|
| |
Issue no. 49 - June 1992
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 49 - June
1992
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 49 June 1992
 Page 1 2
Page 1 2
The child and its environment
Child health begins at conception. It is influenced by the health of the mother as the
foetus grows within the micro-environment of her belly.
|
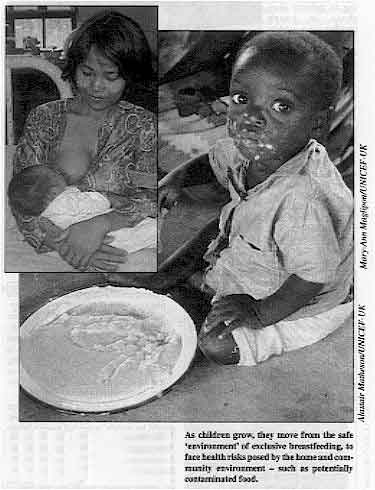
As children grow, they move from the safe 'environment' of
exclusive breastfeeding, to face health risks posed by the home and community environment
- such as potentially contaminated food.
After birth, the newborn infant's environment expands to include its immediate family
circumstances. Central to these is its mother - breastfeeding by the mother protects and
nourishes the newborn with, first, colostrum, and then breastmilk. An infant should
consume nothing else during the first four to six months of life. Exclusive breastfeeding
(see="#page2">pages 2-3) plays an important role in providing a safe
'environment' for young babies.
|
 |
Hygienic disposal of waste Health risks increase when the child starts to eat other foods, and to move around
inside and outside the home. There is a greater chance that the child will consume
contaminated food and water. This happens especially where standards of hygiene are low as
a result of insufficient resources or education. Essential to a safe domestic environment is the hygienic disposal of domestic water and
human waste. This is considered in the article on="#page6">page 6, which looks
at the construction of local sewerage systems. Other practical aspects of water supply and
sanitation in low income areas have been covered in DD31. As this issue of DD goes to press, strategies for protecting the global
environment have been discussed at the Earth Summit conference in Rio de Janeiro, Brazil.
At the other end of the scale, it is important to remember that much can be done to
protect immediate local environment of the child - in the womb, at the breast, in the home
and in the community - which largely determines its health now and in the future.
|
In this issue:
- Exclusive breastfeeding
- Diarrhoea and low birthweight
- Cholera guidelines
- Low cost sewerage
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 49 June 1992
 1 Page 2 3 1 Page 2 3
| Breast is best... but breast alone is best of all |
Exclusive breastfeeding
The value of exclusive breastfeeding in the first four to six months of life is
being increasingly recognised.
|
Breast is best - giving extra fluids is unnecessary - a mother
in the Philippines breastfeeding her day-old baby.
The importance of breastfeeding in helping to prevent diarrhoea in young children is
now widely accepted. There is growing evidence that the risk of death and illness from
diarrhoeal infections increases sharply when supplements are given in addition to
breastmilk. Most infants in Africa, Asia and Latin America are breastfed in the first few months of
life. But many mothers (as well as doctors and other health workers) wrongly believe that
infants under four months old need other liquids in addition to breastmilk, especially in
hot climates.
|
 |
In Peru and Brazil, for example, most infants receive herbal teas or water in their
first month of life. In Senegal, West Africa, only 5 per cent of infants under five months
old are exclusively breastfed, with over two thirds receiving supplementary water (1). Dangers of extra drinks Giving extra liquids is not only unnecessary, but may also be harmful because:
- The baby may spend less time breastfeeding, which means that the mother's breasts are
less stimulated to produce breastmilk. A Brazilian study showed that breastfed infants,
who received teas or water in the first days of life, did not breastfeed for as long as
those who were exclusively breastfed during their first week (2).
- The extra fluids may be made with unsafe water and given in feeding bottles which are
contaminated. In Peru, babies who received water and teas in addition to breastmilk had
twice as many days with diarrhoea in any given month as those receiving only breastmilk (3). These findings were confirmed by recent research from the Philippines (4). Another Brazilian study showed that each additional daily 'feed' with
teas or water was associated with a 40 per cent increase in diarrhoea mortality. An infant
receiving three feedings of extra fluids a day was almost three times more likely to die
than an exclusively breastfed infant'.
