|
| |
Issue no. 33 - June 1988
pdf  version
of this Issue version
of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 33 - June
1988
|
DDOnline
Dialogue
on Diarrhoea Online Issue 33 June 1988  Page 1 2
Page 1 2
Child survival - a universal concern
Concern today must be with more than the difference between life and death for children
born in circumstances of poverty and deprivation. These children need not just to survive
but also the chance to grow up healthy in both body and mind. It is the children of today
who will be responsible for the world of tomorrow. Importance of education
 |
The parents of tomorrow - early education can establish healthy
habits for life.
Education is of paramount importance in influencing later hygiene and health behaviour.
More than 1,300 schoolchildren from Europe, Asia, Africa and the Pacific region entered
our poster competition. This excellent response shows how widely the causes of diarrhoea
and the place for ORT in treating it are coming to be understood by the parents of the
future.
|
The judges had a difficult task in choosing from so many good pictures. Thanks to the
generous sponsors we will be able to send something to all entrants as well as the winners
listed in the="su33.htm">insert with this issue. ORT - lifesaver but not a cure
There is no doubt that promotion of oral rehydration therapy has already saved the
lives of many children, but it should be remembered that ORT does not prevent the problem
of diarrhoea itself. Recent Dialogues have highlighted the importance of other
measures to prevent diarrhoea such as immunisation against other infectious diseases like
measles and the need to promote breastfeeding and good weaning practices. The possibility
that vitamin A reduces the risk and severity of diarrhoea is discussed on="#page4">pages
4 and 5. In many places promotion of ORT should continue and extend. Nurses can play a key role
in all countries in spreading the message about ORT and ways to prevent diarrhoea. Page 6 of this issue shows how nurses in a hospital setting in the U.K.
work with parents to manage diarrhoea using ORT. There is still no easy answer to the diarrhoea problem, but there are many ways in
which people can help to protect their families. There are two pages of letters from
readers in this issue; writing to DD is just one way to share ideas about what
people can do about diarrhoea. KME and WAMC
|
In this issue ...
- Vitamin A and diarrhoea update
- Children's Poster Competition results
- Nurses and ORT in the U.K.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 33 June 1988
 1 Page 2 3 1 Page 2 3
Iran: attitudes to treatment and use of antibiotics
Until recently, use of intravenous fluids has been a common practice in Iran. People
have accepted it as a routine treatment and have often demanded it, not only for diarrhoea
and vomiting, but also for headaches, tiredness etc. Doctors' attitudes
Many doctors use ORS only to prevent dehydration or during the maintenance phase of
rehydration therapy. Any dehydration is usually treated by IV fluids. Paediatricians,
although well aware of ORT, do not always practise it without also using IV therapy. The
government of Iran has started a popular campaign to promote ORT and is training health
workers in this field. In my opinion, some doctors, who graduated during the 1970's or
earlier, may also need a special re-orientation course because they can change people's
attitudes effectively. ORS packets are available at reasonably low cost. Unfortunately, as in other parts of
the world, antibiotics and antimotility agents are very much overused despite a campaign
by the Ministry of Health. Aetiology and antibiotics
In North Iran, we have conducted a study of children admitted to hospital with
diarrhoea. This year, of the first one hundred cases analysed, 90 per cent had received
unsuccessful treatment before admission with a variety of drugs, including antibiotics and
antimotility agents. Without facilities for identification and culture of viruses and campylobacter,
definite aetiology could be established in only 38 per cent of cases; another 15 per cent
(classified as parenteral diarrhoea) were associated with definite infection elsewhere
(UTI, septicaemia, otitis, pneumonia etc.). Salmonella was found in 16 per cent of the
stool cultures, 13 per cent showed pathogenic E. coli, eight per cent had Giardia
lamblia and one per cent Entamoeba histolytica. The significance of the initial
results of the study (which is still in progress) is not only the previously unreported
high incidence of Salmonella infection, but also the alarming level of drug resistance. To
our surprise, all Salmonella cultures were resistant to ampicillin, 45 per cent were
resistant to both ampicillin and chloramphenicol, and 38 per cent to chloramphenicol and
co-trimoxazole. Similarly, all pathogenic E. coli cultures were resistant to
ampicillin, 62 per cent were resistant to both ampicillin and co-trimoxazole, and 31 per
cent were resistant to both ampicillin and gentamycine. While ORT has been proved to be a simple, effective and inexpensive treatment for
diarrhoea, there are many socio-cultural barriers to be overcome before it becomes popular
and more widely used. Dr R. C. Bhardwa is currently working in Iran.
