.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 27 December 1986
 6 Page 7 8 6 Page 7 8
Amoebiasis
Amoebiasis means being infected with the protozoan parasite, Entamoeba histolytica, an
amoeba with a simple life cycle. Infection starts by swallowing the amoebic cyst, which
hatches out in the small intestine and divides to produce trophozoites or feeding stages.
These pass into the large intestine where they feed (mainly on starch and bacteria) and
multiply. Amoebae are shed in the faeces either as trophozoites during diarrhoea or in the
cyst form. E. histolytica as a cause of diarrhoea Although amoebiasis is very common, the vast majority of infected persons are entirely
free of symptoms. In these cases, the amoeba seems to live a completely commensal life
within the gut. Problems arise when E. histolytica attacks the gut wall - a condition
known as invasive amoebiasis, thought to affect 48 million people annually. After invading
it, the parasites may remain in the bowel wall causing intestinal amoebiasis, spread to
the liver causing amoebic liver abscess or, more rarely affect other parts of the body.
Only intestinal amoebiasis causes dysentery. In typical amoebic dysentery, blood-stained
stools containing mucus are passed each day or bloody diarrhoea occurs, with some colicky
pain but no fever and patients do not feel particularly ill. In contrast, fulminating amoebic colitis is an extremely severe clinical condition with
sudden onset, swinging fever, chills, sweating and very severe diarrhoea, dehydration and
prostration. Stools are liquid with varying amounts of blood and mucus. Severe intestinal
haemorrhages or perforation followed by peritonitis may occur. The mortality in untreated
cases is high. Epidemiology It is still not clear whether all types of E. histolytica have the potential to
cause invasive disease, or whether specific invasive strains exist. Although many experts
still regard invasive amoebiasis as a consequence of the failure of mechanisms (either of
host immunity or related to diet or gut flora) which normally keep the parasite in check,
more recent evidence (particularly from isoenzyme studies) suggests that both invasive and
non-invasive strains occur. The subject however, is still under intensive investigation. The incidence of invasive amoebiasis varies greatly in different parts of the world, as
does the ratio of cases of invasive disease to asymptomatic cyst shedding. The infection
is considerably more common in tropical and developing countries but the organism is
present in all countries, and male homosexuals throughout the world represent a newly
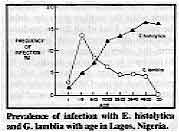
recognised group with very high levels of asymptomatic infection. Unlike infections with Giardia
lamblia, no effective immunity develops even after repeated infections (see below) and
the highest prevalence of infection is found in adults. It is not clear how much of
diarrhoea (and particularly childhood diarrhoea) in the tropics is due to E.
histolytica. Transmission and prevention
|
Prevalence of infection with E. histolytica and G.
lamblia with age in Lagos, Nigeria. Adapted by R Guerrant and J Ravdin in Reviews of Infectious Diseases from J P
Oyerinde et al in International Journal of Epidemiology.
|
 |
Infection invariably occurs by swallowing cysts, and there is both person-to-person and
waterborne transmission. A considerably higher concentration of chlorine is required to
kill cysts than faecal bacteria. Water may be rendered safe by boiling, pasteurisation (at
above 50° C), and by treatment with 3 ppm (parts per million) of iodine or hypochlorite,
or by sand-bed filtration. If they dry out, cysts in soil or faecal material are
immediately killed. If kept damp, they may survive for several weeks, depending on the
temperature. Vegetables to be eaten raw should be steeped in vinegar or dilute
hypochlorite solution for 30 minutes, followed by rinsing in boiled water. Diagnosis Diagnosis of infection is made by detecting the organisms in the faeces using a
microscope. In asymptomatic infected patients the cysts should be sought in faecal
concentrate after staining with iodine. Training and practice are needed to accurately
distinguish cysts of E. histolytica from other protozoa.
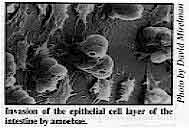 |
Invasion of the epithelial cell layer of the intestine by amoebae. In all cases, a fresh (preferably warm) specimen should also be examined without
concentration or the addition of iodine in order to detect live trophozoites (feeding
stages).