The message that breast is best, and that giving additional fluids is unnecessary,
should be widely promoted among health workers, as well as the wider community. Professor Cesar Victora, Centro de Pesquisas Epidemiologicas, Universidade Federal
de Pelotas, Pelotas, RS, Brazil. 1. Dr Jean Claude Lowe, Ministry of Public Health, Cameroon. 1991.
Health worker attitudes towards breastfeeding.
2. Martines, J C, 1985. The interrelations between feeding mode,
malnutrition and diarrhoea morbidity in early infancy among the urban poor in Southern
Brazil. PhD dissertation, University of London.
3. Brown, K H, et al., 1989. Infant feeding practices and their
relationship with diarrhoeal and other diseases in Huascar (Lima), Peru. J.
Ped. 83:
31-40.
4. Popkin, B M et al., 1990. Breastfeeding and diarrhoeal mortality
J. Ped. 86: 874-82.
5. Victora, C G et al., 1987. Evidence for a strong protection of
breastfeeding against infant deaths from infectious diseases in Brazil. Lancet 2: 319-22.
|
What is exclusive breastfeeding? In order to measure breastfeeding practices, including exclusive breastfeeding, in a
standard way, definitions have been agreed. Exclusive breastfeeding is when an infant
receives only breastmilk from his or her mother (or a wet-nurse, or expressed breastmilk),
and no other liquids or solids. The following are key to establishing 'exclusive breastfeeding':
- starting to breastfeed within an hour after birth - this ensures that the infant
receives colostrum (thicker, yellowish milk produced during the first few days after
delivery) as well as breastmilk;
- not giving any prelacteal drinks (any drink given before the first breastfeed),
including water, 'holy' or ritually blessed water, sugar or glucose water, herbal teas or
other fluids before the first breastfeed;
- breastfeeding frequently, day and night;
- not giving any other food or fluids such as water or infant formula during the first
four to six months (until food is introduced between four and six months in addition to
breastmilk).
Note: An exclusively breastfed child under six months old who develops diarrhoea needs
extra fluids to prevent dehydration. WHO recommends that this be oral rehydration solution
or clean water, in addition to frequent breastfeeding. Fluids that contain nutrients, such
as rice water, gruel, etc, are not recommended. If possible, the infant should be seen by
a health worker who is trained to give ORS solution. As soon as the diarrhoea stops,
exclusive breastfeeding should be resumed.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 49 June 1992
 2 Page 3 4 2 Page 3 4
| Breast is best... but breast alone is best of all |
Extra drinks are unnecessary
Mothers and health workers often believe that healthy infants need fluid
supplements. Stina Almroth explains why extra drinks can do more
harm than good. Families and health workers give extra drinks to breastfed babies for many reasons.
Sugar water is often given to prevent or treat constipation. Water is usually given in the
belief that it is needed when the weather is hot. Some people believe that too frequent
breastfeeding should be avoided and that it is good to give the baby something else, like
water, in between breastfeeds. Herbal teas are sometimes given to prevent or treat a
variety of ailments. These beliefs may be understandable, but several studies have shown that extra fluids
are not actually needed by healthy infants during the first half year if they are
exclusively breastfed. Breastmilk does not make an infant constipated. Provided that a baby is breastfed frequently to ensure that it gets enough milk, extra
drinks are not necessary. People may think that babies, like adults, get thirsty and need
extra water when it is hot. Physiologically this is not necessary (1).