The Editors would like to hear from other readers who have investigated antibiotic
resistance. Leaf concentrate consumption and diarrhoea
Given that leaf concentrate is one of the richest known natural sources of B-carotene
(pro-vitamin A), its consumption may help to minimise the risk of diarrhoea. This has been
reported by mothers in Find Your Feet's Mexican project, who stated that once their
children started eating leaf concentrate routinely, they had fewer episodes of diarrhoea. A number of studies have also shown that episodes of diarrhoea are less severe and less
prolonged in well-nourished children. Regular consumption of leaf concentrate by children
could thus be expected to ameliorate the effects of diarrhoea. Treatment
As far as is known, leaf concentrate has not been added to ORT solutions or fed with
them. One study, however, reports that feeding cooked pureed amaranthus leaves along with
the standard ORT solution brought about a remarkable improvement in children treated with
this mixture, attributed to the B-carotene in the amaranthus. If this is verified in
further studies, it could be expected that leaf concentrate (LC) would also be effective. Potassium is frequently missing from home-made ORS solutions. To overcome this
deficiency, it has been suggested that bananas be fed to children with diarrhoea. LC could
also be effective since it contains almost as much potassium as bananas (320mg per 100g of
LC versus 370mg per 100g of bananas). Counteracting the effects
When a child has diarrhoea there may be a reduction in food intake and nutrient
absorption lasting for a week or more, and resulting in faltering growth. Extra nutrients
are needed for catch up growth: including an additional 10 to 15 grams of protein a day,
for several weeks. Since leaf concentrate curd contains 25 to 30 per cent protein, its
consumption during the post-diarrhoeal period may be recommended. It is soft and easily
digested and can be taken before the diarrhoeal episode is completely over. Walter J Bray, c/o Find Your Feet (UK) Ltd, 13-15 Frognal, London NW3.
For further information please contact the author. Using ORS packets to measure water volume?
An accurately measured volume of water is important in preparing solution using ORS
packets and in making sugar-salt solution. Programmes usually try to ensure this by:
- promoting the use of a commonly used and widely available 'standard' container;
- careful instruction of mothers and other users in how to measure a litre (or other
volume) using a container which they have at home; or
- distribution of containers of standard size such as jars, cups, plastic bags to
potential users.
All these methods require training and possibly the cost of producing and distributing
a special container.
|
Why not use the
ORS packet as a standard unit to measure the volume of water needed? Packets are usually
made from water-resistant material and are sealed by the manufacturer to a standard size. At the Hospital General de Oxapampa in the high central jungle area of Peru, we studied
the ability of twelve mothers to use ORS packets to measure the correct volume of water.
The mothers, who were mostly from poor homes, all came with children who had acute
diarrhoea.