|
These may be found, either in an asymptomatic infected patient where some other
bacterial or viral diarrhoea is causing trophozoites to be shed before they have had time
to form cysts; or in cases of invasive intestinal amoebiasis. In the latter, the parasites
will be large, motile (but only if still warm) and contain red blood cells. Trophozoites
containing red blood cells may also be found by rectal biopsy and are diagnostic for the
intestinal disease. Treatment The treatment of choice for invasive amoebiasis is now one of the 5-nitroimidazole
drugs (or diloxanide or chloroquine). Whether completely asymptomatic cyst passers should
be treated is still controversial. If such amoebae are fundamentally incapable of
invasion, then there is not justification for doing so, but some people do not yet accept
that most isolates of E. histolytica are inherently harmless. On the other hand, in
situations where rapid reinfection is probably unavoidable, the treatment of asymptomatic
persons is widely regarded as a waste of scarce resources. J P Ackers, Department of Medical Protozoology, London School of Hygiene and
Tropical Medicine, Keppel Street, London WC1E 7HT, UK.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 27 December 1986
 7 Page 8 7 Page 8
Fighting incorrect beliefs I have been working in general practice for two years, and I have experienced very good
results when using ORT. I find it easy to use, economical and it avoids the hazards of
dehydration. I have also tried honey in water, which seemed to work very well, and was
accepted well by children. I have often found it difficult to convince people that ORT
does work, they expect instant results and expensive medicines, which are often useless.
Many doctors advise mothers to stop breastfeeding and feeding during diarrhoea, which I
think is very wrong. I have experienced many problems in going against the beliefs of a
majority of doctors, as I am only a junior practitioner, but I have full confidence and
faith in ORT, so please send me your DD regularly. Dr Subhash B Gawari, 1393 Ghodnadi, Pune, Maharashtra State, 412 210, India.
More on vitamin A You are right to point out in DD 24 that oral
vitamin A should be used for prevention and treatment of those at risk of blindness due to
malnutrition. In high risk areas all children with severe diarrhoea should be given
200,000 IU vitamin A orally when first seen, unless they have been given a comparable dose
of vitamin A recently. All children should have their eyes checked, remembering that even
breastfed children are at risk if the mother is herself severely malnourished, has little
milk or weaning has been delayed. Oral vitamin A has been shown in a controlled trial in Indonesia to give results
similar to injectable vitamin A. It is unlikely that injectable vitamin A will be
available extensively in the areas where the need is greatest, and oral vitamin A anyway
works very well without all the other problems associated with injections. The dose must
be high though, and this is not mentioned in your update note. At least 200,000 IU should
be given; a further 200,000 IU may be given the next day and again after seven days if
there is severe corneal damage. Give half doses for very young children, under one year. Nicholas Cohen MD, Department of Community Medicine and Epidemiology, The University
of Nottingham Medical School, Queen's Medical Centre, Nottingham NG7 2UH, UK.
ORT in Turkey The use of ORT and importance of breastfeeding are stressed to all mothers who visit
the Gulveren Health Centre, near Ankara. Every health centre should have a diarrhoea unit
for teaching parents and treating children with diarrhoea. Diarrhoea units do not need
much equipment; a simple room, a few chairs, some cups and glasses and posters about
diarrhoea and ORT are sufficient. Every parent whose child has diarrhoea, whether
dehydrated or not, should be taught about diarrhoea and ORT, and shown how to prepare ORS.
The doctor and nurse should watch while the mother gives the child the solution. First of
all this procedure separates the patient with diarrhoea from the other patients, and
mothers do not have to wait to see the doctor. It is also important not just to tell a
mother how to use ORT and about the hazards of diarrhoea and then send her home as you
will not know whether she actually gives the solution. We also show mothers that children
with nausea and vomiting can be given ORS. Mothers are also visited at home to check the
condition of the children and continue education. The unit was established in June 1986
and in one month, 300 diarrhoea patients were admitted. No problems with taking ORS with
vomiting were seen. Educating parents is not enough. You should show them how to prepare ORS, watch while
they are giving the solution to the child and call them back to the unit or visit them at
home the next day. And the most important thing about ORT is that all the doctors and
medical staff believe that it works. Dr Atilla Buyukgebiz, Director of Gulveren Health Centre, Ankara, Turkey.
DD mailing list
- Funds for free distribution of DD are limited. We would like the newsletter to
continue to reach those readers who find it useful. Please write to us or fill in and
return the form below if you no longer wish to receive DD.
- Readers in North America, Western Europe, Australia and New Zealand are asked to pay an
annual subscription to DD (US$10.00 or £5.00 sterling). If you have not already
paid, please send a cheque or international money order payable to AHRTAG (DD) together
with your completed form.
- The DD mailing list is currently being updated. If we do not have your correct mailing
address please complete the form and return to AHRTAG at 85 Marylebone High Street, London
W1M 3DE, U. K.
|
Name . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Address . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . .
Subscription No. . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . .
Readers in North
America, Western Europe, Australia and New Zealand only:
I enclose payment for one year's subscription to DD
[ ]
I no longer wish to receive DD [ ] |
In the next issue . . . DD 28 will focus on home solutions for preventing
dehydration and ORS for preventing dehydration.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Editor Kathy Attawell
Editorial assistant Maria Spyrou Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), ODA (UK), UNICEF, WHO and GTZ
|
Issue no. 27 December 1986
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
updated: 23 August, 2019
|