Breastmilk is a food and fluid uniquely balanced for babies, with virtually no excess
minerals and protein. Therefore the amount of waste products that need to be excreted in
the urine is small, requiring very little water. Even where the climate is very hot and dry and there is considerable water lost through
evaporation from the skin and lungs, a healthy exclusively breastfed baby is not in danger
of dehydration. Studies in many hot countries have shown that exclusively breastfed
infants do not need extra fluids (2), (3). The
concentration of solutes in the urine of these infants was well below levels associated
with inadequate fluid intake. Giving babies glucose water during the first few days after birth has been a common
hospital practice. It was thought that this helped to maintain the infant's body weight
until the mother started to produce sufficient milk. A study in Australia has shown that
babies who received only breastmilk lost less weight during the first few days than
infants who received supplements of glucose water(4). Many have assumed that water supplements breastmilk, whereas in fact water replaces
it (5). Naturally, babies grow better on breastmilk, which contains
more than three times as much energy by volume as glucose water. The message to breastfeed exclusively may seem simple, but promoting it effectively
requires carefully designed communication strategies. We must learn what particular extra
fluids are commonly given and why. Then our advice to avoid them can be more specific and
more effective. Stina Almroth, Selmedalsringen 8, 126 70 Hagersten, Sweden. 1. Almroth, S G, 1978. Water requirements of breastfed infants in a
hot climate. Am. J. Clin. Nutr, 31: 1154-57.
2. Almroth, S G and Bidinger P D, 1990. No need for water
supplementation in exclusively breastfed infants under hot and arid conditions. Trans. R.
Soc. Trop. Med. and Hygiene 84: 602-604.
3. WHO/CDD, 1991. Breastfeeding and the use of water and teas. CDD
Update no 9, August.
4. Glover, J and Sandilands, M, 1990. Supplementation of
breastfeeding infants and weight loss in hospital. J. Human Lactation 6:163-166.
5. Sachdev: HP S, et al., 1991. Water supplementation in
exclusively breastfed infants during summer in the tropics. Lancet 337:929-933.
|
Health workers: beliefs versus advice Most health workers believe in the benefits of breastfeeding. But few actually
recommend breastfeeding within an hour of birth, and few actually help mothers to
establish and practise breastfeeding. This means that infants risk infections from other
possibly contaminated fluids, and do not have the immediate post-partum protection
provided by breastfeeding and colostrum.
|
Health workers play a crucial role in helping mothers to
establish and practise breastfeeding.
Advice about giving prelacteal feeds, separation of mother and newborn, and delaying
breastfeeding until 24 hours after delivery, are still very common.
- In Senegal's capital city, Dakar, although more than 80 per cent of health
workers questioned believed that colostrum should be given to infants, only a quarter
recommended that breastfeeding begin within two hours of birth. One third recommended that
the mother wait as long as 24 hours. Sugar water, and 'holy water' were often given to
infants before their first breastfeed.
|
 |
- In Kumasi, Ghana, although all of 100 medically qualified midwives asked about
infant feeding and giving water supplements (1) believed breastfeeding
to be the best method of infant feeding, 75 per cent of them advised giving sugar and
water or water alone before the first breastfeed.
Reasons given included: 'to prevent hypoglycaemia' (low blood sugar levels), 'to check
the swallowing reflex', or 'to maintain a correct fluid balance'. Only a few said that
infants did not need water at any time during the first few months. Most thought that
water should be given to all infants on the first day of life, usually within six hours of
birth.
A common belief is that the tongue must be cleansed with water after breastfeeding, to
prevent oral thrush and that although breastmilk provides an infant with energy, water is
essential for life.
1. Mackie, E, 1991. Water supplementation of breastfed infants in
Ghana. Letter in The Lancet, vol 338: 251.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 49 June 1992
 3 Page 4 5 3 Page 4 5
Low birth weight babies Children born with low birth weight are at high risk of malnutrition and frequent
diarrhoea infections. DD explains why, and how to care for them. Some 22 million low birth weight (LBW) babies are born in the world each year, most of
them in less developed countries. These babies weigh under 2,500g at birth, rarely catch
up in growth, and are likely to remain malnourished at least during their first four years
of life (1). Low birth weight babies are more vulnerable to a range of
infections, including acute respiratory infections and diarrhoeal diseases. A study in Brazil (2) found that LBW infants are twice as likely to
die from diarrhoea as babies weighing 2,500g or more at birth. Malnourished and well
nourished children can have equal numbers of diarrhoeal episodes, but in less well
nourished children these are more severe or prolonged.
|
If the baby cannot suck, it should be given expressed breastmilk. Children of low weight, due to LBW or malnutrition, are also at higher risk of becoming
dehydrated during a diarrhoea episode than children who weigh more. One possible
explanation for this increased severity has been identified (3).