|
 |
After careful instruction they each tried to measure a litre of water four times and
the volumes were all between 882 and 1058 cc (1). If ORS packets were designed with
measurement in mind, this might be a feasible method for measuring the water when
preparing ORS solution with no additional cost (2). Dr O J Chang, currently at the London School of Hygiene and Tropical Medicine,
Keppel Street, London WC1E 7HT, UK. Editors' notes
1. At 882cc the sodium concentration would exceed 100 mmol/l which is higher than
the recommended concentration of sodium. 2. This is one way of measuring a fluid volume, although as a method it has some
weaknesses. Its practicability would depend on the local situation. At what level and how
neatly it is opened will affect the volume of the empty packet. One concern is that
multiple filling of the packet, presumably by dipping it, and difficulty in handling it,
may result in greater contamination of ORS solution from the hands and environment than
using a larger, more stable container. More operational research of this type in
developing countries would be very useful. Readers are invited to send in comments from
their own experience.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 33 June 1988
 2 Page 3 4 2 Page 3 4
IDD newsletter
The most common result of iodine deficiency is goitre - a swelling in the neck caused
by an enlarged thyroid gland. Children of iodine deficient mothers can be affected by
severe physical and mental retardation, and cretinism. Approximately 800 million people
are living in areas where they are at risk from IDD although it is most common in inland
mountain countries of the Himalayas and the Andes, Indonesia, Malaysia and many African
countries are also affected. The Iodine Deficiency Disorders (IDD) newsletter covers all aspects of prevention and
control of this important disease. Recent articles include community education programmes,
discussion of disease and nutrition, and reports of iodinated salt distribution in
Bangladesh, Java and Brazil. The journal is quarterly and available free of charge to
readers in developing countries from Dr J. T. Dunn, Editor, IDD Newsletter, Box 511, University of Virginia Medical
Center, Charlottesville, VA 22908. USA. Note for readers
Please include your mailing list number (printed on the address label) when
writing to DD. This will help us to answer your requests as quickly as
possible. ORS flavouring and colouring: follow-up
DD32 reported on the possible advantages and
disadvantages of using flavoured or coloured ORS compositions. Recent evidence from
Pakistan (1) shows the importance of ensuring that using flavoured ORS does not lead to
over-consumption, and consequent hypernatremia. A study showed that flavoured and
unflavoured ORS were equally acceptable during the initial rehydration period. During the
maintenance period, however, when taste rather than thirst is more likely to influence
fluid intake, flavoured solution was preferred and hence consumed in greater quantities. 1. Nayyar, G., et al., 1987 Comparative clinical trial of acceptability of flavoured
vs non-flavoured ORS (WHO formula). J.P.M. A July: 167-170. AHRTAG's resource centre
The resource centre at AHRTAG is a focus for the exchange of information on primary
health care and appropriate health technologies. The following resource lists are available:
- Health education on diarrhoeal diseases - manuals, bibliographies, health
education materials, journals and audiovisuals about diarrhoeal diseases. Also includes a
list of international resource centres. Cost: £0.50 (free to developing countries).
- French health education materials and information - organisations in Africa,
Europe and North America which produce French language health education materials. Cost:
£0.50 (free to developing countries).
- Spanish health education materials and information -
organisations in Latin America, Europe and North America which produce Spanish language
health education materials. Cost: £0.50 (free to developing countries).
- Community assessment and evaluation - currently available publications and
articles, where to get them and prices. Cost: £0.50 (free to developing countries).
- Free international newsletters - a comprehensive list of 73 free international
newsletters on health and development. Each is listed by address, frequency of
publication, language and a brief description of the contents. A subject index is also
included. Cost: £0.75 (free to developing countries).
- Directory of primary health care courses in the U. K. (under 6 months) and Directory
of primary health care courses in the U. K. (6 months - 2 years). Both directories
include a comprehensive list of courses held in the U. K. on primary health care and
related topics. Each entry includes where the course is held, dates, duration, number of
places for students, fees, entry requirements, and a curriculum outline. The courses are
indexed by subject and city. Cost of each directory: £3.50.
Resource lists available from Resource Centre, AHRTAG,
|
DDOnline
Dialogue
on Diarrhoea Online Issue 33 June 1988
 3 Page 4 5 3 Page 4 5
Reducing the risk?