Infections in the proportionally greater intestinal surface area of small infants and
children result in larger stool losses per kilogram of body weight.
|
 |
- LBW babies should be exclusively breastfed during the first four to six months of life.
Breastfeeding should also be continued well into the child's second year, as it protects
from diarrhoea and other infections. This requires special efforts from health workers, as
these babies are often weaned early (4).
- Not all LBW babies can breastfeed. For very LBW babies (less than 1,500g) who are unable
to suck, expressed breastmilk should be provided with a nasogastric tube or a cup and
spoon.
- LBW babies with diarrhoea must be given oral rehydration therapy as soon as possible, as
they can easily become dehydrated.
- Parents should seek medical care quickly if a LBW baby with diarrhoea shows any of the
following signs: starts to pass many loose or watery stools; has repeated vomiting;
becomes very thirsty; is sucking / nursing, eating or drinking poorly; develops a fever;
has blood in the stool; or does not get better within three days.
Drs Fernando C Barros and Cesar Victora, Department of Social Medicine, Universidade
Federal de Pelotas, Brazil, and Dr José C Martines, Diarrhoeal Diseases Control
Programme, WHO, Geneva, Switzerland. 1. Barros, F C, et al., 1992. Determinants and consequences of
prematurity and intrauterine growth retardation: a longitudinal study in Southern Brazil.
Paediatrics (in press).
2. Victora, C G, et al., 1988. Influence of birth weight on
mortality from infectious diseases: a case-control study. Paediatrics 81: 807-811.
3. Victora, C G, et al., in press. Small body size as a simple
indicator of the risk of dehydration among young children with diarrhoea.
4. Barros, F C, et al., 1986. Birth weight and duration of
breastfeeding: are the beneficial effects of human milk being over-estimated? Paediatrics
78: 656-61.
|
Home treatment for infants with diarrhoea Specific guidelines according to the infant's age and feeding status are: 1. If the infant is less than four to six months old and normally takes
breastmilk alone, or with supplements of water or tea advise the mother to:
- continue to breastfeed as frequently and for as long as the infant wants;
- give ORS solution, or if this is not possible, give plain water, 50-l00mI after each
loose stool; tea is not recommended.
2. If the infant is less than four to six months of age and normally takes
animal milk or formula, with or without breastmilk, advise the mother to:
- continue to breastfeed as frequently and for as long as the infant wants;
- give the usual animal milk or formula, undiluted,
- give ORS solution or plain water.
3. If the infant is taking soft weaning foods, in addition to animal or formula
milk and / or breastmilk, advise the mother to:
- continue to breastfeed as frequently and for as long as the infant wants;
- give the usual animal milk or formula, undiluted;
- give additional fluids such as ORS solution, rice water, yogurt drink, or plain water;
50-100ml after each loose stool;
- give the normal diet of soft nutritious weaning foods; if the child is over six months
of age and not yet taking soft foods, these should start to be given.
Guidelines that apply to all infants, regardless of their age and feeding
status:
- If it is not possible to give measured amounts of recommended fluids after each stool,
advise the mother to give the child more fluid than usual, as much as the child will take.
- Special lactose-free or hydrolysed protein formulas should not be used routinely in
place of the usual animal milk or formula; they are rarely required.
- Use a clean cup or spoon to give fluids to infants - not feeding bottles which axe a
source of infection.
All mothers should be taught to bring an infant with diarrhoea for treatment by a
health worker, if it does not get better in three days or develops any of the following:
many watery stools; repeated vomiting; marked thirst; eating or drinking poorly; fever;
blood in the stool.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 49 June 1992
 4 Page 5 6 4 Page 5 6
Facing up to the threat
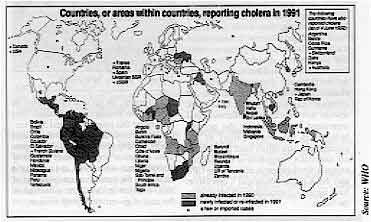
DD provides guidelines for prevention and treatment. In 1991, for the first time this century, cholera broke out in Latin America. It has
been endemic in Africa since 1970. Now nearly half of the continent's 52 countries have
reported cases. Cholera is also endemic in Asia and parts of the Middle East. Isolated
cases have been identified in the USA and eastern Europe.
 |
Cholera is treatable and preventable. In some countries only 1 per cent of all people
with the disease have died, while in others the death rate has been much higher. Efforts
to train health workers in early detection of cases and effective treatment, and to
educate the public, are essential in every country at risk. |
How to recognise cholera Most cholera infections cause only mild symptoms, and the illness resembles other types
of watery diarrhoea. The severe form of the disease occurs in only about 5 per cent of
infected persons. The signs of cholera are: frequent vomiting; large amounts of very watery diarrhoea
which is straw-coloured and contains little faecal matter (known as 'rice-water'
diarrhoea); and rapidly developing signs of severe dehydration due to the loss of large
amounts of liquid stool fluid (up to 25 per cent of body weight in a day). These signs are usually all that is needed to diagnose cholera, especially in children
older than five years and adults. Precise laboratory diagnosis is not necessary to
determine the best treatment. How to treat cholera
- If there is severe dehydration, give Ringer's Lactate Solution intravenously: 30ml/kg in
the first 30 minutes, and then 70ml/kg in the next 2½ hours (total IV fluid 100ml/kg).
- Replace ongoing losses of liquid stool with equal amounts of ORS solution by mouth; this
may require 5-10ml of ORS solution per kg body weight each hour. If signs of dehydration
recur, more ORS solution should be given, In patients with very high rates of stool loss,
Ringer's Lactate Solution should be given intravenously until the rate of stool output
diminishes.
- Treat severe cases with an appropriate oral antibiotic, such as tetracycline, when
vomiting has stopped.
Adult dosage:
- 500mg tetracycline four times per day for three days or
- 300mg doxycycline in a single dose or
- 100mg furazolidone four times per day for three days, or
- 160mg trimethoprim and 800mg sulfamethoxazole twice a day for three days.
Child dosage:
- tetracycline 12.5mg/kg four times a day for three days (tetracycline should not be
given to children under 12 years of age) or
- (if local resistance) furazolidone 1.25mg/kg four times a day for three days or
- trimethoprim 5mg/kg and sulfamethoxazole 25mg/kg twice a day for three days.
- For patients with some dehydration, give ORS solution by mouth. During the first four
hours give approximately:
| under 4 months |
200ml to 400ml |
| 4-11 months |
400ml to 600ml |
| 1-4 years |
600ml to 1200ml |
| 5-14 years |
1200ml to 2200ml |
| over 14 years |
2200ml to 4000ml |
- When rehydration is complete and vomiting has stopped (usually 4-6 hours after treatment
is started) encourage the patient to eat and drink - infants should continue to
breastfeed.
Prevention in the home Cholera is spread via the stools of people who are infected with the cholera organism;
faecally contaminated water and food are especially important. The majority who are
symptomless or have only mild diarrhoea can still spread the disease to others through
faecal-oral transmission. Health workers and families can do much to reduce the risk of
infection.
Safe food:
food is contaminated during preparation or storage after cooking, by hands or water
contaminated with cholera germs. Cholera vibrio can survive in food for up to five days.
- Wash hands before preparing food and after using the toilet.
- Cook food thoroughly.
- Eat cooked foods immediately.
- Store cooked foods carefully.
- Reheat cooked foods thoroughly.
- Wash fruits and vegetables with clean water, if they are to be eaten raw.
- Use clean, uncontaminated or boiled or chlorinated water to prepare and cook foods.
Water:
use only clean potable water for drinking or washing food, or water that has been:
- disinfected with alum potash or chlorine;
- boiled (for up to five minutes); or
- collected as rainwater.
Store drinking water in a clean, covered container. To take water out, use a
long-handled dipper that is not used for any other purpose.