Vitamin A is an essential nutrient, especially in preventing eye diseases. Can it
also help to prevent diarrhoea and other infections? Andre Briend
discusses the latest evidence. Xerophthalmia is the term used to describe the eye diseases caused by a deficiency of
Vitamin A. Symptoms range from difficulties in seeing in poor light to severe damage to
the cornea which can result in blindness (1). The main objective of current programmes
distributing capsules of vitamin A is to prevent blindness due to xerophthalmia. There is
no doubt that these programmes are effective for that purpose, and that malnourished
children with diarrhoea who are especially at risk of going blind benefit from them. Vitamin A affects the health of the eye because of its role in the growth and
development of epithelial cells. The gut is also lined with epithelial cells and so it
seems reasonable to suppose that a deficiency of vitamin A might increase susceptibility
to diarrhoeal disease. Some studies also suggest that vitamin A deficiency may reduce the
effectiveness of the immune system, which would also increase the risk of diarrhoea. The
evidence for such an effect is still very limited but deserves careful consideration. Many factors involved
A link between mild vitamin A deficiency and an increased risk of diarrhoea has been
suggested by studies in Indonesia. The first study found that children with symptoms of
xerophthalmia had more attacks of respiratory disease and diarrhoea, and that more
children died in this group than in a similar group of children without xerophthalmia
(2)(3). Explaining these findings is difficult because many other factors could have been
involved that were not studied or known, and so it is not possible to state confidently
that vitamin A deficiency caused this effect.
|
Breastfeeding reduces the risk of diarrhoea and other infections.
For example, stopping breastfeeding at an early age is a factor associated with
increased risk of diarrhoea, xerophthalmia and death (4) (5). Also, a history of repeated
attacks of diarrhoea increases the chances of further attacks and of vitamin A deficiency.
It has also been suggested that these findings could be explained by differences in
nutritional status.
|
 |
Significant differences?
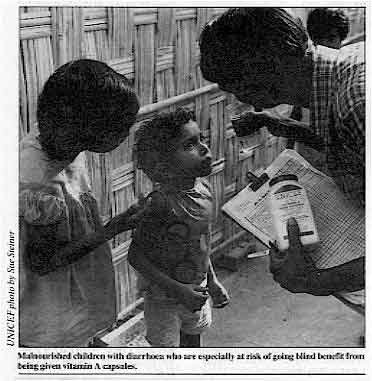 |
Malnourished children with diarrhoea who are especially at risk
of going blind benefit from being given vitamin A capsules.
In an attempt to confirm their initial findings, the same researchers in Indonesia
carried out another study. This study examined the effect of providing vitamin A capsules
every six months to children in randomly selected villages, and comparing them with
children in other (control) villages who did not receive vitamin A supplements(6).
|
The results show significant differences, but there is some evidence that the
experimental and control villages were not exactly alike in some important respects(7).
The authors' claim, that the intervention reduced child mortality by as much as 34 per
cent, should therefore be treated with some caution. In addition. the report did not
mention what caused the deaths of children, so it was not possible to check that deaths
due to diarrhoea were reduced in the group of children who received vitamin A supplements.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 33 June 1988
 4 Page 5 6 4 Page 5 6
No conclusive evidence yet
A more recent study conducted in India (8)' using methods very similar to the first
Indonesian study failed to find an association between xerophthalmia and the incidence of
diarrhoea (although it did report an increased frequency of respiratory diseases
associated with xerophthalmia). The preliminary findings of several current studies at the
International Centre for Diarrhoeal Diseases Research, Bangladesh (lCDDR, B) also do not
support the theory that the incidence of diarrhoea can be reduced by the provision of
vitamin A supplements. In summary, there is no conclusive evidence yet that vitamin A supplements can be used
to control diarrhoeal diseases. No definite statements can be made at this stage, however,
because few studies have investigated this issue. None have looked at the effect of
vitamin A status on the duration of diarrhoea or on the occurrence of complications,
although the possibility of some effect on these is plausible. More research is needed
before any benefits of vitamin A, in addition to its ocular effects, can be confirmed*. Andre Briend, MD, Nutritionist, International Centre for Diarrhoeal Diseases
Research, Bangladesh, GPO Box 128, Dhaka 2, Bangladesh.
* WHO/CDD is interested in supporting such research. References
1. Sommer, A., 1982. Nutritional blindness: xerophthalmia and keratomalacia.
Oxford University Press.
2. Sommer, A., et al., 1984. Increased risk of respiratory disease and diarrhoea in
children with pre-existing mild vitamin A deficiency. Am. J. Clin. Nut. 40: I090-1095.
3. Sommer, A., et al., 1983. Increased mortality in children with mild vitamin
deficiency. Lancet 2 (Sept. 10): 585-588.