Hygiene and waste disposal:
- If possible, wash kitchen dishes with soap, rinse with clean water and only use clean
cloths to wipe dishes dry (if not, leave dishes to dry in the sun).
- Dispose of all excreta and faecally contaminated materials in a latrine or bury them if
latrines are not available.
Sources: WHO, PAHO and ADDR materials. The WHO cholera information pack is available from CDD/WHO, Geneva 27, 1211
Switzerland.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 49 June 1992
 5 Page 6 7 5 Page 6 7
Low cost sewerage
Peter Kolsky describes circumstances where sewerage
systems may be appropriate, and outlines the key issues to consider. Safe disposal of domestic water and human waste plays an important role in the control
of diarrhoeal diseases. Recent issues of DD have highlighted some practical aspects
of water supply and sanitation for low-income and refugee communities. These have focused
in particular on low-cost alternatives to conventional engineering methods for the
disposal of human waste in rural and peri-urban areas. These low-cost alternatives (e. g.
VIP latrines and pour-flush toilets with soakaways) cost much less than conventional
sewerage, are much easier to build, and are easier to manage by individual families. There are, however, some situations where sewers (pipes for removing used domestic
water and human waste) are the most appropriate technology. For example, where water has
been piped into houses in areas of high population density, some form of piped sewerage is
the only way to avoid flooding the area with sewage (the mix of used water and human
wastes). If domestic water use is high, people need a safe way to dispose of sewage. If a
sewerage system does not exist, sewage flooding will spread faecal contamination. In these circumstances, some form of sewer or septic tank will be more appropriate than
latrines or pour-flush toilets. The choice between sewers and septic tanks is usually
based on consideration of population density, soil conditions and cost. Septic tanks Septic tanks are simple systems that let the solids settle out of the waste water and
sewage, before the liquid filters into the soil. Where population density is low, and
where soils can absorb water easily (e. g. sandy soils with a low groundwater level), some
form of septic tank can provide a safe and economic means of sewage disposal. The tank
itself does not treat the sewage, and the water flowing out of it is highly contaminated;
it is the soil into which the contaminated water flows that does the real 'filtering' of
the sewage. If the water coming out of a septic tank system cannot be absorbed by the soil
(and therefore runs along the ground), it becomes a significant environmental health
hazard and a septic tank is not an appropriate sewerage system. Note: septic tanks should not be sited too close to drinking water
supplies and pipes, in case the pipes have breaks in them and drinking water becomes
contaminated by sewage being absorbed by the soil in the surrounding area.
|
Self-managed sanitation The Orangi Pilot Project (OPP) is a non-government organisation working in Pakistan.
Orangi is a large unplanned slum on the edge of the city of Karachi, with a population of
800,000. The OPP has undertaken a number of development projects, but is best known for
its model of low-cost sanitation. The project recognises development on two levels. Internal development consists
of constructing sanitary latrines in the houses, sewerage lines in the lanes, and small
sewerage collectors downstream of the lanes. The project's experience shows that local
people, organised by lanes, can finance, manage, and maintain this internal development. External
development consists of constructing large drains and collectors along main roads,
main trunk sewers downstream of collectors, and treatment works, which the project
believes is the responsibility of the government, and which local people cannot undertake.
Integration of internal and external development is critical - the OPP and the Karachi
Municipal Corporation have signed a contract to work together in the future.
|
The sewer built by local people.
At present, 70 per cent of the lanes in Orangi have underground sewerage lines built
under this programme, and 345 'secondary' drains, downstream of the lane drains, have been
constructed. This represents sanitation improvements for nearly 70,000 homes since 1980;
and a dramatic impact on the immediate environment of slum dwellers in
Orangi, at a
fraction of the cost of government programmes.
|
 |
|
Sewers Sewers are pipe systems that remove sewage from the home and neighbourhood. They should
be considered where water use is high, and septic tanks cannot be used. Even where septic
tanks are technically feasible, sewers may still be a cheaper or better option, depending
upon the housing density, the local experience with sewers and septic tanks, and the
wishes of the community. Conventional sewers,
as first developed in Europe and North America, are expensive; in 1978 (1),
they cost about US$ 400 / household/ year. One of the main reasons they cost so much is
because they are often quite deep, thus requiring a lot of excavation. They are deep for
two reasons:
- the slope of the pipes must be relatively steep, so that the sediment from human waste
moves and does not settle out and block the pipe; and
- pipes must be sufficiently deep (about a meter) to avoid being broken by car and lorry
traffic on the ground above them.