4. Tarwotjo, I., et al., 1982. Dietary practices and xerophthalmia among Indonesian
children. Am. J. Clin. Nutr. 35: 574-58.
5. Briend, A., et al., (in press). Breastfeeding, nutritional status and survival in
rural Bangladesh. Br. Med. J.
6. Sommer, A. et al., 1986. Impact of vitamin A supplementation on childhood
mortality. Lancet 1 (May 24): 1169-1173.
7. Feachem, R. G., 1987 Vitamin A deficiency and diarrhoea: a
review of inter-relationships and their implications for the control of xerophthalmia and
diarrhoea. Trop. Dis. Bull. 84: R1-R1.
8. (No author) 1987 Mild vitamin A deficiency and childhood morbidity - an Indian
experience. Am. J. Clin. Nutr. , 46: 827-829. Note
The="#Feachem">article listed as reference 7 above (Feachem, 1987) is a
recommended source for further information on Vitamin A deficiency and diarrhoea. The
evidence for links between vitamin A deficiency and diarrhoea are discussed and areas
where further research is needed are highlighted. Four possible reasons for giving vitamin A to children with diarrhoea are identified:
- to contribute to the control of vitamin A deficiency in the community;
- to prevent future xerophthalmia in children with diarrhoea;
- to help with a current attack of diarrhoea; and
- to reduce the risk of future attacks.
The review includes a warning that it is possible to give dangerously large doses of
Vitamin A. Readers who would like to know more about these studies should write to Dr Briend at
the ICDDR, B.
News and information about Vitamin A
The International Vitamin A Consultative Group (IVACG) met in December 1987 in
Addis Ababa, Ethiopia to discuss the development and use of integrated operational
programmes to combat vitamin A deficiency, particularly in Africa. Further information
from: IVACG Secretariat, The Nutrition Foundation Inc., 1126 Sixteenth Street, N. W,
Washington D.C. 20036, U.S.A.
Assignment Children: a new book published by UNICEF on Vitamin A deficiency and
xerophthalmia. Susan Eastman reports on recent research covering all aspects of this
subject, from recommended daily allowances of Vitamin A to links with diarrhoea and
nutrition. Available from UNICEF Programme Division, UNICEF House, 3 United Nations
Plaza, New York, N.Y 10017, U.S.A. Price: US$3.00
The Xerophthalmia Club Bulletin: an eight page newsletter which reports on
current developments in the control and prevention of nutritional eye diseases.
Appropriate methods and primary health care are stressed. Available free of charge to
those interested in xerophthalmia from Dr D. S. McLaren, Club Secretary, Department of
Medicine, The Royal Infirmary, Edinburgh EH3 9YW, U.K.
Supercarrot: a new type of carrot with ten times the normal amount of carotene
(which the body converts to vitamin A) has been developed by the U.S. Department of
Agriculture. Vitamin A deficiency increases the risk of diarrhoeal disease, malnutrition
and eye disease, and causes blindness in severe cases. Field tests are being carried out
in south Asia and central Africa. Further information is available from the Agricultural
Research Service, Department of Horticulture, 1575 Linden Drive, University of Wisconsin,
Madison, WI 53706, U.S.A.
|
|
DDOnline
Dialogue
on Diarrhoea Online Issue 33 June 1988
 5 Page 6 7 5 Page 6 7
A nursing perspective
Oral rehydration therapy to treat dehydration from diarrhoea is safer and cheaper
than other methods, and is equally valuable in developed and developing countries. Nurses
and parents can play a key role. Christine Candy reports from
the U. K. The first step in the treatment of diarrhoea is to recognise that it is the loss of
fluids and electrolytes (salts) from the body that is potentially dangerous and that
replacement of these losses by oral rehydration allows the patient to recover. The role of nurses
 |
A
nurse gives ORS at the Birmingham Children's Hospital. The use of oral rehydration can lead to greater involvement of nurses and parents in
the management of children with diarrhoea. The majority of children with diarrhoea
attending the Children's Hospital, Birmingham (U. K.) are treated in the Accident and
Emergency Department. In most acute cases, initial assessment by the medical staff is
followed by management by nursing staff. An important change in policy is that nurses only
refer the patient for further assessment if they are in doubt about the child's progress
after being given preliminary ORT. Now, in addition to their previous responsibilities,
trained nursing staff take the case history, prescribe fluid requirements, and teach
parents to rehydrate their child by mouth.
|
Follow-up
The next day parents attend a follow-up clinic with their child, and the nurse assesses
the success of the treatment. This assessment is based on:
- weight change;
- frequency of vomiting and diarrhoea;
- whether the child is drinking eagerly; and
- the volume of solution that has been drunk.
If the child is recovering, the nurse encourages continuing feeding with drinks and a
normal diet and makes sure that parents understand what they need to do. Nursing staff
then follow the child's progress, and discharge him/her when the diarrhoea has stopped and
weight is being gained. Advantages of ORT
ORT is simple, safe, and cheap. Any nurse who has had to start an intravenous drip in a
frightened child will soon realise that ORT is a much more pleasant alternative. It is
surely preferable to sit cuddling a child while encouraging him or her to take small sips
of fluid.
|
Using oral rehydration parents can be actively involved in treatment.
Oral rehydration is also less alarming to parents. They can be actively involved in
giving the treatment. The child is more mobile when not attached to a drip, and there is
no anxiety that the tube may be displaced. The child does not have a dry mouth and can be
encouraged to eat normally. Although this method of rehydration is more labour-intensive,
the time taken for rehydration and recovery is less. If nursing staff shortage is a
problem, and parents are not available, then a nasogastric tube can be passed. Giving
fluid in this way may be preferable to the pain of intravenous infusions (see DD26).
|
 |
Using ORT, paediatric nurses, in partnership with parents, can treat greater numbers of
children suffering from this life-threatening condition. Using ORT also means less
discomfort and weight loss for children, less parental anxiety, decreased length of
hospital stay. and financial savings. Christine Candy, Paediatric Nurse Tutor Queen Elizabeth School of Nursing, Medical
Centre, Edgbaston, Birmingham B15 2TH, U.K.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 33 June 1988
 6 Page 7 8 6 Page 7 8
Drugs for diarrhoea?
I would like to present a problem facing us in treating cases of diarrhoea. Sometimes
the parents and relatives of patients are too worried and agitated to wait for a period of
several days for diarrhoea to stop, when oral rehydration therapy alone is used. To them,
diarrhoea and not dehydration is the major problem. Because of this, doctors may find
themselves obliged to prescribe anti-diarrhoeal drugs and sometimes antibiotics, or the
patient will seek another doctor's advice or buy the drugs directly from a pharmacist. If you can throw any light on the role, if any, of anti-diarrhoeals and antibiotics in
the treatment of diarrhoea, and how to determine a bacterial aetiology for diarrhoea in
the absence of laboratory facilities, I will be thankful. Dr Sharif Salry Nassif, 10 Gamal El Dien Street, Tanta, Egypt. Editors' note:
Anti-diarrhoeal drugs are mostly inappropriate, ineffective and sometimes dangerous for
young children. The role of drugs, including antimicrobial, antimotility, antisecretory
and other drugs, in the treatment of diarrhoeal diseases was covered in="dd25.htm">DD
issue 25. A forthcoming issue of DD will suggest how to determine bacterial
aetiology for diarrhoea in the absence of laboratory facilities. Drinking water storage
I have read your practical advice item on water purification in DD30.
I congratulate you on publishing this useful information which is not given in most
community medicine textbooks. In Karachi, water is purified by rapid sand filters, then chlorinated and tested in
laboratories on site before distribution to the various parts of the city. In different
multi-storey buildings, water is pumped from underground storage tanks to roof tanks from
where it is piped to individual flats. In old Karachi, the water tanks are very old and
contaminated and need frequent cleaning. Some tanks are made of cement and some are metal.