Two different systems have been developed that save money by allowing sewers to be
shallower.
Small bore sewers
use a settling compartment, like a septic tank, outside each house to catch solids before
they flow into the sewer. This means that the sewer pipe itself can be smaller and laid
with a flatter slope, because it carries only the liquid, since solids have already been
deposited in the tank. Such systems are most appropriate where septic tanks have already
been installed. Shallow sewers
are like ordinary sewers in that they carry both the liquid and solid parts of the
sewage. The sewers are shallow because they are built where there is no vehicle traffic.
Shallow sewers are often located in the back yards of houses to avoid traffic, or they may
be placed under streets in communities where traffic is unlikely ever to be very heavy.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 49 June 1992
 6 Page 7 8 6 Page 7 8
|
Women take action Amman Nagar (B) is a low-income community located in an abandoned water reservoir in
Hyderabad, India. Because of the area's inherent drainage problems, recent slum-upgrading
work in this community has included the construction of some large open drains, although
it did not include sewers for each street. Nevertheless, a number of streets have sewers,
funded by the residents themselves, which lead to the open drains.
|
Youssef Bi and her friends, and the sewer that they
arranged to have constructed.
In one of the lanes, the prime mover for this was a woman named Youssef Bi.
|
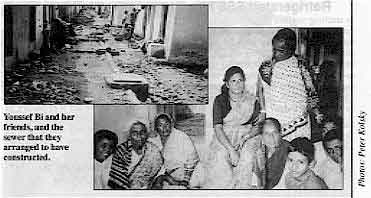 |
Several years ago, her family built a twin-pit sanitation system, which she claims the
municipality was supposed to clean out periodically. The municipality did not do so, but
Youssef Bi did not complain; her family had no title to the land on which they were living
and had no wish to attract attention to themselves. As a result, the toilet failed, and
the system overflowed into the lane. Other houses had similar problems, with the result
that the area was soon flooded with sewage. Youssef Bi went to the local slum improvement
committee (composed entirely of men) and asked them to consider building a sewer to
connect to the open drain. They were more concerned, however, with other problems.
Undeterred, Youssef Bi talked to the women in the other twelve houses of her lane, and
succeeded in obtaining a contribution of 500Rs (US$ 25) from each to build a sewer. She
contributed a little bit more, and then hired a contractor to build the sewer; the job was
done in two days. After their success, the lane on the opposite side of the open drain
followed suit, and now four lanes have built their own sewers. They have had no blockages
in eight months, but anticipate collecting 5Rs per household to cover the cost of
unblocking the sewer, should that problem arise.
|
Community participation At least as important as the development of lower cost technical solutions has been the
evolution of community participation in low-cost sewerage. Traditionally, central
authorities have taken responsibility for entire sewerage networks, on the basis that all
drains up to the individual property boundaries are public property and that maintenance
is best done by a single organisation. In some areas, however, municipal authorities are beginning to think about devolving
responsibility for small 'local sewers to community groups or non-government
organisations. This can be done because the small branches are technically simple, and
because they can be managed more closely by the community than by municipal authorities.
The Orangi Pilot-Project, and the stories of individuals such as Youssef Bi in slums
without organised projects, show the potential for such efforts.
|
Sewerage checklist
1. Where does the waste go?
A sewer for one street can create a problem for the neighbours if it is not planned
properly.
2. Is the system technically feasible?
Some help from the local sewerage board, if they are willing to break with traditional
engineering standards, can save problems. Low-cost sewerage requires significant technical
input from an engineer or technician. It also depends on availability of adequate water
supply, the slope of the ground and the soil not being too rocky.