Will you please mention some practical methods for cleaning these tanks and for purifying
the water inside them. Dr Zubair Ahmad, A-1/I, Maymarr Terrace, Block-2, Gulshan-e-Iqbal, Karachi,
Pakistan. Editors' note: See future issues. Welcome DD in Bengali
Allow me to congratulate you on the decision you have taken to bring out DD in
my mother tongue, Bengali. Bengali is very widely spoken (by 160 million people). It is
the language of Bangladesh, and of the West Bengal and Tripura Indian provinces, and is
also spoken by many people in the Bihar, Orissa and Assam provinces of India, as well as
by many from Bangladesh in the U. K. and the Middle East. It goes without saying that the
success of any journal like DD depends on the understanding of it by the readers so
that they can make changes to their daily lives. Viva DD Bengali - 'Udaramoy
Shanglap'. Dr A. H. Hafizzuddin Ahmed, PO. Box 32441, Augla (Via Agedabia), Libya. Giving oral polio vaccine
Your Immunisation supplement in="dd30.htm">DD issue 30 was quite
informative. However, I should like some clarification: you had a photograph showing a
health worker giving OPV to a child in Colombia, and she was using a teaspoon. I would
like to know if there are any vaccine preparations that can or should be given by
teaspoon, and whether this method would be more effective than dropping the OPV straight
into the child's mouth. If the vaccine is spoon-fed there is a chance that it will not all
be licked up by the child, and besides, it adds more time and logistics to provide a
spoon. Or perhaps giving vaccine by spoon is more culturally appropriate? At ICM we provide medical services for refugees and we follow US CDC standards, so
necessarily immunisation schedules and preparations are different from the EPI. Thank you
very much and more power to your organisation. Dr Vic S. Salas, Medical Co-ordinator, Intergovernmental Committee for Migration,
Mission in the Philippines, 2nd floor, Victoria Building, 429 United Nations Avenue,
Ermita, Manila, Philippines. Dr N. Hirschhorn of Resources for Child Health (REACH) replies:
WHO recommends that vaccinators use the dropper supplied with the vial of oral polio
vaccine (OPV). This is the most direct and effective way to deliver the correct drop size.
Tilt the child's head back and gently squeeze the cheeks or pinch the nose to make the
mouth open. Let the drop fall from the dropper onto the child's tongue. Repeat the process
if the child spits out the vaccine. Because the vaccine can be bitter, some OPV
manufacturers suggest, especially for older children, that the drops be put in a cup of
distilled water or onto a sugar cube, or on a disposable plastic spoon with syrup. These
methods are, however, not always possible. Where the photo is really misleading is in
showing an older child receiving OPV We must stress the necessity to immunise children
against polio before their first birthday. Preventing neonatal tetanus
Regarding the Health Basics="su30.htm">Immunisation Insert (in Issue 30),
this information package has been really well thought out and put together in a very
readable form to help people to use the information in a practical way. However, it is not quite true to say that "hygienic cord treatment can also
prevent neonatal tetanus but is not as effective as complete immunisation of the
mother". Hygienic cord treatment prevents neonatal tetanus 100 per cent. The problem
is to ensure that all contact with the cord is, indeed, clean. Clean cord care usually
goes hand in hand with clean delivery care, and therefore the advantages of hygienic
practices include not only the elimination or reduction of neonatal tetanus, but also of
post-partum and cord infections. The TBAs who work with the Refugee Health Unit (RHU) in Somalia are trained to use
hygienic delivery and cord care practices with extremely good results. RHU can count on
two hands the number of cases of neonatal tetanus in the last two years in a population of
800,000 and with 25,695 births (8 neonatal tetanus cases). The effectiveness of hygienic
cord care is in no doubt. The problem, as with immunisation, is in ensuring 100 per cent
use of the chosen method. Una MacAskiII, Refugee Health Unit, Box 2925, Mogadishu, Somalia. Dr Hirschhorn: Ms MacAskill is correct, hygienic cord treatment is 100 per cent
effective if it can be ensured.
|
DDOnline
Dialogue
on Diarrhoea Online Issue 33 June 1988
 7 Page 8 7 Page 8
Teaching with DD
The Medical Centre of the Federal Polytechnic, Bida, is a clinic which caters for
students and staff of the polytechnic, and their immediate families (about 3,500 people in
total). With the introduction of the primary health care programme in Nigeria, we now have
an EPI/ORT unit in the clinic which is free to other members of the community. We also
have outreach programmes to surrounding villages to give vaccinations and nutritional
advice. It was initially difficult to get members of the Health Team to stop giving
anti-diarrhoeal drugs and use ORS instead, until we started holding clinical sessions to
go through copies of DD and discuss issues raised. It has now been fully
accepted that drugs are not necessary and a lot of village mothers are now being taught to
prepare their own ORS. Dr C. Gana, Medical Centre, The Federal Polytechnic, P. M. B. 55, Bida, Niger State,
Nigeria. Public latrines
Regarding the letter from Ms Carrie Osborne (DD31) -
our small township of Tatkon (population 180,000) has launched a campaign to build
fly-proof latrines; one third of the township has now been covered within a year. The
market place is the centre of activity in the town, but, until recently, had no proper
sanitary facilities. The old latrines were filthy and smelt unpleasant. After discussion
with local municipal officials our Township Health Team removed all the insanitary pit
latrines and installed pour-flush fly-proof latrines instead. Attendants hired by the
authorities refill the water pots (there is no running water in the town) and do the
cleaning. Customers are charged a small fee which goes towards the maintenance of the
latrines and the salaries of the attendants. Everybody is happy and our market place is free from obnoxious smells and filthy
sights, creating a positive health effect on the surrounding area. Villagers who have used
the new latrines are now keen to install fly-proof latrines in their villages as well. So
we are practically selling health in our market place! Myint Oo, Health Assistant, Myaukmyaik RHC, Tatkon Township, Burma. Living with disease - urban slums
Greetings from Lagos city! The population density here is 5,000 to 7,000 persons per
square kilometre. During the wet season, when it rains all day and all night, everything
overflows - drains, pits, wells, latrines. The result is an increase in cholera, typhoid,
other diarrhoeal diseases and acute respiratory infections. This puts an unbearable burden
on an already inadequate health service. I have started a programme of self-reliance
health schemes at ten community centres in Lagos, but positive development is difficult
without the co-operation of landlords to improve water, sanitation and drainage
facilities. The issues covered in DD relating to urban conditions are most
useful - especially the material on diarrhoea in urban slums (in="dd31.htm">issue
31). Sister Brigid Kennedy, SRM, DYM, Medical Missionaries of Mary, PMB 21294, Ikeja,
Nigeria. Water purification
I read with interest your article on "water purification" in="dd30.htm">DD issue 30. I would like to question your advice to
keep water boiling for ten minutes in order to destroy germs. Recently, I was informed by
WHO/CDD that it would be enough to bring water to the boil! It is very confusing for
people to receive different information from different sources. Can you help? In your article you also asked for other methods of water purification. I worked in
Botswana from 1983 to 1985 as the co-ordinator of a National Water Hygiene Campaign. The
Department of Water Affairs started a study of storage of water in the sun. We used 15
litre black plastic containers, kept them in the sun for a day and achieved a reduction of
bacteria of around 95 per cent (and we used very contaminated water for some of the
samples). Unfortunately, we could not finalise the study and find out exactly how many
hours of sun was needed or if the method was applicable also during the winter. But the
preliminary results were interesting and I would like to know if other people have carried
out similar research. In the campaign we used clean water from standpipes to show people how to keep water
clean at home. We found that the most effective method was to use 15 litre plastic
containers with a small opening and a lid both for fetching water and for storage
(especially drinking water). This way people could not put dirty hands and dippers into
the water and it stayed uncontaminated. Marianne Enge, Technical Advisor Health Education and Information, League of Red
Cross and Red Crescent Societies, Community Health Department, PO. Box 372, 1211 Geneva
19, Switzerland. Editors' note: Bringing water to the boil will kill most microbial pathogens.
Longer boiling is safer, but more expensive and time consuming.
|
| In the next issue.. . Diarrhoeal disease control activities have
achieved a great deal in many places but there are still problems to resolve. DD34 will include an overview of the CDD programmes of
agencies such as WHO, UNICEF and USAID, and individual country reports. Comments from
readers about their own CDD activities would be welcome.
|

Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 33 June 1988
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
updated: 23 August, 2019
|