3. Is the plan socially feasible?
A lot depends on how much the community wants sewerage, and whether it makes sense for
them to manage the construction, as in Orangi, or whether they expect the municipality to
do it. If people choose the community based option, it makes sense to start small and
learn as you go.
4. Does the system fit together?
A little work with levels at the beginning (with the help of trained engineers or
technicians), and some knowledge of the plans of the sewerage board, can help assure that
low-cost sewers from many streets fit together properly. Otherwise, upstream sewers may be
unable to empty into downstream sewers that are too small or at a higher elevation.
5. Is it necessary?
Other technologies (latrines, pour-flush toilets and soakaways) are cheaper, simpler and
easier to implement. Sewers should only be considered where water consumption is high, and
should be weighed carefully against septic tanks or similar soakaway systems, which may be
simpler to organise, and can solve the problem locally. |
Peter Kolsky, London School of Hygiene and Tropical Medicine, Keppel
Street, London WC1E 7HT, UK. 1. Small-bore sewers: Kalbermatten, JM, et al,, 1980. Appropriate
technology for water supply and sanitation. Vol 2, a planner's guide, Washington, D. C;
World Bank. Further reading Septic tanks: Cairncross, S, 1988. Small scale sanitation. Ross Institute
Bulletin No. 8, LSHTM.
Shallow sewers: UNCHS (Habitat), 1986. The design of shallow sewer
systems. UNCHS (Habitat), PO Box 30030, Nairobi, Kenya.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 49 June 1992
 7 Page 8 7 Page 8
Refrigerated SSS? In teaching mothers about how to prepare home made salt and sugar solution, I advise
them to throw it away after 24 hours to avoid contamination during storage. Some of them
ask whether keeping the solution in the fridge would enable them to use it over a period
of a few days. Is there any harm in doing this, and how long can SSS be stored in a
fridge? Saliso Sando, Environmental Health Officer, Ministry of Health, Katsina State,
Nigeria.
Dr Nate Pierce, CDD/WHO, replies: When SSS is kept at room temperature in warm climates it tends to spoil after 24 hours
because of bacterial growth in the solution. Normally, any solution not used within 24
hours should be discarded and a fresh solution made. If the solution is kept in a fridge
it will last longer, at least two days. It should not be necessary to keep the fluid
longer than two days as the amount prepared, usually one litre or less, would be used up
within this time.
Treating cholera There was a cholera epidemic in part of Nigeria last year. At the hospital where I
work, most of the patients were prescribed tetracycline and
phthalysulphathiazole,
together with (mist) kaolin. Do you think this combination of antibiotics is necessary, as
in most cases the cholera vibrio is sensitive to tetracycline? There was also little or no
reduction in stool quantity in the patients treated with kaolin. Oleyede Oyegbade, PO Box 367, Osogbo, Osun State, Nigeria.
Dr William Cutting replies: Phthalysulphathiazole is a poorly absorbed sulphonamide, and can have toxic side
effects. Studies have shown that the drug has no effect on cholera vibrio excretion.
Tetracycline is one of the recommended drugs of choice for treating cholera, and should be
given without other antibiotics. Clinical trials have shown that giving kaolin does not result in fewer stools or less
fluid loss. The stools may look less watery, because the kaolin itself absorbs
fluids in the gut, but it does not stop fluid loss from the body. As Mr Oyegbade points
out, giving kaolin to cholera patients is of no benefit. Rehydration therapy is the most
important part of treatment for cholera. An appropriate antibiotic, such as tetracycline,
is helpful because it shortens the illness and reduces stool losses.
|
Future issues ...
DD50 will focus on training issues. DD51
will review evaluation of CDD activities. We would like to include
readers' experiences and examples of what has worked and why, as well as
what has not worked so well! Please send contributions for issue 51 by 13
September.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Assistant editor Nel Druce
Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Nicole Guérin (France)
Dr Norbert Hirschhorn (USA)
Dr Sharon Huttly (UK)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Dang Due Trach (Vietnam)
Professor Andrew Tomkins (UK)
With support from AID (USA), ODA (UK), UNICEF, WHO
Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 49 June 1992
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
updated: 23 April, 2014
|